Area for Tuberculosis Control
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Social Audit Report: Part II
Detailed reports of the 62 villages 1 | Social Audit Report: Part II Detailed reports of the 62 villages SOCIAL AUDIT REPORT PART II: DETAILED REPORTS November 2016 2 | Social Audit Report: Part II Detailed reports of the 62 villages Contents 1. Ariyalur District ............................................................................................................................... 6 1.1 Sendurai village, Sendurai block, Ariyalur District ........................................................................ 6 1.2 Viluppanankurichi village, Thirumanur block, Ariyalur District .................................................... 8 1. Coimbatore district ....................................................................................................................... 10 2.1 Periyapodu Village, Anaimalai Block, Coimbatore District ......................................................... 10 2.2 Nachipalayam Village, Madukkarai Block, Coimbatore District .................................................. 13 2.3 Puliyampatti village, Palladam block, Coimbatore district ......................................................... 16 3. Cuddalore district .......................................................................................................................... 20 3.1 Nedunkulam village, Mangalore block, Cuddalore ..................................................................... 20 3.2 T.V.Puthur village, Viruthachalam block, Cuddalore ............................................................ 21 4. Dharmapuri -
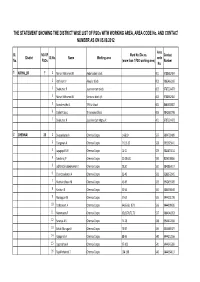
Dos-Fsos -District Wise List
THE STATEMENT SHOWING THE DISTRICT WISE LIST OF FSOs WITH WORKING AREA, AREA CODE No. AND CONTACT NUMBER AS ON 05.09.2012 Area Sl. NO.OF Ward No./Div.no. Contact District Sl.No. Name Working area code No. FSOs (more than 1 FSO working area) Number No. 1 ARIYALUR 7 1 Nainar Mohamed.M Andimadam block 001 9788682404 2 Rathinam.V Ariyalur block 002 9865463269 3 Sivakumar.P Jayankondam block 003 9787224473 4 Nainar Mohamed.M Sendurai block i/c 004 9788682404 5 Savadamuthu.S T.Palur block 005 8681920807 6 Stalin Prabu.L Thirumanur block 006 9842387798 7 Sivakumar.P Jayankondam Mpty i/c 401 9787224473 2 CHENNAI 25 1 Sivasankaran.A Chennai Corpn. 1-6&10 527 9894728409 2 Elangovan.A Chennai Corpn. 7-9,11-13 528 9952925641 3 Jayagopal.N.H Chennai Corpn. 14-21 529 9841453114 4 Sundarraj.P Chennai Corpn. 22-28 &31 530 8056198866 5 JebharajShobanaKumar.K Chennai Corpn. 29,30 531 9840867617 6 Chandrasekaran.A Chennai Corpn. 32-40 532 9283372045 7 Muthukrishnan.M Chennai Corpn. 41-49 533 9942495309 8 Kasthuri.K Chennai Corpn. 50-56 534 9865390140 9 Mariappan.M Chennai Corpn. 57-63 535 9444231720 10 Sathasivam.A Chennai Corpn. 64,66-68 &71 536 9444909695 11 Manimaran.P Chennai Corpn. 65,69,70,72,73 537 9884048353 12 Saranya.A.S Chennai Corpn. 74-78 538 9944422060 13 Sakthi Murugan.K Chennai Corpn. 79-87 539 9445489477 14 Rajapandi.A Chennai Corpn. 88-96 540 9444212556 15 Loganathan.K Chennai Corpn. 97-103 541 9444245359 16 RajaMohamed.T Chennai Corpn. -

Introduction the Chennai Basin Group Rivers Are Situated Between
CHENNAI BASIN Introduction The Chennai basin group rivers are situated between latitudes 12o 30’ 00’’ to 13 o35’00’’ N and longitudes 79o15’00’’ to 80o22’30’’E and is located into the northern part of Tamil Nadu. The Chennai Basin Group of rivers is Araniar, Korattalaiyar or Kosasthalaiyar, Cooum and Adyar and small minor stream on the southern part of the basin. The Chennai basin comprises of 8 sub basins as shown in Plate:CHE-02. The northern part of Chennai basin is occupied by Andhra Pradesh and Pulicat lake, south and west by the Palar river basin and east by Bay of Bengal. The total geographical area of Chennai basin within Tamil Nadu is 6118.34 sq km totally. It covers in the Survey of India toposheets 57‘O’, 57 ‘P’, 66’C’, and 66 ‘D’ and it also covers in Chennai, Kancheepuram, Thiruvallur and Vellore districts. The administrative setup of the Chennai basin group is given below (Figure 1) Sl DISTRICT TALUK Sl BLOCK BLOCK/ARE No No A FALLING WITHIN THE BASIN AREA IN Sq Km 1. Kancheepura Thirukalunkundram 1 Thirukalukundram 71.60 m Tambaram 2 St. Thomas Mount 217.49 3 Thiruporur 411.82 Chengalpattu 4 Kattankulathur 158.83 5 Kancheepuram 10.14 Kancheepuram 6 Walajabad 73.27 7 Sriperumpudur 248.69 Sriperumpudur 8 Kundrathur 203.70 BLOCK/ARE A FALLING Sl Sl DISTRICT TALUK BLOCK WITHIN THE No No BASIN AREA IN Sq Km Gummidipoond Gummidipoondi 9 420.51 i 10 Minjur 478.69 Ponneri 11 Cholavaram 193.85 12 Puzhal 127.10 Ambattur 13 Villivakkam 210.61 Poonamallee 14 Poonamallee 178.33 2. -

List of Food Safety Officers
LIST OF FOOD SAFETY OFFICER State S.No Name of Food Safety Area of Operation Address Contact No. Email address Officer /District ANDAMAN & 1. Smti. Sangeeta Naseem South Andaman District Food Safety Office, 09434274484 [email protected] NICOBAR District Directorate of Health Service, G. m ISLANDS B. Pant Road, Port Blair-744101 2. Smti. K. Sahaya Baby South Andaman -do- 09474213356 [email protected] District 3. Shri. A. Khalid South Andaman -do- 09474238383 [email protected] District 4. Shri. R. V. Murugaraj South Andaman -do- 09434266560 [email protected] District m 5. Shri. Tahseen Ali South Andaman -do- 09474288888 [email protected] District 6. Shri. Abdul Shahid South Andaman -do- 09434288608 [email protected] District 7. Smti. Kusum Rai South Andaman -do- 09434271940 [email protected] District 8. Smti. S. Nisha South Andaman -do- 09434269494 [email protected] District 9. Shri. S. S. Santhosh South Andaman -do- 09474272373 [email protected] District 10. Smti. N. Rekha South Andaman -do- 09434267055 [email protected] District 11. Shri. NagoorMeeran North & Middle District Food Safety Unit, 09434260017 [email protected] Andaman District Lucknow, Mayabunder-744204 12. Shri. Abdul Aziz North & Middle -do- 09434299786 [email protected] Andaman District 13. Shri. K. Kumar North & Middle -do- 09434296087 kkumarbudha68@gmail. Andaman District com 14. Smti. Sareena Nadeem Nicobar District District Food Safety Unit, Office 09434288913 [email protected] of the Deputy Commissioner , m Car Nicobar ANDHRA 1. G.Prabhakara Rao, Division-I, O/o The Gazetted Food 7659045567 [email protected] PRDESH Food Safety Officer Srikakulam District Inspector, Kalinga Road, 2. K.Kurmanayakulu, Division-II, Srikakulam District, 7659045567 [email protected] LIST OF FOOD SAFETY OFFICER State S.No Name of Food Safety Area of Operation Address Contact No. -

Tiruvallur District Human Development Report 2017
TIRUVALLUR DISTRICT HUMAN DEVELOPMENT REPORT 2017 District Administration, Tiruvallur and State Planning Commission, Tamil Nadu in association with Hand in Hand India TIRUVALLUR DISTRICT HUMAN DEVELOPMENT REPORT 2017 District Administration, Tiruvallur, and State Planning Commission, Tamil Nadu in association with Hand in Hand India CONTENTS TitlePage No. Message by Member Secretary, State Planning Commission i Preface by District Collector ii Acknowledgements iii List of Boxes v List of Fgures vi List of Tables vi List of Annex Tables viii Chapter 1 District Profile 1 Chapter 2 Status of Human Development 13 Chapter 3 Employment, Income and Poverty 23 Chapter 4 Demography, Health and Nutrition 37 Chapter 5 Literacy and Education 61 Chapter 6 Gender 81 Chapter 7 Social Security 91 Chapter 8 Infrastructure 101 Chapter 9 Summary and Way Forward 115 ANNEXURES Tables 131 Technical notes 160 Abbreviations 166 References 171 E. Sundaravalli, I.A.S., Tiruvallur District District Collector Tiruvallur – 602 001 STD : (044) OFF : 27661600 RES : 27662233 FAX : 27662455 27.02.2017 PREFACE I acknowledge the efforts by the State Planning Commission and Hand in Hand India with the assistance from UNDP and the Government of Tamil Nadu towards the preparation of District Human Development Report and I am happy to be associated with this process. Present report portrays various facets of district’s development highlighting joint initiatives by the State Government and district administration to achieve sustainable human development. The report includes detailed discussions pertaining to key geographical, as well as sociocultural features of the district; the status of employment, poverty and economic growth; key health and nutritional parameters; literacy, status of school education and higher education and educational infrastructure; socioeconomic as well as political empowerment of women; social security for vulnerable population; and infrastructure options available to the people of the district etc. -

World Bank Document
INDIA GOVERNMENT OF TAMILNADU TAMILNADU IRRIGATED AGRICULTURE MODERNIZATION AND WATER RESOURCES MANAGEMENT ( TN IAM WARM) PROJECT III PHASE PROCUREMENT - PLAN FOR WRD SUB BASIN NAME:-ARANIYAR SUB BASIN DIVISION NAME:-ARANIYAR BASIN DIVISION CIRCLE NAME:-PALAR BASIN CIRCLE, Chennai (Package No. 1,2,3,4,6,8 & 12) & TM Circle Vellore Period of Contact: 18 Months (Package No’s 5,7,9,10 & 11) Public Disclosure Authorized Public Disclosure Authorized Sl.N Package Desrciption of ate of of ate o. No. Work Cost works Approval D Signing Number of Worksof informed) Estimated Method of to biddingto document Bank’s no- Bank’s Appraisal / / Appraisal & (Bank be to objection to ICB/NCB/FA Bank’s WBR (rs in Lakhs) in (rs Review Post Pre Review / Review Pre Evaluation & Procurement Preparation of Bit Documents contract award contract Contract award award Contract Revised / Actual / Revised ateCompletion of Date of Contract Contract of Date Bid Opening date Recommendation Recommendation Bid Invitation date Commencement of D Bank’s no objection 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 1 01/IAMWARM/ Rehabilitation and WRD/ANR/ modernisation of tanks in Appraisal 12.12.2009 NR 30.12.2009 04.02.2010 15.03.2010 NR 05.04.2010 NR 14.04.2010 13.10.2011 WORKS/III Poondi Block of Uthukottai 381.3 Post NCB Revised (2009-10) Taluk in Tiruvallur District Actual 2 02/IAMWARM/ Rehabilitation and Appraisal 12.12.2009 NR 30.12.2009 04.02.2010 15.03.2010 NR 05.04.2010 NR 14.04.2010 13.10.2011 WRD/ANR/ modernisation of tanks in WORKS/III Ellapuram Block of Uthukottai 457.71 -

Download (1MB)
A CROSS-SECTIONAL STUDY ON THE PREVALENCE OF EXCLUSIVE BREASTFEEDING PRACTICES AMONG THE IRULAR MOTHERS IN THIRUVALLUR DISTRICT, TAMILNADU 2011 Dissertation submitted to THE TAMILNADU DR. MGR MEDICAL UNIVERSITY In partial fulfillment of the requirements for the degree of M.D. BRANCH XV COMMUNITY MEDICINE THE TAMIL NADU Dr. MGR MEDICAL UNIVERSITY, CHENNAI, TAMILNADU. APRIL - 2012 CERTIFICATE This is to certify that the dissertation titled ‘A CROSS-SECTIONAL STUDY ON THE PREVALENCE OF EXCLUSIVE BREASTFEEDING PRACTICES AMONG THE IRULAR MOTHERS IN THIRUVALLUR DISTRICT, TAMILNADU, 2011’ is a bonafide work carried out by Dr. P. SARAVANAKUMAR, Post Graduate student in the Institute of Community Medicine, Madras Medical College, under my supervision and guidance towards partial fulfillment of the requirements for the degree of M.D. Branch XV Community Medicine and is being submitted to The Tamilnadu Dr.M.G.R. Medical University, Chennai. Dr.V.Kanagasabai, M.D., Dr.A.K.Rajendran, M.D., D.P.H., Dean, Director, Madras Medical College, Institute of Community Medicine, Chennai- 600 003. Chennai- 600 003. ACKNOWLEDGEMENT I gratefully acknowledge and sincerely thank Dr.V.Kanagasabai, M.D., the Dean, Madras Medical College, Chennai for granting me permission to carry out this community based study. I would like to express my sincere and profound gratitude to Dr.A.K.Rajendran, M.D., D.P.H., Director, Institute of Community Medicine, Madras Medical College, who has been a constant encouragement and perseverance which has helped me in the successful completion of this study. I am deeply indebted to Dr.V.V.Anantharaman, B.Sc., M.D., DPH., D.D, Assistant Professor, Institute of Community Medicine, Madras Medical College who has been the guiding force behind my study and helped me by extending his knowledge and experience during the course of this study. -

4. Fsos Details.Xlsx
Food Safety Officers Details as on 31.01.2020 Name of the FSO Mobile S.No. District Working Place Code FSO Number Andimadam Block & 1 Ariyalur Ponraj.A 001 Sendurai Block 7502221888 Ariyalur Block & 2 Ariyalur Vasanthan. E 002 municiplaity 9952116122 Justin 3 Ariyalur T.Palur Block 005 Amalraj.W 9790053064 4 Ariyalur Alaguvel.T Thirumanur Block 006 9865232120 Jayankondam 5 Ariyalur Sasikumar. S 401 Municipality & Block 9361222722 Chennai Corporation, 6 Chennai N.H. Jayagopal 527 Kodungaiyur 9841453114 Chennai Corporation, 7 Chennai 528 V. Jayavel Thandaiyarpet 9994237448 Chennai Corporation, 8 Chennai Selvam .R 529 Royapuram & Parrys 9444172751 Chennai Corporation, 9 Chennai Kannan .R 531 Sowcarpet 9444171585 Chennai Corporation, Pulianthope Jebaraja 10 Chennai Vacant 532 Shobana Kumar .K (i/c) Code No. 538 Chennai 11 Chennai V. Alagupandi 533 Corporation,Park Town 9790183187 P.Sundramoort Chennai Corporation, 12 Chennai 534 hy Ayanavaram 8122227055 Chennai Corporation, 13 Chennai Suthakar .V 535 Kolathur 7871555786 Chennai Corporation, 14 Chennai Ramaraj .A 536 Anna Nagar 9940067099 K. Chennai Corporation, 15 Chennai Shanmugasund 537 Koyambedu aram 9442030961 Jebaraja Chennai Corporation, 16 Chennai Shobana Choolaimedu & 538 Kumar .K Nungambakkam 9840348538 Chennai Corporation, 17 Chennai S. Baskaran 540 Ice House 9940920790 Chennai Corporation, 18 Chennai Raja .N 541 Periamet & Egmore 9994238989 Chennai Corporation, Manimurugan 19 Chennai Valluvarkottam & 543 .J Teynampet 9791141691 Senthil Chennai Corporation, 20 Chennai 545 Arumugam -

Thesis Paul Meijer
Access to Groundwater Case study on extraction of groundwater in the A-K basin in the north of Chennai, India Master Thesis by Paul Meijer March 2012 Law and Governance Group Irrigation and Water Engineering Group Master Thesis Report Access to groundwater Case study on extraction of groundwater in the A-K basin in the north of Chennai, India Paul Meijer March 2012 Registration number 850606-554-070 International Development Studies Thesis code: LAW-80433 Supervisors: Dr. D. Roth Dr. Ir. M. Zwarteveen Rural Sociology Group Irrigation and Water Engineering Group Wageningen University Wageningen University The Netherlands The Netherlands Prof. N.K. Ambujam Dr. P. Nelliyat Centre for Water Resources Centre for Water Resources Anna University Anna University India India ii Master Thesis Report Preface and acknowledgement The master International Development Studies at Wageningen University (WUR) in the Netherlands has given me extensive preparation to do research in a developing country. I have been educated to apply and test development theories in practise, I have been trained in research methods, and my awareness has been raised to the many ethical and practical pitfalls that research abroad potentially entails. Doing research abroad was a life changing experience for me and has given me much more experience in scientific knowledge generation than hundreds of textbooks could have done. I stayed in India for three months where I had a wonderful time. I am most grateful to the Centre for Water Resources (CWR) at Anna University. I would like to express my appreciation to all the people within CWR, who have assisted me in fulfilling this research and I want to say that without them this thesis would not have been what it is today. -

Annual Work Plan & Budget 2003-2004
SARVA SHIKSHA ABHIYAN DISTRICT ELEMENTARY EDUCATION PLAN ANNUAL WORK PLAN & BUDGET 2003-2004 NIEPA DC □12081 THIRUVALLUR DISTRICT TAMILNADU L»RART & BOCVIIilTATM C H W Ia4«i tu»» of KAncatioaal rl8av*^j| Administration. 17-B, :in Aurobindo Matf« New Oelhi-ll(:^i.6 J) " [%t$\ DOC, No .............. *'«te---------------— . INDEX SI. No. Chapters Page No 1 1‘LAN OVERVIEW PROGRESS RIVIEW 30 ACTIVITIES AND BUDGET 74 1 I List of Contents C h a p ter 1 • - Plan Overview 1.1 Introduction 1.2 Planning process 13 General Profile 1.4 Educational Profile 1.4.1 Access h:nrolmcnt - GHR & NF.R 1.4.2. I iUns c^'(iirls 1.4.2.2 SC/ST children 1.4.2.3 Disabled children 1.4.3 Completion rate 1.4.4 Repetition rate 1.4.5 Drop out rale 1.4.6 'Fransition rate 1.4.7 Teacher pupil ratio 1.5 Early childhood Care and Education 1.6 Out of school Children 1.7 Special Focus Group 1.8 VECs, CRCs, BRCs 1.9 Infrastructure 1.9.1 Block resource Centre 1.9.2 Cluster resource Centre 1.9.3 Three classrooms 1.9.4 Two classrooms 1.9.5 Toilets 1.9.6 Drinking water Facilities 1.10 District project office Chapter II - Progress Review 2.1 Introduction 2.2 Progress in ACCESS 2.2.1 Opening of Primary schools 2.2.2 Upper Primary schools 2.2.3 EGS centres 2.3 Progress in ENROLM ENT 2.3.1 Boys & Girls 2.3.2 SC/ST 2.3.3 Disabled 2.4 Progress in CO M PLETIO N 2.5 Retention 2.6 Transition 2.7 Attcudauce 2.8 Pupils’ achievem ent 2.9 M ainstream ing out of school children 2.9.1 Bridge courses/Transit camps 2.9.2 Residential Schools 2.10 Appointment of Teachers 2.11 Programmes for Disabled -

Araniyar Sub Basin
TN – IAMWARM PROJECT ARANIYAR SUB BASIN DETAILED PROJECT REPORT WATER RESOURCES DEPARTMENT 1. WATER RESOURCES ORGANISATION 1.1 INTRODUCTION 1.1 INTRODUCTION 1.1.1 General Agriculture is the dominant sector in the Indian economy. Tamil Nadu depends largely on the surface water irrigation as well as ground water irrigation. The state has used the surface and ground water potentials to the maximum limit and hence the future development and expansion depends only on the efficient and economical use of water potential and resources. To achieve higher water use efficiency, it is necessary to improve and upgrade the existing conveyance system and also to introduce modern irrigation methods. With the above objective, a comprehensive programme has been proposed with a Multi Disciplinary Approach. 1.1.2 Description of the Araniyar Sub Basin The Araniar River is one of the sub basin in Chennai basin which is located in the Northen part of Chennai basin and Pulicat lake. The Araniar river originates near Karnetnagar in Nagiri hills of Chittur District of Andhra Pradesh at an altitude of 600m above MSL. The river runs in Andhra Pradesh for a distance of 65.20 Km up to Suruttapalli Anicut before entering into Tamil Nadu. Beyond this the river runs in Tamil Nadu is 66.40Km and finally confluence into Bay of Bengal near Pulicat. The river basin spreads with a total extent of 1470Sq.Km and out of which 763 Sq.Km lies in Tamil Nadu. This river segment in Tamil Nadu irrigates 174 irrigation tanks to an extent of 22319.115 Hectares. -

Qty AGRICULTURAL ENGINEERING DEPARTMENT the Beneficiary Details of Custom Hiring Centres Established So Far with Subsidy Assista
AGRICULTURAL ENGINEERING DEPARTMENT The Beneficiary details of Custom Hiring Centres established so far with subsidy assistance of SMAM and NADP Scheme from the year 2014-15 to 2020-21 Tiruvallur Sl. Name of Beneficiary Address of Custom Hiring Centre Name of Block Mobile No/Phone No. Name of Agrl.Machinery available in the centre Qty No. 1 Jayaseelan, Agricultural Development Programme Sholavaram 9176279602 Farmers Association, Transplanter (6 ROW)-1, 1 Transplanter (4 ROW)-1, 1 Tractor-(45 HP) -1, 1 Tractor Mini -(24 HP) -1, 1 Rotavator-1 1 2 Thiru. Murali Nathakoil Thippai, Ekkadu, Ekkadu 9381024612 TiruvallurTaluk. 1.Transplanter (6 ROW)-1, 1 2.Tractor-(50 HP) -1, 1 3.Tractor-(35 HP)-1, 1 4.Rotavator-(42)-1, 1 5.Rotavator - (36)-1, 1 6.Power weeder-1. 1 3 Thiru. S.Venkadesan, S/o.Sankariaha Naidu, Panjatti, Ellapuram 9444021245 Ponneri. 1.Transplanter (6 ROW)-1, 1 2.Tractor-(47 RPSCE) -1, 1 3.Tractor-(47 RPSCE) -1, 1 4.Rotavator-(42)-1. 1 5.Rotavator-(42)-1. 1 4 Thiru. G.Adhiseshan, S/o.Govindaraj, Perampakkam, Kadambathur 9444795839 Kadambathur Block Tiruvallur 1.Transplanter (6 ROW)-1, 1 Taluk 2.Tractor-(47 RPSCE) -1, 1 3.Tractor-(47 RPSCE) -1, 1 4.Rotavator-(42)-1. 1 5.Rotavator-(42)-1. 1 AGRICULTURAL ENGINEERING DEPARTMENT The Beneficiary details of Custom Hiring Centres established so far with subsidy assistance of SMAM and NADP Scheme from the year 2014-15 to 2020-21 Tiruvallur 5 Thiru. M.V.Parandhaman S/o Vijayaranga Mudaliar, Medur village Minjur 9600904666 &Post, Meenjur Block, Ponneri Taluk.