ANALYSIS of EARLY STROKE-INDUCED CHANGES in CIRCULATING LEUKOCYTE COUNTS USING TRANSCRIPTOMIC Grant C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Reascreen™ MAX Kit, Human, FFPE, Version 01 Panel Composition – 89 Antibody Conjugates # 130-127-847
REAscreen™ MAX Kit, human, FFPE, version 01 Panel composition – 89 antibody conjugates # 130-127-847 REAscreen MAX Antibody Plate 1 2 3 4 5 6 7 8 9 10 11 12 IRF-7 CD104 CD158i CD181 CD295 A pS477/ SSRP1 CD45RA ZAP70 TTF-1 CD138 Sox2 (Integrin CD162 (KIR2DS4) (CXCR1) (LEPR) pS479 β4) CD134 B CD240DCE IRF-7 CD15 CD43 AN2 Galectin-3 CD66c TOM22 CD147 CD66acde (OX40) Cyto- CD279 CD234 C Syk Slug LRP-4 IgD Vimentin Dectin-1 Galectin-9 keratin CLA (PD1) (DARC) PAX-5 CD195 CD196 CD88 CD305 D FAK pS910 p53 FcεRIα PCNA CD268 BMI-1 (BSAP) (CCR5) (CCR6) (C5AR) (LAIR-1) CD334 CD45R CD226 AKT Pan E PKCα BATF Bcl-2 CD65 CD223 CD52 CD66abce (FGFR4) (B220) (DNAM-1) (PKB) CD182 CD20 CD326 Cyto- Podo- HLA-DR, F Cyto- CD45 MLC2v CD66b Hsp70 CD45RB (CXCR2) plasmic (EpCAM) keratin 8 planin DP, DQ CD235a α-Actinin CD202b CD317 G Dnmt3b Jak1 SUSD2 EZH2 (Glycopho (Sarco- CD79a CD40 CD99 (TIE-2) (BST2) rin A) meric) p120 CD239 CD271 H Catenin CD44 CD57 CD123 Ki-67 CD233 CD45RO β-Catenin CD100 (BCAM) (LNGFR) pS879 Antigen Clone Fluorochrome Antibody type Plate position AKT Pan (PKB) REA676 PE REAfinity™ E11 AN2 REA989 PE REAfinity B6 BATF REA486 FITC REAfinity E2 1 Antigen Clone Fluorochrome Antibody type Plate position Bcl-2 REA872 FITC REAfinity E5 BMI-1 REA438 FITC REAfinity D10 CD100 REA316 FITC REAfinity H11 CD104 (Integrin β4) REA236 FITC REAfinity A10 CD123 REA918 FITC REAfinity H5 CD134 (OX40) ACT35 FITC Hybridoma B1 CD138 44F9 FITC Hybridoma A8 CD147 REA282 FITC REAfinity B10 CD15 VIMC6 FITC Hybridoma B4 CD158i (KIR2DS4) JJC11.6 PE Hybridoma A1 CD162 REA319 -
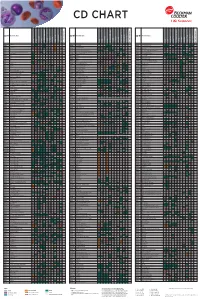
Flow Reagents Single Color Antibodies CD Chart
CD CHART CD N° Alternative Name CD N° Alternative Name CD N° Alternative Name Beckman Coulter Clone Beckman Coulter Clone Beckman Coulter Clone T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells T Cells B Cells Granulocytes NK Cells Macrophages/Monocytes Platelets Erythrocytes Stem Cells Dendritic Cells Endothelial Cells Epithelial Cells CD1a T6, R4, HTA1 Act p n n p n n S l CD99 MIC2 gene product, E2 p p p CD223 LAG-3 (Lymphocyte activation gene 3) Act n Act p n CD1b R1 Act p n n p n n S CD99R restricted CD99 p p CD224 GGT (γ-glutamyl transferase) p p p p p p CD1c R7, M241 Act S n n p n n S l CD100 SEMA4D (semaphorin 4D) p Low p p p n n CD225 Leu13, interferon induced transmembrane protein 1 (IFITM1). p p p p p CD1d R3 Act S n n Low n n S Intest CD101 V7, P126 Act n p n p n n p CD226 DNAM-1, PTA-1 Act n Act Act Act n p n CD1e R2 n n n n S CD102 ICAM-2 (intercellular adhesion molecule-2) p p n p Folli p CD227 MUC1, mucin 1, episialin, PUM, PEM, EMA, DF3, H23 Act p CD2 T11; Tp50; sheep red blood cell (SRBC) receptor; LFA-2 p S n p n n l CD103 HML-1 (human mucosal lymphocytes antigen 1), integrin aE chain S n n n n n n n l CD228 Melanotransferrin (MT), p97 p p CD3 T3, CD3 complex p n n n n n n n n n l CD104 integrin b4 chain; TSP-1180 n n n n n n n p p CD229 Ly9, T-lymphocyte surface antigen p p n p n -

Snipa Snpcard
SNiPAcard Block annotations Block info genomic range chr19:55,117,749-55,168,602 block size 50,854 bp variant count 74 variants Basic features Conservation/deleteriousness Linked genes μ = -0.557 [-4.065 – AC009892.10 , AC009892.5 , AC009892.9 , AC245036.1 , AC245036.2 , phyloP 2.368] gene(s) hit or close-by AC245036.3 , AC245036.4 , AC245036.5 , AC245036.6 , LILRA1 , LILRB1 , LILRB4 , MIR8061 , VN1R105P phastCons μ = 0.059 [0 – 0.633] eQTL gene(s) CTB-83J4.2 , LILRA1 , LILRA2 , LILRB2 , LILRB5 , LILRP1 μ = -0.651 [-4.69 – 2.07] AC008984.5 , AC008984.5 , AC008984.6 , AC008984.6 , AC008984.7 , AC008984.7 , AC009892.10 , AC009892.10 , AC009892.2 , AC009892.2 , AC009892.5 , AC010518.3 , AC010518.3 , AC011515.2 , AC011515.2 , AC012314.19 , AC012314.19 , FCAR , FCAR , FCAR , FCAR , FCAR , FCAR , FCAR , FCAR , FCAR , FCAR , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL1 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL3 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , KIR2DL4 , -

Supplementary Material DNA Methylation in Inflammatory Pathways Modifies the Association Between BMI and Adult-Onset Non- Atopic
Supplementary Material DNA Methylation in Inflammatory Pathways Modifies the Association between BMI and Adult-Onset Non- Atopic Asthma Ayoung Jeong 1,2, Medea Imboden 1,2, Akram Ghantous 3, Alexei Novoloaca 3, Anne-Elie Carsin 4,5,6, Manolis Kogevinas 4,5,6, Christian Schindler 1,2, Gianfranco Lovison 7, Zdenko Herceg 3, Cyrille Cuenin 3, Roel Vermeulen 8, Deborah Jarvis 9, André F. S. Amaral 9, Florian Kronenberg 10, Paolo Vineis 11,12 and Nicole Probst-Hensch 1,2,* 1 Swiss Tropical and Public Health Institute, 4051 Basel, Switzerland; [email protected] (A.J.); [email protected] (M.I.); [email protected] (C.S.) 2 Department of Public Health, University of Basel, 4001 Basel, Switzerland 3 International Agency for Research on Cancer, 69372 Lyon, France; [email protected] (A.G.); [email protected] (A.N.); [email protected] (Z.H.); [email protected] (C.C.) 4 ISGlobal, Barcelona Institute for Global Health, 08003 Barcelona, Spain; [email protected] (A.-E.C.); [email protected] (M.K.) 5 Universitat Pompeu Fabra (UPF), 08002 Barcelona, Spain 6 CIBER Epidemiología y Salud Pública (CIBERESP), 08005 Barcelona, Spain 7 Department of Economics, Business and Statistics, University of Palermo, 90128 Palermo, Italy; [email protected] 8 Environmental Epidemiology Division, Utrecht University, Institute for Risk Assessment Sciences, 3584CM Utrecht, Netherlands; [email protected] 9 Population Health and Occupational Disease, National Heart and Lung Institute, Imperial College, SW3 6LR London, UK; [email protected] (D.J.); [email protected] (A.F.S.A.) 10 Division of Genetic Epidemiology, Medical University of Innsbruck, 6020 Innsbruck, Austria; [email protected] 11 MRC-PHE Centre for Environment and Health, School of Public Health, Imperial College London, W2 1PG London, UK; [email protected] 12 Italian Institute for Genomic Medicine (IIGM), 10126 Turin, Italy * Correspondence: [email protected]; Tel.: +41-61-284-8378 Int. -

Whole Exome Sequencing in Families at High Risk for Hodgkin Lymphoma: Identification of a Predisposing Mutation in the KDR Gene
Hodgkin Lymphoma SUPPLEMENTARY APPENDIX Whole exome sequencing in families at high risk for Hodgkin lymphoma: identification of a predisposing mutation in the KDR gene Melissa Rotunno, 1 Mary L. McMaster, 1 Joseph Boland, 2 Sara Bass, 2 Xijun Zhang, 2 Laurie Burdett, 2 Belynda Hicks, 2 Sarangan Ravichandran, 3 Brian T. Luke, 3 Meredith Yeager, 2 Laura Fontaine, 4 Paula L. Hyland, 1 Alisa M. Goldstein, 1 NCI DCEG Cancer Sequencing Working Group, NCI DCEG Cancer Genomics Research Laboratory, Stephen J. Chanock, 5 Neil E. Caporaso, 1 Margaret A. Tucker, 6 and Lynn R. Goldin 1 1Genetic Epidemiology Branch, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 2Cancer Genomics Research Laboratory, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; 3Ad - vanced Biomedical Computing Center, Leidos Biomedical Research Inc.; Frederick National Laboratory for Cancer Research, Frederick, MD; 4Westat, Inc., Rockville MD; 5Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD; and 6Human Genetics Program, Division of Cancer Epidemiology and Genetics, National Cancer Institute, NIH, Bethesda, MD, USA ©2016 Ferrata Storti Foundation. This is an open-access paper. doi:10.3324/haematol.2015.135475 Received: August 19, 2015. Accepted: January 7, 2016. Pre-published: June 13, 2016. Correspondence: [email protected] Supplemental Author Information: NCI DCEG Cancer Sequencing Working Group: Mark H. Greene, Allan Hildesheim, Nan Hu, Maria Theresa Landi, Jennifer Loud, Phuong Mai, Lisa Mirabello, Lindsay Morton, Dilys Parry, Anand Pathak, Douglas R. Stewart, Philip R. Taylor, Geoffrey S. Tobias, Xiaohong R. Yang, Guoqin Yu NCI DCEG Cancer Genomics Research Laboratory: Salma Chowdhury, Michael Cullen, Casey Dagnall, Herbert Higson, Amy A. -

Association of KIR2DS4 and Its Variant KIR1D with Leukemia
Letters to the Editor 2129 Association of KIR2DS4 and its variant KIR1D with leukemia Leukemia (2008) 22, 2129–2130; doi:10.1038/leu.2008.108; comparison with healthy subjects. We included 90 adults published online 8 May 2008 with chronic myeloid leukemia (CML, n ¼ 31), acute myeloid leukemia ( n ¼ 38), and acute lymphoblastic leukemia (n ¼ 21) who were candidates for allogeneic hematopoietic stem cell Natural killer (NK) cells are postulated to take part in innate transplantation. KIR2DS4n001 and KIR1D alleles were detected immunosurveillance against leukemia, contributing to both the according to previously described methodology5 in patients as disease control and clearance.1 A systematic review regarding well as in their HLA-matched related (n ¼ 31) or unrelated the role of NK cell receptors and their ligands in leukemia has (n ¼ 59) donors, serving as controls. Such selection of control recently been published by Verheyden and Demanet.1 group let us avoid potential bias resulting from the association of The activity of NK cells depends on the balance of activating HLA genotype with leukemia. All patients and donors were and inhibitory signals that are transmitted through respective Caucasoids. Patients and sibling donors were of Polish origin, receptors, including killer immunoglobulin-like receptors (KIRs). while the majority of unrelated donors were either Polish or HLA class I molecules are ligands for inhibitory KIRs, whereas German. As previously reported, the distribution of KIR genes ligands for their activating counterparts have not been well among these two populations is very similar.6 defined. As well, the physiological role of activating KIRs The frequencies of various allele combinations in patients, remains obscure and appears particularly intriguing in view of donors and population controls are listed in Table 1. -

NK Cells: Receptors and Functions Eric Vivier and Sophie Ugolini
NK cells: receptors and functions Eric Vivier and Sophie Ugolini Natural killer (NK) cells were identified in 1975 as lymphocytes of the innate many processes that were originally restricted to adaptive immunity, such immune system that can kill tumour cells. Since then, NK cells have been as priming, education and memory, are now known to occur in NK cells. shown to kill an array of ‘stressed’ cells and secrete cytokines that Indeed, NK cells undergo sophisticated processes of adaptation that allow participate in shaping adaptive immune responses. A key feature of NK cells them to be tuned to their environment. There is also a growing interest in resides in their capacity to distinguish stressed cells (such as tumour cells, manipulating NK cells in innovative therapeutic settings. For example, the infected cells and damaged cells) from normal cells. Although NK cells are understanding of NK cell inhibition by MHC class I-specific receptors has generally considered to be components of early innate immune defence, prompted the design of innovative anticancer therapies. The NK cell detection system includes numerous receptors, Key receptors on human NK cells the engagement of which dictates the quality and intensity Inhibitory receptors Activating receptors, adhesion molecules or co-stimulatory molecules of the NK cell response. NK cells use inhibitory receptors to gauge the absence of constitutively expressed self molecules Target cell Nectin 2 SLAMF7 Sialic CLEC2D (CD112, PVRL2) NECL2 L-selectin NECL5 AICL NTB-A (CRACC, on susceptible target cells. As a consequence, NK cells can Receptors for MHC class I and class I-Iike molecules B7-H6 acid Cadherins (LLT1) CMV pp65 NECL5 (CADM1) (CD62L) (CD155, PVR) (CLEC2B) CEACAM1 (SLAMF6) CS1, CD319) recognize ‘missing self’ on haematopoietic cells. -

4871.Full.Pdf
Coordinated Regulation of NK Receptor Expression in the Maturing Human Immune System This information is current as Dara M. Strauss-Albee, Amir Horowitz, Peter Parham and of October 2, 2021. Catherine A. Blish J Immunol 2014; 193:4871-4879; Prepublished online 6 October 2014; doi: 10.4049/jimmunol.1401821 http://www.jimmunol.org/content/193/10/4871 Downloaded from Supplementary http://www.jimmunol.org/content/suppl/2014/10/03/jimmunol.140182 Material 1.DCSupplemental http://www.jimmunol.org/ References This article cites 46 articles, 20 of which you can access for free at: http://www.jimmunol.org/content/193/10/4871.full#ref-list-1 Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on October 2, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2014 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology Coordinated Regulation of NK Receptor Expression in the Maturing Human Immune System Dara M. Strauss-Albee,*,† Amir Horowitz,*,‡,x Peter Parham,*,‡,x and Catherine A. -
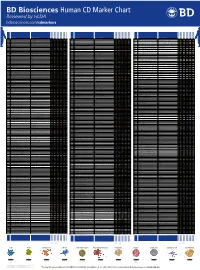
Human CD Marker Chart Reviewed by HLDA1 Bdbiosciences.Com/Cdmarkers
BD Biosciences Human CD Marker Chart Reviewed by HLDA1 bdbiosciences.com/cdmarkers 23-12399-01 CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD Alternative Name Ligands & Associated Molecules T Cell B Cell Dendritic Cell NK Cell Stem Cell/Precursor Macrophage/Monocyte Granulocyte Platelet Erythrocyte Endothelial Cell Epithelial Cell CD1a R4, T6, Leu6, HTA1 b-2-Microglobulin, CD74 + + + – + – – – CD93 C1QR1,C1qRP, MXRA4, C1qR(P), Dj737e23.1, GR11 – – – – – + + – – + – CD220 Insulin receptor (INSR), IR Insulin, IGF-2 + + + + + + + + + Insulin-like growth factor 1 receptor (IGF1R), IGF-1R, type I IGF receptor (IGF-IR), CD1b R1, T6m Leu6 b-2-Microglobulin + + + – + – – – CD94 KLRD1, Kp43 HLA class I, NKG2-A, p39 + – + – – – – – – CD221 Insulin-like growth factor 1 (IGF-I), IGF-II, Insulin JTK13 + + + + + + + + + CD1c M241, R7, T6, Leu6, BDCA1 b-2-Microglobulin + + + – + – – – CD178, FASLG, APO-1, FAS, TNFRSF6, CD95L, APT1LG1, APT1, FAS1, FASTM, CD95 CD178 (Fas ligand) + + + + + – – IGF-II, TGF-b latency-associated peptide (LAP), Proliferin, Prorenin, Plasminogen, ALPS1A, TNFSF6, FASL Cation-independent mannose-6-phosphate receptor (M6P-R, CIM6PR, CIMPR, CI- CD1d R3G1, R3 b-2-Microglobulin, MHC II CD222 Leukemia -

Humanized Mouse Model Supports Development, Function, and Tissue
Humanized mouse model supports development, PNAS PLUS function, and tissue residency of human natural killer cells Dietmar Herndler-Brandstettera,1, Liang Shana,1,2, Yi Yaob,3, Carmen Stechera, Valerie Plajera, Melanie Lietzenmayera, Till Strowiga,4, Marcel R. de Zoetea,5, Noah W. Palma, Jie Chena, Catherine A. Blishc, Davor Frletad, Cagan Gurerd, Lynn E. Macdonaldd, Andrew J. Murphyd, George D. Yancopoulosd, Ruth R. Montgomeryb, and Richard A. Flavella,e,6 aDepartment of Immunobiology, Yale University School of Medicine, New Haven, CT 06519; bDepartment of Internal Medicine, Yale University School of Medicine, New Haven, CT 06519; cDepartment of Medicine, Stanford University School of Medicine, Stanford, CA 94305; dRegeneron Pharmaceuticals Inc., Tarrytown, NY 10591; and eHoward Hughes Medical Institute, New Haven, CT 06519 Contributed by Richard A. Flavell, September 18, 2017 (sent for review March 30, 2017; reviewed by Hergen Spits and Wayne M. Yokoyama) Immunodeficient mice reconstituted with a human immune sys- acids identical between humans and mice, is interleukin 15 (IL- tem represent a promising tool for translational research as they 15). IL-15 is essential for the development and/or function of NK may allow modeling and therapy of human diseases in vivo. cells, memory CD8 T cells, CD8αα intraepithelial lymphocytes However, insufficient development and function of human natural (IELs), and tissue-resident NK cells (10, 11). In addition, phys- killer (NK) cells and T cell subsets limit the applicability of human- iological levels of IL-15 are essential for functional antitumor ized mice for studying cancer biology and therapy. Here, we de- responses of NK and T cells in cancer immunotherapy (12). -

NK-Activating Receptor KIR2DS4 MHC Class I-Independent
MHC Class I-Independent Recognition of NK-Activating Receptor KIR2DS4 Gil Katz, Roi Gazit, Tal I. Arnon, Tsufit Gonen-Gross, Gabi Tarcic, Gal Markel, Raizy Gruda, Hagit Achdout, Olga This information is current as Drize, Sharon Merims and Ofer Mandelboim of September 29, 2021. J Immunol 2004; 173:1819-1825; ; doi: 10.4049/jimmunol.173.3.1819 http://www.jimmunol.org/content/173/3/1819 Downloaded from References This article cites 31 articles, 17 of which you can access for free at: http://www.jimmunol.org/content/173/3/1819.full#ref-list-1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication by guest on September 29, 2021 *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2004 by The American Association of Immunologists All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. The Journal of Immunology MHC Class I-Independent Recognition of NK-Activating Receptor KIR2DS41 Gil Katz,* Roi Gazit,* Tal I. Arnon,* Tsufit Gonen-Gross,* Gabi Tarcic,* Gal Markel,* Raizy Gruda,* Hagit Achdout,* Olga Drize,† Sharon Merims,† and Ofer Mandelboim2* Natural killer cells are capable of killing tumor and virus-infected cells.