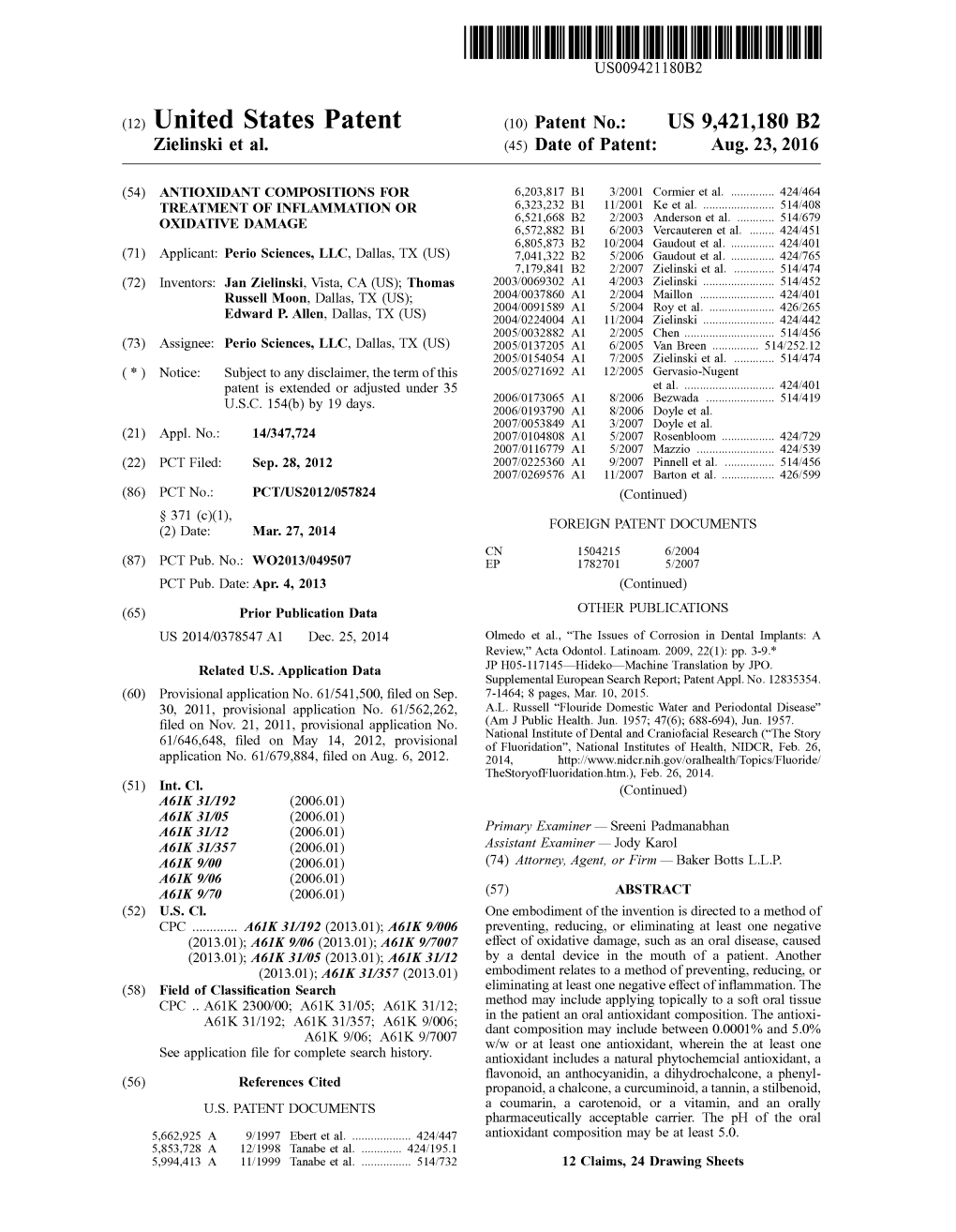
(12) United States Patent (10) Patent No.: US 9.421,180 B2 Zielinski Et Al
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Herbal Insomnia Medications That Target Gabaergic Systems: a Review of the Psychopharmacological Evidence
Send Orders for Reprints to [email protected] Current Neuropharmacology, 2014, 12, 000-000 1 Herbal Insomnia Medications that Target GABAergic Systems: A Review of the Psychopharmacological Evidence Yuan Shia, Jing-Wen Donga, Jiang-He Zhaob, Li-Na Tanga and Jian-Jun Zhanga,* aState Key Laboratory of Bioactive Substance and Function of Natural Medicines, Institute of Materia Medica, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, P.R. China; bDepartment of Pharmacology, School of Marine, Shandong University, Weihai, P.R. China Abstract: Insomnia is a common sleep disorder which is prevalent in women and the elderly. Current insomnia drugs mainly target the -aminobutyric acid (GABA) receptor, melatonin receptor, histamine receptor, orexin, and serotonin receptor. GABAA receptor modulators are ordinarily used to manage insomnia, but they are known to affect sleep maintenance, including residual effects, tolerance, and dependence. In an effort to discover new drugs that relieve insomnia symptoms while avoiding side effects, numerous studies focusing on the neurotransmitter GABA and herbal medicines have been conducted. Traditional herbal medicines, such as Piper methysticum and the seed of Zizyphus jujuba Mill var. spinosa, have been widely reported to improve sleep and other mental disorders. These herbal medicines have been applied for many years in folk medicine, and extracts of these medicines have been used to study their pharmacological actions and mechanisms. Although effective and relatively safe, natural plant products have some side effects, such as hepatotoxicity and skin reactions effects of Piper methysticum. In addition, there are insufficient evidences to certify the safety of most traditional herbal medicine. In this review, we provide an overview of the current state of knowledge regarding a variety of natural plant products that are commonly used to treat insomnia to facilitate future studies. -

2013 Book Antioxidantpropertie
Antioxidant Properties of Spices, Herbs and Other Sources Denys J. Charles Antioxidant Properties of Spices, Herbs and Other Sources Denys J. Charles Frontier Natural Products Co-op Norway, IA , USA ISBN 978-1-4614-4309-4 ISBN 978-1-4614-4310-0 (eBook) DOI 10.1007/978-1-4614-4310-0 Springer New York Heidelberg Dordrecht London Library of Congress Control Number: 2012946741 © Springer Science+Business Media New York 2013 This work is subject to copyright. All rights are reserved by the Publisher, whether the whole or part of the material is concerned, speci fi cally the rights of translation, reprinting, reuse of illustrations, recitation, broadcasting, reproduction on micro fi lms or in any other physical way, and transmission or information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed. Exempted from this legal reservation are brief excerpts in connection with reviews or scholarly analysis or material supplied speci fi cally for the purpose of being entered and executed on a computer system, for exclusive use by the purchaser of the work. Duplication of this publication or parts thereof is permitted only under the provisions of the Copyright Law of the Publisher’s location, in its current version, and permission for use must always be obtained from Springer. Permissions for use may be obtained through RightsLink at the Copyright Clearance Center. Violations are liable to prosecution under the respective Copyright Law. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a speci fi c statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -

Namenverzeichnis. Index of Names. Index Des Auteurs
Namenverzeichnis. Index of Names. Index des Auteurs. ABDERHALDEN, E. 398, 400. ARNOLD, ,V. 200, 201, 236, 237, 241. ABELSON, P. H. 379, 383, 389, 390, 393, ARONOFF, S. 26, 59, 258, 282. 394, 395, 400, 402. ASAHINA, Y. 13, 130, 131 , 175. ADAIR, G. S. 327, 371. ASANO, J. 131, 175· ADAMS, R. 147, 149, 175. ASHBY, ''I'. C. 267, 282. ADANK, K. 189, 237, 238, 241, 242, 245. ASHWORTH, B. DE 49, 61. ADRIAN, M. M. 138, 175. ASMIS, H. 190, 2lI, 214, 215, 228, 236, AGREN, G. 383, 400. 238, 241. AHLUWALIA, V. K. 13, 21, 40, 59. Aso, K. 175. AHMED, M. 173, 178. ASTON, B. C. 161, 177. AHRENS, G. 84, 118. AusKAPS, J. 434, 446. AKABORI, S. 360, 371. AVERY, G. S., Jr. 258, 270, 273, 275, ALADASHVILI, V. A. 127, 175. 276, 282, 283. ALDAG, H. J. 434, 448. ALDER, K. 77, 8o, lI8, 154, 175. BACCARINI, P. 252, 283. ALDERWEIRELDT, F. 165. BACHLI, E. 190, 204, 207, 2I5, 225, 226, ALGAR, J. 41, 59. 228, 236, 238, 239, 241, 242, 243· ALLAN, J. 34, 59· BACHMANN, E. 312, 313, 3 18. ALLEN, D. W. 332, 338, 340, 344, 345, BADER, F. E. 191, 202, 239, 241. 347, 348, 349, 350, 35 1, 352, 368 371, BAHR, K. 18 5, 187, 189, 207, 2II, 2I5, 372. 218, 219, 220, 236, 237, 238, 246. ALLEN, F. 127, 175. 'BAKER, J. W. 281, 283. ALLEN, P. W. 420, 425, 445. II BAKER, W. 3, 16, 35, 41, 43, 44, 56, 59· ALLISON, A. C. 334, 356, 372. -

USP Statement on Validation of DNA Test Methods for Regulating the Quality of Herbal Supplements
USP Statement on Validation of DNA Test Methods for Regulating the Quality of Herbal Supplements U.S. PHARMACOPEIAL CONVENTION The United States Pharmacopeial Convention Urges Scientific Validation of DNA Test Methods for Regulating the Quality of Herbal Supplements (Rockville, MD – April 16, 2015) – In response to an agreement announced between the New York State Attorney General (NYAG) and GNC Holdings, Inc. (GNC) the United States Pharmacopeial Convention (USP), an independent, science based, standards setting organization and publishers of the United States Pharmacopeia-National Formulary (USP-NF), an official compendia of quality standards for dietary supplements sold in the U.S., issued the following statement: Statement by Gabriel Giancaspro, PhD – Vice President –Foods, Dietary Supplement and Herbal Medicines United States Pharmacopeial Convention (USP) “As a science-based standards-setting organization, the United States Pharmacopeial Convention (USP) has a keen interest in adopting emerging technologies to ensure the test methods and quality standards included in the United States Pharmacopeia-National Formulary (USP-NF) are current and reflect the state of the industry. DNA testing including DNA Barcoding, is just one example of a technology that has been recently added to the USP-NF. As of December 2014, DNA-based identification methods are included in the official USP chapter <563> Identification of Articles of Botanical Origin. However, this method is not yet referenced in a USP-NF monograph (quality standard) for a specific ingredient or product. That is because USP quality standards are specific for each ingredient, product and dosage form and the standards we develop include only those test methods that have been scientifically validated and shown to be fit for purpose. -

Natural Chalcones in Chinese Materia Medica: Licorice
Hindawi Evidence-Based Complementary and Alternative Medicine Volume 2020, Article ID 3821248, 14 pages https://doi.org/10.1155/2020/3821248 Review Article Natural Chalcones in Chinese Materia Medica: Licorice Danni Wang ,1 Jing Liang,2 Jing Zhang,1 Yuefei Wang ,1 and Xin Chai 1 1Tianjin State Key Laboratory of Modern Chinese Medicine, Tianjin University of Traditional Chinese Medicine, Tianjin 301617, China 2School of Foreign Language, Chengdu University of Traditional Chinese Medicine, Sichuan 611137, China Correspondence should be addressed to Xin Chai; [email protected] Received 28 August 2019; Accepted 7 February 2020; Published 15 March 2020 Academic Editor: Veronique Seidel Copyright © 2020 Danni Wang et al. -is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Licorice is an important Chinese materia medica frequently used in clinical practice, which contains more than 20 triterpenoids and 300 flavonoids. Chalcone, one of the major classes of flavonoid, has a variety of biological activities and is widely distributed in nature. To date, about 42 chalcones have been isolated and identified from licorice. -ese chalcones play a pivotal role when licorice exerts its pharmacological effects. According to the research reports, these compounds have a wide range of biological activities, containing anticancer, anti-inflammatory, antimicrobial, antioxidative, antiviral, antidiabetic, antidepressive, hep- atoprotective activities, and so on. -is review aims to summarize structures and biological activities of chalcones from licorice. We hope that this work can provide a theoretical basis for the further studies of chalcones from licorice. -

Phytochem Referenzsubstanzen
High pure reference substances Phytochem Hochreine Standardsubstanzen for research and quality für Forschung und management Referenzsubstanzen Qualitätssicherung Nummer Name Synonym CAS FW Formel Literatur 01.286. ABIETIC ACID Sylvic acid [514-10-3] 302.46 C20H30O2 01.030. L-ABRINE N-a-Methyl-L-tryptophan [526-31-8] 218.26 C12H14N2O2 Merck Index 11,5 01.031. (+)-ABSCISIC ACID [21293-29-8] 264.33 C15H20O4 Merck Index 11,6 01.032. (+/-)-ABSCISIC ACID ABA; Dormin [14375-45-2] 264.33 C15H20O4 Merck Index 11,6 01.002. ABSINTHIN Absinthiin, Absynthin [1362-42-1] 496,64 C30H40O6 Merck Index 12,8 01.033. ACACETIN 5,7-Dihydroxy-4'-methoxyflavone; Linarigenin [480-44-4] 284.28 C16H12O5 Merck Index 11,9 01.287. ACACETIN Apigenin-4´methylester [480-44-4] 284.28 C16H12O5 01.034. ACACETIN-7-NEOHESPERIDOSIDE Fortunellin [20633-93-6] 610.60 C28H32O14 01.035. ACACETIN-7-RUTINOSIDE Linarin [480-36-4] 592.57 C28H32O14 Merck Index 11,5376 01.036. 2-ACETAMIDO-2-DEOXY-1,3,4,6-TETRA-O- a-D-Glucosamine pentaacetate 389.37 C16H23NO10 ACETYL-a-D-GLUCOPYRANOSE 01.037. 2-ACETAMIDO-2-DEOXY-1,3,4,6-TETRA-O- b-D-Glucosamine pentaacetate [7772-79-4] 389.37 C16H23NO10 ACETYL-b-D-GLUCOPYRANOSE> 01.038. 2-ACETAMIDO-2-DEOXY-3,4,6-TRI-O-ACETYL- Acetochloro-a-D-glucosamine [3068-34-6] 365.77 C14H20ClNO8 a-D-GLUCOPYRANOSYLCHLORIDE - 1 - High pure reference substances Phytochem Hochreine Standardsubstanzen for research and quality für Forschung und management Referenzsubstanzen Qualitätssicherung Nummer Name Synonym CAS FW Formel Literatur 01.039. -

Curcumin in Autoimmune and Rheumatic Diseases
nutrients Review Curcumin in Autoimmune and Rheumatic Diseases Melissa Yang, Umair Akbar and Chandra Mohan * Department of Biomedical Engineering, University of Houston, 3517 Cullen Blvd, Room 2004, Houston, TX 77204, USA; [email protected] (M.Y.); [email protected] (U.A.) * Correspondence: [email protected]; Tel.: 713-743-3709 Received: 29 March 2019; Accepted: 24 April 2019; Published: 2 May 2019 Abstract: Over recent decades, many clinical trials on curcumin supplementation have been conducted on various autoimmune diseases including osteoarthritis, type 2 diabetes, and ulcerative colitis patients. This review attempts to summarize the highlights from these clinical trials. The efficacy of curcumin either alone or in conjunction with existing treatment was evaluated. Sixteen clinical trials have been conducted in osteoarthritis, 14 of which yielded significant improvements in multiple disease parameters. Eight trials have been conducted in type 2 diabetes, all yielding significant improvement in clinical or laboratory outcomes. Three trials were in ulcerative colitis, two of which yielded significant improvement in at least one clinical outcome. Additionally, two clinical trials on rheumatoid arthritis, one clinical trial on lupus nephritis, and two clinical trials on multiple sclerosis resulted in inconclusive results. Longer duration, larger cohort size, and multiple dosage arm trials are warranted to establish the long term benefits of curcumin supplementation. Multiple mechanisms of action of curcumin on these diseases have been researched, including the modulation of the eicosanoid pathway towards a more anti-inflammatory pathway, and the modulation of serum lipid levels towards a favorable profile. Overall, curcumin supplementation emerges as an effective therapeutic agent with minimal-to-no side effects, which can be added in conjunction to current standard of care. -

Enzyme-Mediated Regioselective Acylations of Flavonoid Glycosides
FABAD j. P/ıarrıı. Sci., 20, 55-59, 1995 RESEARCH AR.TICLES /BİLİMSEL ARAŞTIRMALAR Enzyme-Mediated Regioselective Acylations of Flavonoid Glycosides Ihsan ÇALIŞ*t, Meltem ÖZİPEK*, Mcvlüt ERTAN**, Petcr RÜEDI*** Abstract: Flavonoid glycosides, xaııtlıorlıanınins B, C, a11d ru Flavouoit Glikozitlerirıiu Eıızinıatik Açilleunıesi tin lıaı~ been acylated by the catalytic actioıı of the protense sııbtilisi11 in aıılrydrous pyridine. The acylatioıı occııred ıoitlı Özet: Flavonoit glikozitlerinden ksantornnınin B, C ve rutin, lıiglı yield roitlı rutin giving a single monoester 011 its glııcose anlıidr piridinde proteaz subtilisin ile açillenmiştir. rııoicty Reaksiyo11 slıoıoing excellent selectivity. But it occııred witlı loıv 011 yield the galactose moiety of tJıe two flavonoid triglycosides. sonucunda, glukoz üzerinden rutinin nıonoesteri yüksek vcrinı Ie elde edilirken, galaktoz üzerinden flavonoit triglikozitleriııiıı Key words : Acylated f!avonoid glycosides, enzyrnatic acy- esterleri çok düşük verirnle elde edilmiştir. lation. Received : 29.6.1994 Anahtar kelinıeler : Ester flavonoit glikozit/er, enzhnatik Accepted : 19.1.1995 açillenıe Introduction the regioselective acylation of polyhydroxylated cornpounds3.4. Flavonoid glycosides are widely distributed in na ture and often found as esters with different acids at We now report on the substilisin-catalyzed esterifica specific positions of their sugar moieties. Besides tion of two flavonoid triglycosides isolated from these esters, the cinnamoyl, p-coumaroyl and feru Rhamnus petiolaris -

USP Reference Standards Catalog
Last Updated On: November 7, 2020 USP Reference Standards Catalog Catalog Status RS Name Current Previous Lot CAS # NDC # Unit Co. Of Material UN # Net Unit Commodity Special Pkg. USMCA KORUS Base Base # Lot (VUD) Price Origin Origin Weight Of Codes Restriction Type Eligible Eligible Control Control Measur (HS Codes)* Drug Drug % e 1000408 Active Abacavir Sulfate (200 R108M0 R028L0 (30- 188062- N/A $245.00 GB Chemical 200 mg 2933595960 No No mg) JUN-2020) 50-2 Synthesis 1000419 Active Abacavir Sulfate F0G248 188062- N/A $760.00 IN Chemical 20 mg 2933595960 No No Racemic (20 mg) (4- 50-2 Synthesis [2-amino-6- (cyclopropylamino)- 9H-purin-9yl]-2- cyclopentene-1- methanol sulfate (2:1)) 1000420 Active Abacavir Related F1L311 F0H284 (31- 906626- N/A $877.00 IN Chemical 20 mg 2933599550 No No Compound A (20 mg) OCT-2013) 51-5 Synthesis ([4-(2,6-diamino-9H- purin-9-yl)cyclopent- 2-enyl]methanol) 1000437 Active Abacavir Related F0M143 N/A N/A $877.00 IN Chemical 20 mg 2933599550 No No Compound D (20 mg) Synthesis (N6-Cyclopropyl-9- {(1R,4S)-4-[(2,5- diamino-6- chlorpyrimidin-4- yloxy)methyl] cyclopent-2-enyl}-9H- purine-2,6-diamine) 1000441 Active Abacavir Related F1L318 F0H283 (31- N/A N/A $877.00 IN Chemical 20 mg 2933599550 No No Compound B (20 mg) OCT-2013) Synthesis ([4-(2,5-diamino-6- chloropyrimidin-4- ylamino)cyclopent-2- enyl]methanol) 1000452 Active Abacavir Related F1L322 F0H285 (30- 172015- N/A $960.00 IN Chemical 20 mg 2933599550 No No Compound C (20 mg) SEP-2013) 79-1 Synthesis ([(1S,4R)-4-(2-amino- 6-chloro-9H-purin-9- yl)cyclopent-2- -

Biosynthesis of Food Constituents: Natural Pigments. Part 2 – a Review
Czech J. Food Sci. Vol. 26, No. 2: 73–98 Biosynthesis of Food Constituents: Natural Pigments. Part 2 – a Review Jan VELÍšEK, Jiří DAVÍDEK and Karel CEJPEK Department of Food Chemistry and Analysis, Faculty of Food and Biochemical Technology, Institute of Chemical Technology in Prague, Prague, Czech Republic Abstract Velíšek J., Davídek J., Cejpek K. (2008): Biosynthesis of food constituents: Natural pigments. Part 2 – a review. Czech J. Food Sci., 26: 73–98. This review article is a part of the survey of the generally accepted biosynthetic pathways that lead to the most impor- tant natural pigments in organisms closely related to foods and feeds. The biosynthetic pathways leading to xanthones, flavonoids, carotenoids, and some minor pigments are described including the enzymes involved and reaction schemes with detailed mechanisms. Keywords: biosynthesis; xanthones; flavonoids; isoflavonoids; neoflavonoids; flavonols; (epi)catechins; flavandiols; leu- coanthocyanidins; flavanones; dihydroflavones; flavanonoles; dihydroflavonols; flavones; flavonols; anthocya- nidins; anthocyanins; chalcones; dihydrochalcones; quinochalcones; aurones; isochromenes; curcuminoids; carotenoids; carotenes; xanthophylls; apocarotenoids; iridoids The biosynthetic pathways leading to the tetrapyr- restricted in occurrence to only a few families of role pigments (hemes and chlorophylls), melanins higher plants and some fungi and lichens. The (eumelanins, pheomelanins, and allomelanins), majority of xanthones has been found in basi- betalains (betacyanins and betaxanthins), and cally four families of higher plants, the Clusiaceae quinones (benzoquinones, naphthoquinones, and (syn. Guttiferae), Gentianaceae, Moraceae, and anthraquinones) were described in the first part of Polygalaceae (Peres et al. 2000). Xanthones can this review (Velíšek & Cejpek 2007b). This part be classified based on their oxygenation, prenyla- deals with the biosynthesis of other prominent tion and glucosylation pattern. -

Piper Methysticum)
Journal of Student Research (2015) Volume 4, Issue 2: pp. 69-72 Research Article A Closer Look at the Risks vs. Benefits of Kava (Piper methysticum) Anan A. Husseina If you took a trip to Fiji, the locals would probably welcome you with a drink of Kava. For centuries, the indigenous people of the South Pacific Islands have used the roots of a plant known as Kava. Beyond the use of Kava as a psychoactive substance, it has been incorporated as a cultural drink that is used in many ceremonies. In the late 1990’s Kava use spread quickly in Western countries including Europe, North America, and Australia. It was used as a treatment for anxiety. But just as quickly as it spread, the enthusiasm for it faded, because it was banned or restricted in many Western countries following reports of liver toxicity. In the United States, the Food and Drug Administration’s (FDA) concern for safety prompted a request for more research on the substance. The issues of safety and efficacy remain more specifically whether the benefits of using Kava outweigh the risks. History Kava is a beverage made from the roots of the plant included alcohol, cocaine, tobacco, and heroin. The findings Piper methysticum, and has been used historically in the suggest that kava may reduce the craving associated with the South Pacific Islands as a ceremonial drink. Kava was aforementioned substances, which may make kava a great introduced in Europe around the 1700s by Captain James future candidate to help with addiction. 13 Cook and has since spread widely to Australia, Europe, and Although the mechanism of action is not clear, it is the United States. -

Analysis of the Binding and Interaction Patterns of 100 Flavonoids with the Pneumococcal Virulent Protein Pneumolysin: an in Silico Virtual Screening Approach
Available online a t www.scholarsresearchlibrary.com Scholars Research Library Der Pharmacia Lettre, 2016, 8 (16):40-51 (http://scholarsresearchlibrary.com/archive.html) ISSN 0975-5071 USA CODEN: DPLEB4 Analysis of the binding and interaction patterns of 100 flavonoids with the Pneumococcal virulent protein pneumolysin: An in silico virtual screening approach Udhaya Lavinya B., Manisha P., Sangeetha N., Premkumar N., Asha Devi S., Gunaseelan D. and Sabina E. P.* 1School of Biosciences and Technology, VIT University, Vellore - 632014, Tamilnadu, India 2Department of Computer Science, College of Computer Science & Information Systems, JAZAN University, JAZAN-82822-6694, Kingdom of Saudi Arabia. _____________________________________________________________________________________________ ABSTRACT Pneumococcal infection is one of the major causes of morbidity and mortality among children below 2 years of age in under-developed countries. Current study involves the screening and identification of potent inhibitors of the pneumococcal virulence factor pneumolysin. About 100 flavonoids were chosen from scientific literature and docked with pnuemolysin (PDB Id.: 4QQA) using Patch Dockprogram for molecular docking. The results obtained were analysed and the docked structures visualized using LigPlus software. It was found that flavonoids amurensin, diosmin, robinin, rutin, sophoroflavonoloside, spiraeoside and icariin had hydrogen bond interactions with the receptor protein pneumolysin (4QQA). Among others, robinin had the highest score (7710) revealing that it had the best geometrical fit to the receptor molecule forming 12 hydrogen bonds ranging from 0.8-3.3 Å. Keywords : Pneumococci, pneumolysin, flavonoids, antimicrobial, virtual screening _____________________________________________________________________________________________ INTRODUCTION Streptococcus pneumoniae is a gram positive pathogenic bacterium causing opportunistic infections that may be life-threating[1]. Pneumococcus is the causative agent of pneumonia and is the most common agent causing meningitis.