Lacrimal Sac Pseudotumour – a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pediatric Orbital Tumors and Lacrimal Drainage System
Pediatric Orbital Tumors and Lacrimal Drainage System Peter MacIntosh, MD University of Illinois • No financial disclosures Dermoid Cyst • Congenital • Keratinized epidermis • Dermal appendage • Trapped during embryogenesis • 6% of lesions • 40-50% of orbital pediatric orbital lesion • Usually discovered in the first year of life • Painless/firm/subQ mass • Rarely presents as an acute inflammatory lesion (Rupture?) • Frontozygomatic (70%) • Maxillofrontal (20%) suture Imaging - CT • Erosion/remodeling of bone • Adjacent bony changes: “smooth fossa” (85%) • Dumbell dermoid: extraorbital and intraorbital components through bony defect Imaging - MRI • Encapsulated • Enhancement of wall but not lumen Treatment Options • Observation • Risk of anesthesia • Surgical Removal • Changes to bone • Rupture of cyst can lead to acute inflammation • Irrigation • Abx • Steroids Dermoid INFANTILE/Capillary Hemangioma • Common BENIGN orbital lesion of children • F>M • Prematurity • Appears in 1st or 2nd week of life • Soft, bluish mass deep to the eyelid • Superonasal orbit • Rapidly expands over 6-12 months • Increases with valsalva (crying) • Clinical findings • Proptosis Astigmatism • Strabismus Amblyopia INFANTILE/Capillary Hemangioma • May enlarge for 1-2 years then regress • 70-80% resolve before age 7 • HIGH flow on doppler • Kasabach-Merritt Syndrome • Multiple large visceral capillary hemangiomas • Sequestration of platelets into tumor • Consumptive thrombocytopenia • Supportive therapy and treat underlying tumor • Complications • DIC • death •Homogenous -

Stage Surgery on Inverted Papilloma Which Invaded Lacrimal Sac, Periorbita, Ethmoid and Frontal Sinus
臨床耳鼻:第 27 卷 第 1 號 2016 ••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••••• J Clinical Otolaryngol 2016;27:143-147 증 례 Stage Surgery on Inverted Papilloma which Invaded Lacrimal Sac, Periorbita, Ethmoid and Frontal Sinus Jae-hwan Jung, MD, Minsic Kim, MD, Sue Jean Mun, MD and Hwan-Jung Roh, MD, PhD Department of Otorhinolaryngology-Head & Neck Surgery, Pusan National University Yangsan Hospital, Yangsan, Korea - ABSTRACT - Inverted papilloma of the nasal cavity and the paranasal sinuses is a benign epithelial tumor with a high rate of recurrence, local aggressiveness, and malignant transformation. For these reasons, inverted papilloma has been treated like malignant tumors with extensive surgical resection. With the help of endoscopic sinus surgery tech- nique, it is now available to treat inverted papilloma with stage surgery without severe complications which usu- ally resulted from extensive one stage resection. We report a case of stage surgery on inverted papilloma which invaded lacrimal sac, periorbita, ethmoid and frontal sinus. (J Clinical Otolaryngol 2016;27:143-147) KEY WORDS:Inverted papillomaㆍLacrimal sacㆍPeriorbitaㆍSurgery. Authors present a successful endoscopic stage sur- Introduction gery on IP which invaded lacrimal sac, periorbita, ethmoid and frontal sinus with the literature review. Inverted papilloma (IP) of the nasal cavity and the paranasal sinuses is a benign epithelial tumor with a Case Report high rate of recurrence, local aggressiveness, and ma- lignant transformation.1,2) For these reasons, IP has A 41-year-old female presented in outpatient clinic been treated like malignant tumors with extensive sur- with a complaint of tender swelling mass on the in- gical resection. ner side of her right eye for 5 years which suddenly IP of lacrimal sac and periorbita is rarely reported aggravated 2 months ago. -

Anatomy of the Periorbital Region Review Article Anatomia Da Região Periorbital
RevSurgicalV5N3Inglês_RevistaSurgical&CosmeticDermatol 21/01/14 17:54 Página 245 245 Anatomy of the periorbital region Review article Anatomia da região periorbital Authors: Eliandre Costa Palermo1 ABSTRACT A careful study of the anatomy of the orbit is very important for dermatologists, even for those who do not perform major surgical procedures. This is due to the high complexity of the structures involved in the dermatological procedures performed in this region. A 1 Dermatologist Physician, Lato sensu post- detailed knowledge of facial anatomy is what differentiates a qualified professional— graduate diploma in Dermatologic Surgery from the Faculdade de Medician whether in performing minimally invasive procedures (such as botulinum toxin and der- do ABC - Santo André (SP), Brazil mal fillings) or in conducting excisions of skin lesions—thereby avoiding complications and ensuring the best results, both aesthetically and correctively. The present review article focuses on the anatomy of the orbit and palpebral region and on the important structures related to the execution of dermatological procedures. Keywords: eyelids; anatomy; skin. RESU MO Um estudo cuidadoso da anatomia da órbita é muito importante para os dermatologistas, mesmo para os que não realizam grandes procedimentos cirúrgicos, devido à elevada complexidade de estruturas envolvidas nos procedimentos dermatológicos realizados nesta região. O conhecimento detalhado da anatomia facial é o que diferencia o profissional qualificado, seja na realização de procedimentos mini- mamente invasivos, como toxina botulínica e preenchimentos, seja nas exéreses de lesões dermatoló- Correspondence: Dr. Eliandre Costa Palermo gicas, evitando complicações e assegurando os melhores resultados, tanto estéticos quanto corretivos. Av. São Gualter, 615 Trataremos neste artigo da revisão da anatomia da região órbito-palpebral e das estruturas importan- Cep: 05455 000 Alto de Pinheiros—São tes correlacionadas à realização dos procedimentos dermatológicos. -

TEAR PRODUCTION and DRAINAGE the Lacrimal Gland Is Located in the Superolateral Aspect of the Eyelid Below the Eyebrow(S)
Anatomy and Physiology 9 The conjunctiva is a mucous membrane that lines the upper and lower eyelids and extends over the sclera to the corneal margin. It contains lym- phoid tissue, which provides some immunology protection. It is innervated by CN V, the trigeminal nerve. The portion of the conjunctiva that covers the sclera is termed the bulbar conjunctiva; the portion covering the inner surface of the eyelids is termed the palpebral conjunctiva. Figure 1. Eyelid Muscles TEAR PRODUCTION AND DRAINAGE The lacrimal gland is located in the superolateral aspect of the eyelid below the eyebrow(s). It secretes watery (aqueous) tears and produces about 0.2 ml of tears in 24 hours. Aqueous tears flow downward and inward toward the tear drainage system at the inner canthus. In addition to aqueous tears, several glands located in the conjunctiva and eyelid margins secrete oily and sticky (mucous) tears. The meibomian glands are located within the tarsal plate of the eyelid and secrete oily tears. The glands of Zeiss, Moll, Wolfing, and Krause secrete sticky tears. These three types of tears provide moisture and protection to the surface of the eye(s). With each blink, tears are pushed across the eye toward the puncta located at the medial junction of the upper and lower eyelids. From the puncta, tears are pushed into the canaliculi and then into the lacrimal sac. 10 Essentials of Ophthalmic Nursing They are drained from the lacrimal sac and nasolacrimal duct to the inside of the nose and down the throat (see Figure 2). Figure 2. Lacrimal System TEAR FILM The tear film has three distinct layers. -

Acquired Etiologies of Lacrimal System Obstructions
5 Acquired Etiologies of Lacrimal System Obstructions Daniel P. Schaefer Acquired obstructions of the lacrimal excretory outfl ow system will produce the symptoms of epiphora, mucopurulent discharge, pain, dacryocystitis, and even cellulitis, prompting the patient to seek the ophthalmologist for evaluation and treatment. Impaired tear outfl ow may be functional, structural, or both. The causes may be primary – those resulting from infl ammation of unknown causes that lead to occlusive fi brosis—or secondary, resulting from infections, infl amma- tion, trauma, malignancies, toxicity, or mechanical causes. Secondary acquired dacryostenosis and obstruction may result from many causes, both common and obscure. Occasionally, the precise pathogenesis of nasolacrimal duct obstruction will, despite years of investigations, be elusive. To properly evaluate and appropriately treat the patient, the ophthal- mologist must have knowledge and comprehension of the lacrimal anatomy, the lacrimal apparatus, pathophysiology, ocular and nasal relationships, ophthalmic and systemic disease process, as well as the topical and systemic medications that can affect the nasolacrimal duct system. One must be able to assess if the cause is secondary to outfl ow anomalies, hypersecretion or refl ex secretion, pseudoepiphora, eyelid malposition abnormalities, trichiasis, foreign bodies and conjunctival concretions, keratitis, tear fi lm defi ciencies or instability, dry eye syn- dromes, ocular surface abnormalities, irritation or tumors affecting the trigeminal nerve, allergy, medications, or environmental factors. Abnormalities of the lacrimal pump function can result from involu- tional changes, eyelid laxity, facial nerve paralysis, or fl oppy eyelid syndrome, all of which displace the punctum from the lacrimal lake. If the cause is secondary to obstruction of the nasolacrimal duct system, the ophthalmologist must be able to determine where the anomaly is and what the cause is, in order to provide the best treatment possible for the patient. -

The Lacrimal System Terms
The Lacrimal System Lynn E. Lawrence, CPOT, ABOC, COA, OSC Terms • Etiology – the cause of a disease or abnormal condition • Dacryocystitis – inflammation of the lacrimal sac • Epiphora – watering of eyes due to excess secretion of tears or obstruction of the lacrimal passage Tear Film Layers oil aqueous snot What functions does each layer of the tear perform? Lacrimal System: Tear Film Layers LIPID DEFICIENCY ‐ evaporates TEAR DEFICIENCY – fails to hydrate properly oil aqueous snot What functions does each layer of the tear perform? What are functions of tears? Tear Components • Lipid Layer – prevents evaporation • Aqueous Layer ‐ hydration • Mucus Layer – sticks tear to the eye • Other components Lacrimal Apparatus • Sometimes a person cannot produce natural tears they might need punctal plugs to prevent the tears from draining off the eye. • Faucet • Action • Drain Obstructive – vs‐ non‐obstructive Tear Production – Secretory • Lacrimal gland – Reflex tearing – Too much tearing…epiphora • Gland of Krause – Superior fornix • Gland of Wolfring – Superior tarsal plate Two Primary Forms of Dry Eye 800 nm 8,000 nm 100 nm The two primary forms of dry eye are Evaporative Dry Eye, also known as Meibomian Gland Dysfunction or MGD and Aqueous Dry Eye. The majority of dry eye sufferers have MGD. Oil & Water Remember science class? Oil floats. Oil does not mix with water, but rather sits on top of water. Oil is what keeps water from evaporating. Need three volunteers TEST TIME http://optometrytimes.modernmedicine.com/optometrytimes/news/treating‐dry‐eye‐ lipid‐based‐eye‐drops Lipid Secretion: Meibomian Glands Left: Transillumination of eyelid showing meibomian glands Right: Secretion of lipid at lid margin • The lipid layer restricts evaporation to 5‐10% of tear flow – Also helps lubricate Mucin Secretion: Goblet Cells Superficial layer of bulbar conjunctiva. -
Inferior Oblique Muscle of the Eye: Its Fetal Development with Special Reference to Understanding of the Frequent Variants in Adults
ONLINE FIRST This is a provisional PDF only. Copyedited and fully formatted version will be made available soon. ISSN: 0015-5659 e-ISSN: 1644-3284 Inferior oblique muscle of the eye: its fetal development with special reference to understanding of the frequent variants in adults Authors: Z. W. Jin, S. Umeki, Y. Takeuchi, M. Yamamoto, G. Murakami, S. Abe, J. F. Rodríguez-Vázquez DOI: 10.5603/FM.a2021.0043 Article type: Original article Submitted: 2021-03-13 Accepted: 2021-04-09 Published online: 2021-04-28 This article has been peer reviewed and published immediately upon acceptance. It is an open access article, which means that it can be downloaded, printed, and distributed freely, provided the work is properly cited. Articles in "Folia Morphologica" are listed in PubMed. Powered by TCPDF (www.tcpdf.org) Inferior oblique muscle of the eye: its fetal development with special reference to understanding of the frequent variants in adults Z.W. Jin et al., Development of the inferior obliquus Z.W. Jin1, S. Umeki2, Y. Takeuchi2, M. Yamamoto2, G. Murakami2, 3, S. Abe2, J.F. Rodríguez-Vázquez4 1Department of Anatomy, Wuxi School of Medicine, Jiangnan University, Wuxi, China 2Department of Anatomy, Tokyo Dental College, Tokyo, Japan 3Division of Internal Medicine, Cupid Clinic, Iwamizawa, Japan 4Department of Anatomy and Embryology, School of Medicine, Complutense University, Madrid, Spain Address for correspondence: Z.W. Jin, MD, PhD, Department of Anatomy, Wuxi School of Medicine, Jiangnan University, 1800 Lihu Avenue, Wuxi, Jiangsu, 214122, China, tel: +86-510-8519-7079, fax: +86-510-8519-3570, e-mail: [email protected] ABSTRACT To provide better understanding of frequent variations of the inferior oblique (IO) of adult extraocular muscles, we observed sagittal and horizontal histological sections of the eye and orbits from 32 fetuses (approximately 7-34 weeks of gestational age; 24-295 mm of crown-rump length). -

Malignant Melanoma of the Lacrimal Sac: Case Report and Major Review with Treatment Update
Journal of Ophthalmology & Visual Neurosciences Case report Malignant Melanoma of the Lacrimal Sac: Case Report and Major Review with Treatment Update This article was published in the following Scient Open Access Journal: Journal of Ophthalmology & Visual Neurosciences Received November 28, 2016; Accepted December 10, 2016; Published December 20, 2016 Lindsay A McGrath1,2 and Stephen B O’Hagan1,3* Abstract 1 Cairns Base Hospital, Ophthalmology Department, Purpose: To present a rare case of Primary Lacrimal Sac Melanoma, and review all Queensland 4870, Australia 2University of Queensland, Brisbane, Queensland reports of this condition in the literature to date. 4072, Australia Methods: In this review the clinical characteristics, presenting symptoms, treatment 3James Cook University, Cairns, Queensland, and morbidity of all patients with lacrimal sac melanoma reported in the literature from 1926 Australia to the present. We have also discussed new approaches available for adjuvant radiotherapy in the context of this frequently recurrent tumour. Results: Primary Melanoma of the Lacrimal Sac is a rare disease which is frequently diagnosed late. Common presenting symptoms include epiphora, blood-stained tears and painless swelling. Intensity modulated radiation therapy appears to hold promise in the adjuvant treatment of this disease, to reduce morbidity and mortality from recurrence and/ or metastasis. Conclusions: Existing case series and reports of Lacrimal Sac Melanoma describe a variety of treatment regimens and poor follow-up - highlighting the lack of a widely accepted strategy to prevent recurrence of disease. This case and review reminds practitioners of presenting signs and symptoms that should raise suspicion of Lacrimal Sac Melanoma, and a contemporary approach to adjuvant radiation therapy. -

Table 1-1 Bones of the Orbit
6 ● Neuro-Ophthalmology Planum sphenoidale Superior orbital fissure Optic canal Tuberculum sella Cavernous Anterior clinoid Pituitary sinus fossa Foramen ovale Carotid canal Foramen spinosum Foramen lacerum Clivus Petrous portion Dorsum sella of temporal bone Figure 1-3 Parasellar bony anatomy demonstrates the relationship of the pituitary fossa to the cavernous sinus, including the foramina of the skull base. The foramen lacerum is filled with cartilage and contains the artery of the pterygoid canal, the nerve of the pterygoid canal, and the venous drainage structures. The carotid artery enters the skull base through the carotid canal. (Courtesy of Albert L. Rhoton Jr, MD.) Frontal bone Lesser wing of sphenoid bone Superior orbital Optic canal fissure Greater wing of Ethmoidal bone sphenoid bone Lacrimal bone Zygomatic bone Lacrimal sac Palatine bone fossa Inferior orbital Maxillary bone fissure Figure 1-4 Anatomy of the orbit. Bony anatomy of the right orbital apex. The optic canal trans- mits the optic nerve, ophthalmic artery, and some oculosympathetic fibers. The superior orbital fissure, between the greater and lesser wings of the sphenoid bone, transmits CNs III, IV, and VI; the ophthalmic division of CN V (CN V1); the oculosympathetics; and the superior ophthalmic vein. (Illustration by Dave Peace.) Table 1-1 Bones of the Orbit Orbital Roof Lateral Wall Orbital Floor Medial Wall Frontal Zygomatic Zygomatic Maxillary Lesser wing of sphenoid Greater wing of sphenoid Maxillary Lacrimal Palatine Ethmoid Lesser wing of sphenoid CHAPTER 1: Neuro- Ophthalmic Anatomy ● 7 The superior orbital rim is made up of the frontal bone, which connects to the zygomatic bone laterally at the frontozygomatic suture. -

Apocrine Adenocarcinoma of Lacrimal Sac Presenting As Chronic Dacryocystitis
Hoang A, et al., J Ophthalmic Clin Res 2017, 4: 027 DOI: 10.24966/OCR-8887/100027 HSOA Journal of Ophthalmology and Clinical Research Case Report past three months. In the summer of 2014, the patient first noticed Apocrine Adenocarcinoma of a cystic lesion in the right medial canthus which he attributed to an eye infection after swimming in a hot tub. Around December 2014, Lacrimal Sac Presenting as he developed conjunctival injection and discharge and was prescribed Cephalexin by his primary ophthalmologist. His symptoms improved Chronic Dacryocystitis with antibiotics but he continued to have redness and discharge. He denied loss of vision or ocular pain. Past medical history was unre- Amber Hoang1*, Kay T Khine2 and Renzo Zaldivar2 markable. Ophthalmic examination at our institution revealed a firm 1Department of Internal Medicine, New Hanover Regional Medical Center, ulcerative nodule at the right medial canthus above the medial can- Wilmington, North Carolina, USA thus tendon with erythema and spontaneous pus drainage (Figure 2Department of Ophthalmology, University of North Carolina School of 1A). Visual acuity was normal and intraocular pressure was 21mmHg Medicine, Kittner Eye Center, Chapel Hill, North Carolina, USA OD. The patient was placed on Sulfamethoxazole and Trimethoprim. Culture of the pus drainage was positive for coagulase-negative Staph- ylococcus aureus species. Abstract The objective of this paper is to report a case of lacrimal apo- crine adenocarcinoma which presented as chronic dacryocystitis. A 62-year-old male was referred by his primary ophthalmologist for evaluation of chronic dacryocystitis of the right eye for 3 months. Biopsy showed a rare and aggressive type of cancer: apocrine ad- enocarcinoma of the nasolacrimal sac and paranasal sinuses. -
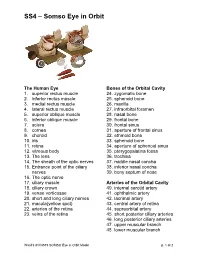
SS4 – Somso Eye in Orbit
SS4 – Somso Eye in Orbit The Human Eye Bones of the Orbital Cavity 1. superior rectus muscle 24. zygomatic bone 2. inferior rectus muscle 25. sphenoid bone 3. medial rectus muscle 26. maxilla 4. lateral rectus muscle 27. infraorbital foramen 5. superior oblique muscle 28. nasal bone 6. inferior oblique muscle 29. frontal bone 7. sclera 30. frontal sinus 8. cornea 31. aperture of frontal sinus 9. choroid 32. ethmoid bone 10. iris 33. sphenoid bone 11. retina 34. aperture of sphenoid sinus 12. vitreous body 35. pterygopalatina fossa 13. The lens 36. trochlea 14. The sheath of the optic nerves 37. middle nasal concha 15. Entrance point of the ciliary 38. inferior nasal concha nerves 39. bony septum of nose 16. The optic nerve 17. ciliary muscle Arteries of the Orbital Cavity 18. ciliary crown 40. internal carotid artery 19. venae vorticosae 41. ophthalmic artery 20. short and long ciliary nerves 42. lacrimal artery 21. macula(yellow spot) 43. central artery of retina 22. arteries of the retina 44. supraorbital artery 23. veins of the retina 45. short posterior ciliary arteries 46. long posterior ciliary arteries 47. upper muscular branch 48. lower muscular branch Ward’s 81V3519 SOMSO Eye in Orbit Model p. 1 of 2 SS4 – Somso Eye in Orbit 49. posterior ethmoid artery 83. branch communication with 50. anterior ethmoid artery nasociliary nerve 51. upper palpebral artery 52. supratrochlear artery The Lacrimal Organs with 53. posterior communicating Eyelid Supports artery 1. lacrimal gland 54. anterior cerebral artery 2. upper part 55. cavernous sinus and internal 3. lower part carotid artery 4. -

Anatomy and Physiology of the Nasolacrimal Ducts 1
ChapterAnatomy and 1 Physiology of the Nasolacrimal Ducts Chapter 1 1 Anatomy and Physiology of the Nasolacrimal Ducts 1 Friedrich Paulsen Core Messages! Q The lacrimal sac and nasolacrimal duct are surrounded by a cavernous body. While Q The tear film is produced by the lacrimal regulating the blood flow, the specialized gland and the different structures of the eye blood vessels permit opening and closing of lid. Its composition is controlled by the the lumen of the lacrimal passage affected by lacrimal functional unit. the bulging and subsiding of the cavernous body, while at the same time regulating tear Q The ocular surface epithelia together with outflow. The blood vessels are connected to the lacrimal gland produce a unique subset the vessels of the outer eye and could act as a of membrane bound and secretory mucins feedback signal for tear-fluid production. that stabilize the tear film, fix it to the epithelia, support binding of bacteria, and are of great importance to tear physiology. Q TFF peptides TFF1 and TFF3 of conjunctival Contents origin influence the rheological properties of 1.1 Introduction ................................... 1 the tear film. 1.2 Anatomy and Physiology Q Drainage of tears involves a number of of the Ocular Surface and Adnexa ................ 2 1.2.1 Ocular Surface ................................. 3 different mechanisms; of these the action of 1.2.2 Lacrimal Gland ................................ 4 the lacrimal part of the orbicularis oculi 1.2.3 Eyelid ......................................... 4 muscle is most important to bring tear fluid 1.2.4 The Lacrimal Functional Unit .................... 5 into the lacrimal sac. Epithelial secretion 1.3 Anatomy and Physiology products, the surrounding cavernous body, of the Nasolacrimal Ducts ......................