6Th CRM Main Report 2012
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Study on Human Rights Violation of Tangkhul Community in Ukhrul District, Manipur
A STUDY ON HUMAN RIGHTS VIOLATION OF TANGKHUL COMMUNITY IN UKHRUL DISTRICT, MANIPUR. A THESIS SUBMITTED TO THE TILAK MAHARASHTRA VIDYAPEETH, PUNE FOR THE DEGREE OF DOCTOR OF PHILOSOPHY IN SOCIAL WORK UNDER THE BOARD OF SOCIAL WORK STUDIES BY DEPEND KAZINGMEI PRN. 15514002238 UNDER THE GUIDANCE OF DR. G. R. RATHOD DIRECTOR, SOCIAL SCIENCE CENTRE, BVDU, PUNE SEPTEMBER 2019 DECLARATION I, DEPEND KAZINGMEI, declare that the Ph.D thesis entitled “A Study on Human Rights Violation of Tangkhul Community in Ukhrul District, Manipur.” is the original research work carried by me under the guidance of Dr. G.R. Rathod, Director of Social Science Centre, Bharati Vidyapeeth University, Pune, for the award of Ph.D degree in Social Work of the Tilak Maharashtra Vidyapeeth, Pune. I hereby declare that the said research work has not submitted previously for the award of any Degree or Diploma in any other University or Examination body in India or abroad. Place: Pune Mr. Depend Kazingmei Date: Research Student i CERTIFICATE This is to certify that the thesis entitled, “A Study on Human Rights Violation of Tangkhul Community in Ukhrul District, Manipur”, which is being submitted herewith for the award of the Degree of Ph.D in Social Work of Tilak Maharashtra Vidyapeeth, Pune is the result of original research work completed by Mr. Depend Kazingmei under my supervision and guidance. To the best of my knowledge and belief the work incorporated in this thesis has not formed the basis for the award of any Degree or similar title of this or any other University or examining body. -

Maternal Health 8
MATERNAL HEALTH 8 Maternal and child health has remained an integral part of the Family Welfare Programme of India since the time of the First and Second Five-Year Plans (1951-56 and 1956- 61) when the Government of India took steps to strengthen maternal and child health services. As part of the Minimum Needs Programme initiated during the Fifth Five-Year Plan (1974-79), maternal health, child health, and nutrition services were integrated with family planning services. In 1992-93, the Child Survival and Safe Motherhood Programme continued the process of integration by bringing together several key child survival interventions with safe motherhood and family planning activities (Ministry of Health and Family Welfare, 1992). In 1996, safe motherhood and child health services were incorporated into the Reproductive and Child Health Programme (RCH). The National Population Policy adopted by the Government of India in 2000 reiterates the government’s commitment to safe motherhood programmes within the wider context of reproductive health (Ministry of Health and Family Welfare, 2000). Several of the national sociodemographic goals for 2010 specified by the policy pertain to safe motherhood. For 2010, the goals are that 80 percent of all deliveries should take place in institutions, 100 percent of deliveries should be attended by trained personnel, and the maternal mortality ratio should be reduced to a level below 100 per 100,000 live births. To improve the availability of and access to quality health care, especially for those residing in rural areas, the poor, women, and children, the government recently launched the National Rural Health Mission for the 2005-2012 period. -

Khadi Institution Profile Khadi and Village
KHADI AND VILLAGE INDUSTRIES COMISSION KHADI INSTITUTION PROFILE Office Name : SO DEHRADUN UTTARAKHAND Institution Code : 2155 Institution Name : KSHETRIYA SHREE GANDHI ASHRAM Address: : GAUCHAR Post : GAUCHAR City/Village : GAUCHAR Pincode : 246429 State : UTTARAKHAND District : CHAMOLI Aided by : KVIC District : C Contact Person Name Email ID Mobile No. Chairman : SHRI JASPAL SINGH gandhiashramgaucher@gmail. 9411365726 Secretary : SHRI INDRASAN YADAV 9410584110 Nodal Officer : Registration Detail Registration Date Registration No. Registration Type 22-03-1991 642/1990 SOC Khadi Certificate No. CZ/UP/99/REN Date : 31-MAR_2021 Khadi Mark No. KVIC/CKMC/UK/004 Khadi Mark Dt. 22-Apr-2025 Sales Outlet Details Type Name Address City Pincode Sales Outlet Ksh shree Gandhi Ashram Josimath Josimath 0 Khadi Bhandar Sales Outlet Ksh shree Gandhi Ashram Gopeshwar Gopashwar 0 khadi Bhandar Sales Outlet Ksh Shree Gandhi Ashram Chamoli Chamoli 0 Khadi Bhandar Sales Outlet Ksh Shree Gandhi Ashram Tharali Tharali 0 Khadi Bhandar Sales Outlet Ksh Shree Gandhi Ashram Gavaldya Gvaldya 0 Khadi Bhandar Sales Outlet Ksh Shree Gandhi Ashram Dewal Dewal 0 Khadi Bhandar Sales Outlet Ksh Shri Gandhi Ashram Khadi Narayangarh Narayangarh 0 Bhandar Sales Outlet Ksh Sree Gandhi Ashram Khadi Karanprayag Karanprayag 0 Bhandar Sales Outlet Ksh Sre Gandhi Ashram Khadi Gauchar Gauchar 0 Bhandar Sales Outlet Ksh Sree Gandhi Ashram Khadi Gersain Gersain 0 Bhandar Sales Outlet Ksh Sree Gandhi Ashram Khadi Pokhari Pokhari 0 Bhandar Sales Outlet Ksh Sree Gandhi Ashram Khadi -

MIGRATION of NURSING and MIDWIFERY WORKFORCE in the STATE of KERALA This Report Was Prepared by Researchers from Oxford Policy Management (Krishna D
CASE STUDY | INDIA FROM BRAIN DRAIN TO BRAIN GAIN MIGRATION OF NURSING AND MIDWIFERY WORKFORCE IN THE STATE OF KERALA This report was prepared by researchers from Oxford Policy Management (Krishna D. Rao, Aarushi Bhatnagar, Radhika Arora, Swati Srivastava, Udit Ranjan), the Centre for Development Studies, Trivandrum (S. Irudaya Rajan, Sunitha Syam), the Health Systems Research India Initiative (Arun Nair, S.J. Sini Thomas), and the WHO Country Office for India (Tomas Zapata). Please address all correspondence to Krishna D. Rao ([email protected]) and Aarushi Bhatnagar ([email protected]) © WHO, all rights reserved November 2017 Contents Acknowledgements .......................................................3 6. Discussion ....................................... 29 Abbreviations ...............................................................4 6.1 Production, stock and migration of nurses ....... 29 6.1.1 Production ...................................... 29 Executive summary ........................................................5 6.1.2 Stock .............................................. 30 1. Background ........................................ 7 6.1.3 Migration ........................................ 31 6.2 Factors influencing migration patterns ............ 33 1.1 Kerala state ..................................................9 6.2.1 Endogenous push and pull factors ....... 33 1.2 Migration of health workers........................... 10 6.2.2 Exogenous push and pull factors .........34 2. Objectives ....................................... -

Directory Establishment
DIRECTORY ESTABLISHMENT SECTOR :URBAN STATE : UTTARANCHAL DISTRICT : Almora Year of start of Employment Sl No Name of Establishment Address / Telephone / Fax / E-mail Operation Class (1) (2) (3) (4) (5) NIC 2004 : 0121-Farming of cattle, sheep, goats, horses, asses, mules and hinnies; dairy farming [includes stud farming and the provision of feed lot services for such animals] 1 MILITARY DAIRY FARM RANIKHET ALMORA , PIN CODE: 263645, STD CODE: 05966, TEL NO: 222296, FAX NO: NA, E-MAIL : N.A. 1962 10 - 50 NIC 2004 : 1520-Manufacture of dairy product 2 DUGDH FAICTORY PATAL DEVI ALMORA , PIN CODE: 263601, STD CODE: NA , TEL NO: NA , FAX NO: NA, E-MAIL 1985 10 - 50 : N.A. NIC 2004 : 1549-Manufacture of other food products n.e.c. 3 KENDRYA SCHOOL RANIKHE KENDRYA SCHOOL RANIKHET ALMORA , PIN CODE: 263645, STD CODE: 05966, TEL NO: 1980 51 - 100 220667, FAX NO: NA, E-MAIL : N.A. NIC 2004 : 1711-Preparation and spinning of textile fiber including weaving of textiles (excluding khadi/handloom) 4 SPORTS OFFICE ALMORA , PIN CODE: 263601, STD CODE: 05962, TEL NO: 232177, FAX NO: NA, E-MAIL : N.A. 1975 10 - 50 NIC 2004 : 1725-Manufacture of blankets, shawls, carpets, rugs and other similar textile products by hand 5 PANCHACHULI HATHKARGHA FAICTORY DHAR KI TUNI ALMORA , PIN CODE: 263601, STD CODE: NA , TEL NO: NA , FAX NO: NA, 1992 101 - 500 E-MAIL : N.A. NIC 2004 : 1730-Manufacture of knitted and crocheted fabrics and articles 6 HIMALAYA WOLLENS FACTORY NEAR DEODAR INN ALMORA , PIN CODE: 203601, STD CODE: NA , TEL NO: NA , FAX NO: NA, 1972 10 - 50 E-MAIL : N.A. -

To 31.12.2015 to Gram Vikas
F. No: SW-45/3/20 I 5-SWADHAR Govelnment of India Ministry of Wornen and Chitd Developrnent Shastri Biralvan, I.Jew Deihi Dated: 16.A1.2A17 . To, The Pay and Accounts Officer Ministry of Women and Child Development Shastri Bhavan; New Delhi Subject: - Reimbursement of the Grant for the period 1.04.2014 to 31.L2.2A15 to Gram Vikas (Voluntary Organization), H.No.l6-3TlI,.Vidyanagar Road, Sathupaliy, Khammam District, Telangana-507303 for running Swadhar Shelter Home & Women Helpline under Swadhar Scheme. Sir/Madam, ln continuation of this Ministry's Sanction order of even number dated 19.06.2015. I am directed toconvey the sanction of tlre President of hidia to the payinent.of fts.13,72,298/- (Rupees Thirteer. lakh seventy two thousand two hundred and ninety eight only) for the period t.84.2:'Jl4 to 31.12.2015 to Gram Vikas (Voluntary Organizatiorr), Ftr.No.l6-3UL, Vidy*nagar lioad, Sathupally, Khammam District, Telangana-507303 for financial year 2016=2Al'7 for runniug __.: Swadhar Shelter home & Women helpline under Swadhar Scheme. The details of the projeci are as .follows: (a) Location of the Project: - At Plot No. 122, H,No. 3-5113 (new H.No. 24-1-65), Sath'.rpally, Khammam District, Telangana. (b) Number of beneficiaries: 38 womerr & 5 children (for 2014-15) & 3l r.vomen & 9 childieir (for 20 I 5- I 6) 2. The grant is subject to the following conditions: i. Before the amount is paid by an Account Payee Cheque, a ceftificate is to be furnished by tlre NGO stating that no funds have been received from any other source for the purpose for which this amount has been sauctioned. -

2017 STATE of YOUTH VOLUNTEERING in INDIA 2017: State of Youth Volunteering in India
2017 STATE OF YOUTH VOLUNTEERING IN INDIA 2017: State Of Youth Volunteering In India STATE OF YOUTH VOLUNTEERING IN INDIA _________________ 2017 1 2017: State Of Youth Volunteering In India 2 2017: State Of Youth Volunteering In India TABLE OF CONTENTS LIST OF FIGURES LIST OF BOXES LIST OF CASE STUDIES OvervieW 14 1. YOUTH VOLUNTEERISM IN INDIA 22 Evolution of volunteerism in India 23 Defining youth volunteerism in India 26 Manifestations of volunteering by youth in India 29 Discourses around youth volunteering in current times 33 Measuring youth volunteering in India 34 Conclusion 36 2. ECOSYSTEM SURROUNDING YOUTH VOLUNTEERING IN INDIA 38 Government 40 Civil Society 53 Private Sector 62 Conclusion 64 3. YOUTH PERCEPTIONS ON VOLUNTEERING IN INDIA 66 Profile of respondents 67 Nature of volunteering 69 Volunteer motivations 71 Modes of communication about volunteering opportunities 79 Perceived barriers to volunteering and challenges faced 80 Perceptions of impact created on community and self 81 Conclusion 84 4. IMPACT OF YOUTH VOLUNTEERING initiatives IN INDIA 86 Volunteerism and education 87 Health and well-being 90 Gender equality and justice 93 Hunger 96 Water and sanitation 98 Climate change and disaster relief 100 Social entrepreneurship 103 Social inclusion 105 Peace, justice and strong institutions 108 Conclusion 111 5. CONCLUSION: Way FORWARD 114 ACKNOWLEDGMENTS 127 3 2017: State Of Youth Volunteering In India LIST OF FIGURES FIGURE 1: Ecosystem - youth volunteering 40 FIGURE 2: Age group 67 FIGURE 3: Educational qualification -

Impact of an Integrated Nutrition and Health Programme on Neonatal
Impact of an integrated nutrition and health programme on neonatal mortality in rural northern India Abdullah H Baqui,a Emma K Williams,a Amanda M Rosecrans,a Praween K Agrawal,a Saifuddin Ahmed,b Gary L Darmstadt,a Vishwajeet Kumar,a Usha Kiran,c Dharmendra Panwar,c Ramesh C Ahuja,d Vinod K Srivastava,d Robert E Black a & Manthuram Santosham a Objective To assess the impact of the newborn health component of a large-scale community-based integrated nutrition and health programme. Methods Using a quasi-experimental design, we evaluated a programme facilitated by a nongovernmental organization that was implemented by the Indian government within existing infrastructure in two rural districts of Uttar Pradesh, northern India. Mothers who had given birth in the 2 years preceding the surveys were interviewed during the baseline (n = 14 952) and endline (n = 13 826) surveys. The primary outcome measure was reduction of neonatal mortality. Findings In the intervention district, the frequency of home visits by community-based workers increased during both antenatal (from 16% to 56%) and postnatal (from 3% to 39%) periods, as did frequency of maternal and newborn care practices. In the comparison district, no improvement in home visits was observed and the only notable behaviour change was that women had saved money for emergency medical treatment. Neonatal mortality rates remained unchanged in both districts when only an antenatal visit was received. However, neonates who received a postnatal home visit within 28 days of birth had 34% lower neonatal mortality (35.7 deaths per 1000 live births, 95% confidence interval, CI: 29.2–42.1) than those who received no postnatal visit (53.8 deaths per 1000 live births, 95% CI: 48.9–58.8), after adjusting for sociodemographic variables. -

District Census Handbook Senapati
DISTRICT CENSUS HANDBOOK SENAPATI 1 DISTRICT CENSUS HANDBOOK SENAPATI MANIPUR SENAPATI DISTRICT 5 0 5 10 D Kilometres er Riv ri a N b o A n r e K T v L i G R u z A d LAII A From e S ! r Dimapur ve ! R i To Chingai ako PUNANAMEI Dzu r 6 e KAYINU v RABUNAMEI 6 TUNGJOY i C R KALINAMEI ! k ! LIYAI KHULLEN o L MAO-MARAM SUB-DIVISION PAOMATA !6 i n TADUBI i rak River 6 R SHAJOUBA a Ba ! R L PUNANAMEIPAOMATA SUB-DIVISION N ! TA DU BI I MARAM CENTRE ! iver R PHUBA KHUMAN 6 ak ar 6 B T r MARAM BAZAR e PURUL ATONGBA v r i R ! e R v i i PURUL k R R a PURUL AKUTPA k d C o o L R ! g n o h k KATOMEI PURUL SUB-DIVISION A I CENTRE T 6 From Tamenglong G 6 TAPHOU NAGA P SENAPATI R 6 6 !MAKHRELUI TAPHOU KUKI 6 To UkhrulS TAPHOU PHYAMEI r e v i T INDIAR r l i e r I v i R r SH I e k v i o S R L g SADAR HILLS WEST i o n NH 2 a h r t I SUB-DIVISION I KANGPOKPI (C T) ! I D BOUNDARY, STATE......................................................... G R SADAR HILLS EAST KANGPOKPI SUB-DIVISION ,, DISTRICT................................................... r r e e D ,, v v i i SUB-DIVISION.......................................... R R l a k h o HEADQUARTERS: DISTRICT......................................... p L SH SAIKUL i P m I a h c I R ,, SUB-DIVISION................................ -
Proceedings of the 61St Meeting of North Eastern Council on 27Th June
FINAL PROCEEDINGS of the 61ST MEETING Of NORTH EASTERN COUNCIL (12TH Meeting as the Statutory Regional Planning Body for the NER) On 27TH JUNE, 2012 In the Main Committee Room, Parliament House Annexe, New Delhi North Eastern Council Secretariat Nongrim Hills, Shillong – 793003 I N D E X Agenda Items Contents Page No Address of Hon’ble Chairman, NEC 1 Agenda Item No. 1 Secretary presents his report 1 – 2 Agenda Item No. 2 Confirmation of the Proceedings of the 60th (Sixtieth) Meeting of the NEC held on 16th -17th June, 2011 at New 2 – 2 Delhi Agenda Item No. 3 Discussions on the Action Taken Report of the decisions of 2 – 5 the 60th Meeting of the NEC Agenda Item No. 4 Discussions on the draft 12th Five Year Plan (2012-17) and 5 – 9 the draft Annual Plan 2012-13 of the NEC Agenda Item No. 5 Presentation by Ministry of Railways on the Action Plan 10 – 19 prepared for North Eastern Region and discussions thereon. Agenda Item No. 6 Presentation by Ministry of Road Transport & Highways on 19 - 26 the Action Plan prepared for North Eastern Region and discussions thereon. Agenda Item No. 7 Presentation by Ministry of Civil Aviation on the Action Plan 26 – 45 prepared for North Eastern Region and discussions thereon. Annexure – I Address of the Hon’ble Chairman, NEC 46 – 51 Annexure – II Report of Secretary, NEC 52 – 80 Annexure – III Written Speeches of Their Excellencies the Governors and 81 – 223 Hon’ble Chief Ministers of NE States Annexure – IV List of Participants 224 - 226 PROCEEDINGS OF THE 61st NORTH EASTERN COUNCIL MEETING HELD ON 27th JUNE, 2012 AT THE PARLIAMENT HOUSE ANNEXE, NEW DELHI. -

Executive Summary DISTRICT PROFILE
Executive Summary 2011 -12 Chandel District having an area of 3313 sq. km, population of about 144028 ( 2011 census)with an international border of about half of the district boundary has a distinction of multi ethnic tribal inhabitants with a few pockets of Meiteis, Muslims, Nepalese, Biharies and other Indian nationals specially at Moreh areas. It is one of the backward hill districts of Manipur with inaccessible problem in many of the villages even on foot and its prevailing Law and Order situation at the border villages to Myanmar. The Integrated Health Action Plan (2013-14) provides information on the various importance subjects like RCH-II, New additionalities under NRHM, Routine Immunization Strengthening, Vertical Programmes through elaborate annexures. The Integrated District Health Action Plan (DHAP) of National Rural Health Mission was prepared with a vision to address local needs and specificities, enable decentralization and public participation, facilitate interdepartmental convergence and improve accountability of Health system. DISTRICT PROFILE The Chandel district is one of the important districts of the state given the multi-lingual, multi- ethnicity culture and tradition it possesses. The District lies in the south-eastern part of Manipur. It is the border district of the state. Its neighbors are Myanmar (erstwhile Burma) on the south, Ukhrul district on the east, Churachandpur district on the south and west, and Thoubal district on north. It is about 64 km. away from Imphal. Several communities inhabit the district and they are scattered all over the district. Prominent tribes in the district are Anal, Lamkang, Kukis, Moyon, Monsang, Chothe, Thadou, Paite, and Maring etc. -
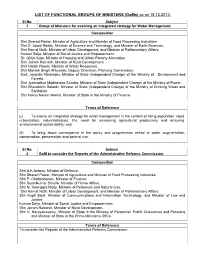
LIST of FUNCTIONAL GROUPS of MINISTERS (Goms) As on 18.12.2013
LIST OF FUNCTIONAL GROUPS OF MINISTERS (GoMs) as on 18.12.2013. Sl.No. Subject 1 Group of Ministers for evolving an integrated strategy for Water Management. Composition Shri Sharad Pawar, Minister of Agriculture and Minister of Food Processing Industries. Shri S. Jaipal Reddy, Minister of Science and Technology, and Minister of Earth Sciences. Shri Kamal Nath, Minister of Urban Development, and Minister of Parliamentary Affairs. Kumari Selja, Minister of Social Justice and Empowerment. Dr. Girija Vyas, Minister of Housing and Urban Poverty Alleviation. Shri Jairam Ramesh, Minister of Rural Development. Shri Harish Rawat, Minister of Water Resources. Shri Montek Singh Ahluwalia, Deputy Chairman, Planning Commission. Smt. Jayanthi Natarajan, Minister of State (Independent Charge) of the Ministry of Environment and Forests. Shri Jyotiraditya Madhavrao Scindia, Minister of State (Independent Charge) of the Ministry of Power. Shri Bharatsinh Solanki, Minister of State (Independent Charge) of the Ministry of Drinking Water and Sanitation. Shri Namo Narain Meena, Minister of State in the Ministry of Finance. Terms of Reference (i) To evolve an integrated strategy for water management in the context of rising population, rapid urbanization, industrialization, the need for increasing agricultural productivity and ensuring environmental sustainability; and (ii) To bring about convergence in the policy and programmes aimed at water augmentation, conservation, preservation and optimal use. Sl.No. Subjec t 2 GoM to consider the Reports of the Administrative Reforms Commission. Composition Shri A.K.Antony, Minister of Defence. Shri Sharad Pawar, Minister of Agriculture and Minister of Food Processing Industries. Shri P. Chidambaram, Minister of Finance. Shri Sushilkumar Shinde, Minister of Home Affairs.