Sex-Specific Innate Immune Selection of HIV-1 in Utero Is Associated With
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wooltru Healthcare Fund Optical Network List Gauteng
WOOLTRU HEALTHCARE FUND OPTICAL NETWORK LIST GAUTENG PRACTICE TELEPHONE AREA PRACTICE NAME PHYSICAL ADDRESS CITY OR TOWN NUMBER NUMBER ACTONVILLE 456640 JHETAM N - ACTONVILLE 1539 MAYET DRIVE ACTONVILLE 084 6729235 AKASIA 7033583 MAKGOTLOE SHOP C4 ROSSLYN PLAZA, DE WAAL STREET, ROSSLYN AKASIA 012 5413228 AKASIA 7025653 MNISI SHOP 5, ROSSLYN WEG, ROSSLYN AKASIA 012 5410424 AKASIA 668796 MALOPE SHOP 30B STATION SQUARE, WINTERNEST PHARMACY DAAN DE WET, CLARINA AKASIA 012 7722730 AKASIA 478490 BODENSTEIN SHOP 4 NORTHDALE SHOPPING, CENTRE GRAFENHIEM STREET, NINAPARK AKASIA 012 5421606 AKASIA 456144 BODENSTEIN SHOP 4 NORTHDALE SHOPPING, CENTRE GRAFENHIEM STREET, NINAPARK AKASIA 012 5421606 AKASIA 320234 VON ABO & LABUSCHAGNE SHOP 10 KARENPARK CROSSING, CNR HEINRICH & MADELIEF AVENUE, KARENPARK AKASIA 012 5492305 AKASIA 225096 BALOYI P O J - MABOPANE SHOP 13 NINA SQUARE, GRAFENHEIM STREET, NINAPARK AKASIA 087 8082779 ALBERTON 7031777 GLUCKMAN SHOP 31 NEWMARKET MALL CNR, SWARTKOPPIES & HEIDELBERG ROAD, ALBERTON ALBERTON 011 9072102 ALBERTON 7023995 LYDIA PIETERSE OPTOMETRIST 228 2ND AVENUE, VERWOERDPARK ALBERTON 011 9026687 ALBERTON 7024800 JUDELSON ALBERTON MALL, 23 VOORTREKKER ROAD, ALBERTON ALBERTON 011 9078780 ALBERTON 7017936 ROOS 2 DANIE THERON STREET, ALBERANTE ALBERTON 011 8690056 ALBERTON 7019297 VERSTER $ VOSTER OPTOM INC SHOP 5A JACQUELINE MALL, 1 VENTER STREET, RANDHART ALBERTON 011 8646832 ALBERTON 7012195 VARTY 61 CLINTON ROAD, NEW REDRUTH ALBERTON 011 9079019 ALBERTON 7008384 GLUCKMAN 26 VOORTREKKER STREET ALBERTON 011 9078745 -

1996 Masters Outdoor Championship
MastersTrack.com: 1996 USATF National Masters Outdoor Championships, Spokane, W... Page 1 of 52 USATF 1996 National Masters Outdoor Track & Field Championship Hosted by Spokane Sports Unlimited Spokane Falls Community College - Spokane, WA Thursday Aug 15, 1996 to Sunday Aug 18, 1996 National Masters Results - Men M30+ 100 Meter Dash AGE GRA. Finals Results - Sunday 08/18/96 PLACE ATHLETE NAME AGE HOMETOWN TIME AGE-GRADED MARK ===== ================================= ============== 1 Stan Whitley M50 Alta Loma, CA 10.38 1.3 9.27 106.36% 2 Milton Silverstein M76 Tuscon, AZ 10.73 1.3 7.83 125.91% 3 James Stookey M66 Dickerson, MD 10.92 1.3 8.78 112.36% 4 Kevin Morning M40 Orangevale, CA 10.93 1.3 10.43 94.51% 5 Marion McCoy M46 Atlanta, GA 11.40 1.3 10.53 93.68% M30+ 100 Meter Dash FINALS Finals Results - Saturday 08/17/96 PLACE ATHLETE NAME AGE HOMETOWN TIME HT AGE-GRADED MARK ===== ================================= ================= ------------ Men 30 ------------- - *Paul Scarlett M33 Portland, OR 11.01 1.5 11 11.01 89.55% 1 David Barmer M32 Glendale, CO 11.03 1.5 11 11.03 89.39% 2 Brett Lawler M32 Sarasota, FL 11.35 1.5 11 11.35 86.87% 3 Joe Ngassa M32 Provo, UT 11.52 1.5 11 11.52 85.59% 4 Richard Washington M33 Scotch Plains, NJ 11.89 1.5 11 11.89 82.93% 5 Gregory Font M34 Mount Lake Terrace, WA 12.20 1.5 11 12.20 80.82% ------------ Men 35 ------------- 1 Martin Krulee M39 Campbell, CA 11.03 -1.1 10 10.88 90.66% 2 Derek Holloway M35 Sicklerville, NJ 11.22 -1.1 10 11.07 89.13% 3 Eugene Vickers M35 Bel Air, MD 11.26 -1.1 10 11.11 88.81% -
Gauteng Property Portfolio
GAUTENG PROPERTY PORTFOLIO BELONG. MORNINGSIDE One-of-a-kind, secure and spacious triple-storey, corner penthouse apartment, with uninterrupted 270-degree views. Refrigerated walk-in wine room, 4 palatial bedrooms with the wooden floor theme continued, with marble covered en suite bathrooms and a state-of-the-art home cinema with top-of-the-range AV equipment. Numerous balconies, all with views, with a heated pool and steam-room on the roof. R39.5 MILLION MORNINGSIDE, Gauteng Ref# HP1139604 WAYNE VENTER 073 254 1453 Best Real Estate Agency 2015 South Africa and Africa Best Real Estate Agency Website 2015 South Africa and Africa / pamgolding.co.za pamgolding.co.za EXERCISE YOUR FREEDOM 40KM HORSE RIDING TRAILS Our ultra-progressive Equestrian Centre, together with over 40 kilometres of bridle paths, is a dream world. Whether mastering an intricate dressage movement, fine-tuning your jump approach, or enjoying an exhilarating outride canter, it is all about moments in the saddle. The accomplished South African show jumper, Johan Lotter, will be heading up this specialised unit. A standout health feature of our Equestrian Centre is an automated horse exerciser. Other premium facilities include a lunging ring, jumping shed, warm-up arena and a main arena for show jumping and dressage events. The total infrastructure includes 36 stables, feed and wash areas, tack- rooms, office, medical rooms and groom accommodation. Kids & Teens Wonderland · Sport & Recreation · Legendary Golf · Equestrian · Restaurants & Retail · Leisure · Innovative Infrastructure -

Directions to 36 Klip Street Observatory
Directions to 36 Klip Street Observatory JHB 26°10'29.58"S – 28° 5'12.43"E Contact number: 011 – 648 6001 From Pretoria / Durban / JHB. Int. Airport From Sandton / Bloemfontein / Soweto From Johannesburg CBD PTA : R21 south (towards JHB Int. Airport) SAN : M1 south (towards JHB CBD) M9 Rissik north Off-ramp Riviera or N1 south (towards JHB) Top off-ramp left (M16 Riviera) N3 south (towards Durban) Traffic light (T-junction) right (M31 West) R24 west (towards JHB) Traffic light left (M16 1 st Avenue) DBN : N3 north (towards JHB) BFT/Soweto : N1 north (towards JHB) R24 west (towards JHB) M1 north (towards JHB) Off-ramp 1 st Avenue JHB International Airport : Traffic light straight (M16 1 st Avenue) R24 west (towards JHB) Follow the whole of 1 st Avenue Pass Metropolitan Centre 2nd traffic light right (Queen/Friedland) (Loveday – Hoofd – Joubert) At the end there is a funny turn to the right Traffic light right (M71 Empire) Traffic light right (M11 Louis Botha) 2nd traffic light left (M11 Louis Botha) After ± 2 km at circle left (Louise) Traffic light left (Acorn) 8th traffic light right (Acorn) T-junction left (St. Peter) T-junction left (St. Peter) Immediately right (Bezuidenhout) Immediately right (Bezuidenhout) Immediately left (Eckstein) Immediately left (Eckstein) At Sacred Heart College right (Innes) At Sacred Heart College right (Innes) 2nd road left (St. Georges) 2nd road left (St. Georges) Enter Observatory Estate enclosure Enter Observatory Estate enclosure Enter Observatory Estate enclosure At circle take 3 rd exit (Bessie) 3rd -

M1 Cnr Anerley Rd & 3Rd Ave, Parktown M1
CNR ANERLEY RD & 3RD AVE, PARKTOWN S26 10.221’ E028 02.896’ N1 Riviera DOUGLASDALE SUNNINGHILL RIVONIA M1 NORTH BUCCLEUCH 17 JOHANNESBURG RIDING N1 MORNINGSIDE SANDOWN M16 Riviera Rd N3 SANDTON RANDBURG C INANDA MODDERFONTEIN SANDHURST Killarney ATHOL Mall DUNKELD M1 LINDEN OR Tambo ROSEBANK NORWOOD International M1 Airport 16 JOHANNESBURG NORTHCLIFF B F M31/Houghton/Joe Slovo PARKTOWN Brenthust PARKVIEW (Harry Oppenheimer’s NORTH African Library) N1 BRAAMFONTEIN KENSINGTON AASTROTECH STROTECH E N12 BEDFORD- JOHANNESBURG VIEW CONFERENCE CENTRE THE M2 WILDS N3 TURFONTEIN The A Pines Johannesburg Killarney 15 JOHANNESBURG Hospital M9 Oxford Rd Roedean N12 Parktown N1 M1 St Johns College Sunnyside Johannesburg Park Hotel College of Education at Wits SHERBORNE RD Wits Graduate School of Business M1 D University of Witwatersrand West Campus Braamfontein A FROM M1 (SOUTH) OXFORD ROAD OFFRAMP B FROM M1 (NORTH) HOUGHTON DR/JOE SLOVO DR OFFRAMP Travel on the M1 in a northerly direction and take the M9 Oxford Rd Travel on the M1 Highway in a southerly direction, take the M31 Houghton Offramp. Continue along Oxford Rd and then turn right into Anerley Rd Dr/Joe Slovo Offramp. At the first traffic light after you come off the (which is directly after the Holy Family College). Travel over the bridge Highway, turn right onto Newtown Ave. Continue along Newtown Ave, spanning the M1 until you see the AstroTech Conference Centre on the crossing over a traffic circle, until you reach a T-Junction, where you will left. turn left into Anerley Rd. The AstroTech Conference Centre is immediately on your left. -
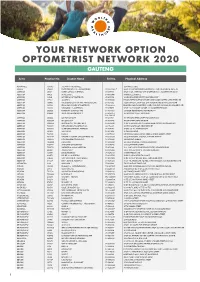
Your Network Option Optometrist Network 2020 Gauteng
YOUR NETWORK OPTION OPTOMETRIST NETWORK 2020 GAUTENG Area Practice No. Doctor Name Tel No. Physical Address ACTONVILLE 456640 JHETAM N - ACTONVILLE 1539 MAYET DRIVE AKASIA 478490 ENGELBRECHT A J A - WONDERPARK 012 5490086/7 SHOP 404 WONDERPARK SHOPPING C, CNR OF HEINRICH AVE & OL ALBERTON 58017 TORGA OPTICAL ALBERTON 011 8691918 SHOP U 142, ALBERTON CITY SHOPPING MALL, VOORTREKKER ROAD ALBERTON 141453 DU PLESSIS L C 011 8692488 99 MICHELLE AVENUE ALBERTON 145831 MEYERSDAL OPTOMETRISTS 011 8676158 10 HENNIE ALBERTS STREET, BRACKENHURST ALBERTON 177962 JANSEN N 011 9074385 LEMON TREE SHOPPING CENTRE, CNR SWART KOPPIES & HEIDELBERG RD ALBERTON 192406 THEOLOGO R, DU TOIT M & PRINSLOO C M J 011 9076515 ALBERTON CITY, SHOP S03, CNR VOORTREKKER & DU PLESSIS ROAD ALBERTON 195502 ZELDA VAN COLLER OPTOMETRISTS 011 9002044 BRACKEN GARDEN SHOPPING CNTR, CNR DELPHINIUM & HENNIE ALBERTS STR ALBERTON 266639 SIKOSANA J T - ALBERTON 011 9071870 SHOP 23-24 VILLAGE SQUARE, 46 VOORTREKKER ROAD ALBERTON 280828 RAMOVHA & DOWLEY INC 011 9070956 53 VOORTREKKER ROAD, NEW REDRUTH ALBERTON 348066 JANSE VAN RENSBURG C Y 011 8690754/ 25 PADSTOW STREET, RACEVIEW 072 7986170 ALBERTON 650366 MR IZAT SCHOLTZ 011 9001791 172 HENNIE ALBERTS STREET, BRACKENHURST ALBERTON 7008384 GLUCKMAN P 011 9078745 1E FORE STREET, NEW REDRUTH ALBERTON 7009259 BRACKEN CITY OPTOMETRISTS 011 8673920 SHOP 26 BRACKEN CITY, HENNIE ALBERTS ROAD, BRACKENHURST ALBERTON 7010834 NEW VISION OPTOMETRISTS CC 090 79235 19 NEW QUAY ROAD, NEW REDRUTH ALBERTON 7010893 I CARE OPTOMETRISTS ALBERTON 011 -

An Overview of Rural Change in Africa
~ " Rural Futures P ·ogramn1 TRANSFORMING AFRICA A NEW EMERGING RURAL WORLD An Overview of Rural Change in Africa z nd edition , .... ..cc BY NC ND https://creativecommons.org/hcenses/by-nc-nd/4.0/deed.en Juty2016 The Cirad the NEPAD Agency. rights owners. authorize the use of the original work for non-commercial purposes. but does not authorize the creation ofderivat ive works. Cover Photo : Geneviève Cortes Printîng : lmp:Actlmprimerîe. Saint Gelydu Fesc (34 - France) ISBN: 978-2-87614-719-5 An Overview of Rural Change in Africa znd edition A NEW EMERGING RURAL WORLD An Overview of Rural Change in Africa 2nd edition Citation: Pesche D .. Losch B. lmbernon J. (Eds.l. 2016. A New Emerging Rural World. An OverviewofRural Change inAfrica. Atlas for the NEPAD Rural Futures Programme. Second Edition. Revised and Enlarged. Montpellier. Cirad. NEPAD Agency. 76 p. This atlas on rura l change in Africa. for this second edition. revised and enlarged. was prepared at the request oft he NEPAD Agency and un der t he overall coordination and guidance of Ibrahim Assane Mayaki, NEPAD Agency CEO. Estherine Lisinge Fotabong. Programme lmplementation and Coordination Director. lt is part of the partnership between Ci rad and NEPAD and benefited from the financial support of NEPAD. AFD and Cirad. Conceived to inform research and discussions during the Second Africa Rural Development Forum (ARDF) held in Yaoundé. Cameroun. from 8 to 10 September 2016. it contributes to the work of the NEPAD Rural Futures programme. The completion of t he atlas has involved 52 aut hors whose detailed list is provided on page 73. -

36927 18-10 Roadcarrierp P1 Layout 1
Government Gazette Staatskoerant REPUBLIC OF SOUTH AFRICA REPUBLIEK VAN SUID-AFRIKA October Vol. 580 Pretoria, 18 2013 Oktober No. 36927 PART 1 OF 4 N.B. The Government Printing Works will not be held responsible for the quality of “Hard Copies” or “Electronic Files” submitted for publication purposes AIDS HELPLINE: 0800-0123-22 Prevention is the cure 305096—A 36927—1 2 No. 36927 GOVERNMENT GAZETTE, 18 OCTOBER 2013 IMPORTANT NOTICE The Government Printing Works will not be held responsible for faxed documents not received due to errors on the fax machine or faxes received which are unclear or incomplete. Please be advised that an “OK” slip, received from a fax machine, will not be accepted as proof that documents were received by the GPW for printing. If documents are faxed to the GPW it will be the sender’s respon- sibility to phone and confirm that the documents were received in good order. Furthermore the Government Printing Works will also not be held responsible for cancellations and amendments which have not been done on original documents received from clients. CONTENTS INHOUD Page Gazette Bladsy Koerant No. No. No. No. No. No. Transport, Department of Vervoer, Departement van Cross Border Road Transport Agency: Oorgrenspadvervoeragentskap aansoek- Applications for permits:.......................... permitte: .................................................. Menlyn..................................................... 3 36927 Menlyn..................................................... 3 36927 Applications concerning Operating Aansoeke -
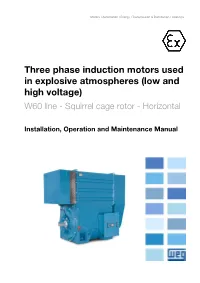
Three Phase Induction Motors Used in Explosive Atmospheres (Low and High Voltage)
Motors I Automation I Energy I Transmission & Distribution I Coatings Three phase induction motors used in explosive atmospheres (low and high voltage) W60 line - Squirrel cage rotor - Horizontal Installation, Operation and Maintenance Manual Installation, Operation and Maintenance Manual Document Number: 12868530 Model: W60 Language: English Revision: 11 July 2020 www.weg.net Dear Customer, Thank you for purchasing a WEG motor. Our products are developed with the highest standards of quality and efficiency which ensures outstanding performance. Since electric motors play a major role in the comfort and well-being of mankind, it must be identified and treated as a driving machine with characteristics that involve specific care, such as proper storage, installation and maintenance All efforts have been made to ensure that the information contained in this manual is faithful to the configurations and applications of the motor. Therefore, we recommend that you read this manual carefully before proceeding with the installation, operation or maintenance of the motor in order to ensure safe and reliable operation of your equipment and facility. If you need any further information, please contact WEG. Always keep this manual close to the motor, so that it can be consulted whenever necessary. ATTENTION 1. It is imperative to follow the procedures contained in this manual for the warranty to be valid; 2. The motor installation, operation and maintenance procedures must be performed only by qualified personnel. NOTES 1. The total or partial reproduction of information supplied in this manual is authorized, provided that reference is made to its source. If this manual is lost, an electronic PDF file is available at www.weg.net or another printed copy may be requested. -

[email protected] from DURBAN F
DOVES PINETOWN SUITE 4, 79 CROMPTON STREET PINETOWN CONTACT NUMBER : 031 – 7024498 EMAIL: [email protected] FROM DURBAN Head north on Joe Slovo St toward Monty Naicker Rd Turn left at the 1st cross street onto Monty Naicker Rd Continue onto N3 Take exit 17 for M13 toward Pinetown/Pietermaritzburg Merge onto King Cetshwayo Hwy Take the exit toward St Johns ave Keep left Keep right At the roundabout, take the 3rd exit Continue onto Underwood Rd Turn right onto Caversham Rd Continue onto Crompton St Destination will be on the left FROM HILLCREST : Head west on Tygerberg Valley Rd/M13 toward Tygerberg Valley Rd/M13 At the roundabout, take the 1st exit onto Plattekloof Rd/M14 Turn left to merge onto N1 toward Paarl Merge onto N1 Partial toll road At the roundabout, take the 3rd exit onto Donkin St/N1/N12 Continue to follow N1 Partial toll road Take the ramp to N5/R708 Turn right onto N5/R708 Continue to follow N5 Turn right onto N5/R26 Continue to follow N5 Merge onto N3 Partial toll road Keep right to stay on N3 Keep right to stay on N3 Partial toll road Take exit 20 to merge onto M7 toward Pinetown/New Germany/M19 Continue onto St Johns Ave/M19 Turn left onto Josiah Gumede Rd Turn right onto Crompton St Destination will be on the left FROM CLERMONT Head east on Kings Rd toward 36th Ave Kings Rd turns slightly right and becomes 36th Ave Turn right at Clermont Rd Turn right onto Clermont Rd Continue onto Posselt Rd Turn left toward Otto Volek Rd Slight left onto Otto Volek Rd Continue onto M5 Turn right to merge onto M19 Turn right onto -

Theologian, Musician, Author and Educator
Theologian, Musician, Author and Educator The gift collections of Dr. Jon Michael Spencer A Catalogue of Books, Microfilm, Journals and Vertical Files Donated to the L. Douglas Wilder Library Virginia Union University Compiled by Suzanne K. Stevenson, Special Collections Librarian Michelle A. Taylor, Technical Services Librarian Library Bibliography Series ©Spring 2002 1 PREFACE Since 1998, Dr. Jon Michael Spencer has donated more than 1,100 books from his personal research library as well as selected journals, microfilm of historic papers and research documentation to the L. Douglas Wilder Library at Virginia Union University. The subject areas reflect his specialties in the history and theology of African-American sacred and secular music, African history and slave culture, and African-American history and sociology. The collection includes a significant number of hymnals from various denominations. The former University of Richmond music and American studies professor is now a professor of religious studies at the University of South Carolina. He earned a music degree from Hampton University and completed graduate work in music composition as well as theology at Washington University and Duke Divinity School. Spencer donated this extensive collection to VUU for several reasons. Until the summer 2000, he was a resident of Richmond and VUU was the city’s African American university. As well, VUU has a School of Theology and Spencer has published extensively in the area of religion. Finally, his architect father, John H. Spencer, participated in the design of the Wilder library. It is in the elder Spencer’s name that Dr. Spencer has donated his collections. The books are housed in the library’s closed collections. -

How to Find Ebm-Papst in South Africa
ebm-papst South Africa (Pty) Ltd. How to find ebm-papst 1119 Yacht Avenue Laser Park, Honeydew Extension 20 in South Africa ZA-2040 Honeydew, Johannesburg Phone +27 11 794 3434 Fax +27 11 794 5020 E-Mail:[email protected] www.ebmpapst.co.za 1/3 B ey er s N au B de ey er s N au de R564 Citrus St. Beyers Naude Dr. Blueberry Rd. d R y r r e b e M6 u l B Braam St. Vlootboot St. Vragboot St. Windjammer St. Yacht Av. N1 Beyers Naude Dr. R564 JOHANNESBURG • From the N1 north turn left into Beyers Naude (M5). Turn left into Blueberry road and then right into Braam street. First left into Yacht avenue, we are the third building on the right. • From the N1 south turn right into Beyers Naude (M5). Turn left into Blueberry road and then right into Braam street. First left into Yacht avenue, we are the third building on the right. ebm-papst South Africa (Pty) Ltd How to find ebm-papst Unit no 1, Marconi Park, 11 Marconi Crescent in Cape Town Montague Gardens ZA-7441 Cape Town Phone +27 21 555 4547 Fax +27 21 551 2854 [email protected] www.ebmpapst.co.za 2/3 Omuramba Road Marconi Crescent Marconi Road Montague e iv r Gardens D e u g ta n o M N7 Montague Drive Marconi Beam N7 Marconi Beam Freedom Way Montague Drive MILNERTON N1 N1 ad Ro am nd ma Bos ✈ M7 R102 • From N7, Take the M8, Milnerton turn off.