Rasayana: Ayurvedic Herbs for Longevity and Rejuvenation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effect of Rasayana Therapy on Ageing: an Ayurvedic Perspective1
Effect of Rasayana Therapy on Ageing: An Ayurvedic Perspective1 R.D.H Kulatunga * Abstract Ageing is a multidimensional process of physical, psychological and social change. Ayurveda Rasayana2 therapy has given powerful contribution to overcome age related disorders and act essentially on nutrition dynamics and rejuvenate the body and the mind. The present study has been carried out to assess the effect of Guduchyadi Rasayana3 on Agnibala4, Dehabala5 and Sattvabala6 on elderly individuals. 138 patients were registered to the study and divided in to two groups. The drugs were prepared as granules form and administered three times per day and continued for three months. Result of the study revealed that the trial group obtained statistically sig- nificant improvement in the signs and symptoms of Agnibala, Dehabala and Sattvabala on elderly individuals. Keywords: Ageing; Guduchyadi Rasayana; Rasayana Therapy 1. This paper is based on the PhD research work carried out at Institute for Post Graduate Teaching and Research in Ayurveda at Gujarat Ayurved University, Jamnagar, India, 2011. * Senior Lecturer, Department of Kayachikitsa, Institute of Indigenous Medicine, University of Colombo, Rajagiriya, Sri Lanka. e-mail: [email protected] 2. Rejuvenation 3. Name of the trial drug 4. Power of digestion and metabolism 5. Strength of body 6. Strength of the mind 102 Sri Lanka Journal of Advanced Social Studies Vol. 3 - No. 1-January- June -2013 Introduction Ageing is essentially a physiological phenomenon usually defined as the progressive loses of biological functions accompanied by decreasing fertility and increasing mortality with advancing age. It represents structural and functional changes of an organism over its life span. -

Sassafras Tea: Using a Traditional Method of Preparation to Reduce the Carcinogenic Compound Safrole Kate Cummings Clemson University, [email protected]
Clemson University TigerPrints All Theses Theses 5-2012 Sassafras Tea: Using a Traditional Method of Preparation to Reduce the Carcinogenic Compound Safrole Kate Cummings Clemson University, [email protected] Follow this and additional works at: https://tigerprints.clemson.edu/all_theses Part of the Forest Sciences Commons Recommended Citation Cummings, Kate, "Sassafras Tea: Using a Traditional Method of Preparation to Reduce the Carcinogenic Compound Safrole" (2012). All Theses. 1345. https://tigerprints.clemson.edu/all_theses/1345 This Thesis is brought to you for free and open access by the Theses at TigerPrints. It has been accepted for inclusion in All Theses by an authorized administrator of TigerPrints. For more information, please contact [email protected]. SASSAFRAS TEA: USING A TRADITIONAL METHOD OF PREPARATION TO REDUCE THE CARCINOGENIC COMPOUND SAFROLE A Thesis Presented to the Graduate School of Clemson University In Partial Fulfillment of the Requirements for the Degree Master of Science Forest Resources by Kate Cummings May 2012 Accepted by: Patricia Layton, Ph.D., Committee Chair Karen C. Hall, Ph.D Feng Chen, Ph. D. Christina Wells, Ph. D. ABSTRACT The purpose of this research is to quantify the carcinogenic compound safrole in the traditional preparation method of making sassafras tea from the root of Sassafras albidum. The traditional method investigated was typical of preparation by members of the Eastern Band of Cherokee Indians and other Appalachian peoples. Sassafras is a tree common to the eastern coast of the United States, especially in the mountainous regions. Historically and continuing until today, roots of the tree are used to prepare fragrant teas and syrups. -

Method to Estimate Dry-Kiln Schedules and Species Groupings: Tropical and Temperate Hardwoods
United States Department of Agriculture Method to Estimate Forest Service Forest Dry-Kiln Schedules Products Laboratory Research and Species Groupings Paper FPL–RP–548 Tropical and Temperate Hardwoods William T. Simpson Abstract Contents Dry-kiln schedules have been developed for many wood Page species. However, one problem is that many, especially tropical species, have no recommended schedule. Another Introduction................................................................1 problem in drying tropical species is the lack of a way to Estimation of Kiln Schedules.........................................1 group them when it is impractical to fill a kiln with a single Background .............................................................1 species. This report investigates the possibility of estimating kiln schedules and grouping species for drying using basic Related Research...................................................1 specific gravity as the primary variable for prediction and grouping. In this study, kiln schedules were estimated by Current Kiln Schedules ..........................................1 establishing least squares relationships between schedule Method of Schedule Estimation...................................2 parameters and basic specific gravity. These relationships were then applied to estimate schedules for 3,237 species Estimation of Initial Conditions ..............................2 from Africa, Asia and Oceana, and Latin America. Nine drying groups were established, based on intervals of specific Estimation -

Bio-Enhancing Properties of Cow Urine – a Review
ISSN(Online) : 2319-8753 ISSN (Print) : 2347-6710 International Journal of Innovative Research in Science, Engineering and Technology (An ISO 3297: 2007 Certified Organization) Vol. 5, Issue 9, September 2016 Bio-Enhancing Properties of Cow Urine – A Review Farida P. Minocheherhomji Associate Professor, Department of Microbiology, B. P. Baria Science Institute, Navsari, Gujarat, India. ABSTRACT: Antibodies and other chemotherapeutic agents are widely used as conservative treatment in various microbial infections and diseases. Majority of the infections in human beings and animals are caused by bacteria and fungi, especially the spore formers, which are found to create hindrances in treatment. These organisms have the genetic ability to transmit and acquire resistance towards the chemotherapeutic drugs, and in return, the host faces many adverse effects of these drugs. So in order to combat these problems, research is being diverted towards the exploration of naturally available products. Cow as “Kamdhenu” is the fullfiller of all desires. Cow has symbiotic relationship with human beings. In the Veda, cow (Bos indicus) is considered as a most valuable animal and is revered equivalent to a mother. Different products are available from a cow like milk, ghee, curd, dung and urine, generally known as Panchgavya. They are used for many ayurvedic formulations. Out of these five products, Gaumutra has many medicinal properties and is used in the cure of number of diseases like Skin diseases, Kidney related urinary problems, Epilepsy, Anaemia, Constipation, Obesity, Blood pressure regulation and even in fight against cancer. KEYWORDS: Antibodies, Bacteria, Cow Urine, Fungi, Panchgavya. I. INTRODUCTION Nature is an infinite source of discovery of new drugs and its further development. -

Energies Alterations and Chakras' Energies Deficiencies As One of The
RESEARCH ARTICLE Energies Alterations and Chakras’ Energies Deficiencies as one of the Causes of Psoriasis Huang Wei Ling Infectious Diseases, General Practice, Nutrition, Acupuncture, Pain management, Medical Acupuncture and Pain Management Clinic, Franca, São Paulo, Brazil ABSTRACT Introduction: Psoriasis is an inflammatory and proliferative condition of the skin characterized by plaques covered by silvery scales mainly in the exterior surfaces, lumbar region, and scalp. In traditional Chinese medicine, psoriasis is caused by the internal Heat generating a Fire, caused by emotional factors leading to a blocked in the Qi movement. This Fire can enter the Blood circulation or stagnate due to improper diet or due to exogenous Fire. Purpose: the purpose of this study is to demonstrate that patients with psoriasis symptoms have energies alterations and chakras’ energies deficiencies and the balance of this internal energies using Chinese dietary counseling, auricular acupuncture associating with apex ear bloodletting and replenishing the chakras’ energies meridians using homeopathies medications according to the theory Constitutional Homeopathy of the Five Elements Based on Traditional Chinese Medicine are important tools to treat this kind of patients. Methods: Two cases report of patients with history of psoriasis symptoms during years using topical medications and other treatments without any success. They both began treatment using Chinese dietary counseling avoiding dairy products, raw foods, sweets, cold water and also, fried foods, chocolate, honey, coconut, alcoholic beverages, and melted cheese. The radiesthesia procedure was done and reveled that all chakras’ energies were in the lowest level of energy, rated one out of eight and the treatment replenishing the chakras’ energies meridians using homeopathies medications according to the theory created by the author entitled Constitutional Homeopathy of the Five Elements based on Traditional Chinese Medicine. -

Various Terminologies Associated with Areca Nut and Tobacco Chewing: a Review
Journal of Oral and Maxillofacial Pathology Vol. 19 Issue 1 Jan ‑ Apr 2015 69 REVIEW ARTICLE Various terminologies associated with areca nut and tobacco chewing: A review Kalpana A Patidar, Rajkumar Parwani, Sangeeta P Wanjari, Atul P Patidar Department of Oral and Maxillofacial Pathology, Modern Dental College and Research Center, Indore, Madhya Pradesh, India Address for correspondence: ABSTRACT Dr. Kalpana A Patidar, Globally, arecanut and tobacco are among the most common addictions. Department of Oral and Maxillofacial Pathology, Tobacco and arecanut alone or in combination are practiced in different regions Modern Dental College and Research Centre, in various forms. Subsequently, oral mucosal lesions also show marked Airport Road, Gandhi Nagar, Indore ‑ 452 001, Madhya Pradesh, India. variations in their clinical as well as histopathological appearance. However, it E‑mail: [email protected] has been found that there is no uniformity and awareness while reporting these habits. Various terminologies used by investigators like ‘betel chewing’,‘betel Received: 26‑02‑2014 quid chewing’,‘betel nut chewing’,‘betel nut habit’,‘tobacco chewing’and ‘paan Accepted: 28‑03‑2015 chewing’ clearly indicate that there is lack of knowledge and lots of confusion about the exact terminology and content of the habit. If the health promotion initiatives are to be considered, a thorough knowledge of composition and way of practicing the habit is essential. In this article we reviewed composition and various terminologies associated with areca nut and tobacco habits in an effort to clearly delineate various habits. Key words: Areca nut, habit, paan, quid, tobacco INTRODUCTION Tobacco plant, probably cultivated by man about 1,000 years back have now crept into each and every part of world. -

For Review Only
International Wound Journal Essential oils and met al ions as alternative antimicrobial agents: A focus on tea tree oil and silver Journal:For International Review Wound Journal Only Manuscript ID IWJ-15-430.R1 Wiley - Manuscript type: Original Article Keywords: Antimicrobial, Silver, Tea Tree Oil, Wound infection The increasing occurrence of hospital infections and the emerging problems posed by antibiotic resistant strains contribute to escalating treatment costs. Infection on the wound site can potentially stall the healing process at the inflammatory stage, leading to the development of acute wounds. Traditional wound treatment regime can no longer cope with the complications posed by antibiotic resistant strains; hence there is a need to explore the use of alternative antimicrobial agents. In recent research, pre- antibiotic compounds, including heavy metal ions and essential oils have been re-investigated for their potential use as effective antimicrobial Abstract: agents. Essential oils have been identified to have potent antimicrobial, antifungal, antiviral, anti-inflammatory, anti-oxidant and other beneficial therapeutic properties. Similarly, heavy metal ions have also been used as disinfecting agents due to their broad spectrum activities. Such activities is contributed by reactive properties of the metal cations, which allows the ions to interact with many different intracellular compounds, thereby resulting in the disruption of vital cell function leading to cell death. This review will discuss the potential properties of essential oils and heavy metal ions, in particular tea tree oil and silver ions as alternative antimicrobial agents for the treatment of wounds. Page 1 of 52 International Wound Journal Abstract The increasing occurrence of hospital acquired infections and the emerging problems posed by antibiotic resistant microbial strains have both contributed to the escalating cost of treatment. -

Rasayana Herbs of Ayurveda to Treat Age Related Cognitive Decline: an Update
Pharmacogn. J. 2016;8(5):411-423 A multifaceted peer reviewed journal in the field of Pharmacognosy and Natural Products Review Article www.phcogj.com | www.journalonweb.com/pj Rasayana Herbs of Ayurveda to Treat age Related Cognitive Decline: An Update Reena Kulkarni1*, Suhas Kumar Shetty2, Rajarajeshwari N M3, Prasanna Narasimha Rao4 and Nayan J5 1Department of Kaumarabhritya, SDM College of Ayurveda, Tanniruhalla, Hassan-INDIA. 2Department of Manasa Roga, SDM College of Ayurveda, Tanniruhalla, Hassan-INDIA. 3Department of Samhita and Siddhanta, SDM College of Ayurveda, Tanniruhalla, Hassan-INDIA. 4Department of Shalya Tantra, SDM College of Ayurveda, Tanniruhalla, Hassan-INDIA. 5Department of Agada tantra, Sri Kalabairaveshvara Swamy Ayurveda Medical College, RPC layout, Vijayanagar, Bengaluru-40, Karnataka, INDIA. ABSTRACT Introduction: Cognitive decline associated with aging could be minor or protective activity. Acetylcholine esterase inhibition, N-Methyl-D-Aspartate major neuro-cognitive disorder presenting with progressive intellectual antagonism, Dopaminergic activity, Anti-amyloidogenic activity, Inhibition deterioration interfering with day to day activities. Behaviour and personal- of Tau aggregation, neuroprotection and immune modulation are activity ity changes may complicate the life in due course. Significant increase in path ways. Tridosha namely Kapha, Pitta and Vata may be viewed to be global prevalence of people aged above 60 years has raised concerns on categorically predominant in initial, middle and final stage of dementia. Se- effective management of old age problems. Age related cognitive deficits lected herbs thus can be specific based on the pathology and relevant do- and dementia raise to the level of epidemics and established management sha predominance. Conclusion: Rasayana herbs with current updates and is yet underway. -

Astavarga Plants- Threatened Medicinal Herbs of the North-West Himalaya
See discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/312533047 Astavarga plants- threatened medicinal herbs of the North-West Himalaya Article · January 2012 CITATIONS READS 39 714 8 authors, including: Anupam Srivastava Rajesh Kumar Mishra Patanjali Research Institute Patanjali Bhartiya Ayurvigyan evum Anusandhan Sansthan 16 PUBLICATIONS 40 CITATIONS 43 PUBLICATIONS 84 CITATIONS SEE PROFILE SEE PROFILE Rajiv K. Vashistha Dr Ajay Singh Hemwati Nandan Bahuguna Garhwal University Patanjali Bhartiya Ayurvigyan Evam Anusandhan Sansthan Haridwar 34 PUBLICATIONS 216 CITATIONS 5 PUBLICATIONS 79 CITATIONS SEE PROFILE SEE PROFILE Some of the authors of this publication are also working on these related projects: ANTI FUNGAL ACTIVITY OF GANDHAK DRUTI AND GANDHAKADYA MALAHAR View project Invivo study of Roscoea purpurea View project All content following this page was uploaded by Rajesh Kumar Mishra on 10 September 2019. The user has requested enhancement of the downloaded file. Int. J. Med. Arom. Plants, ISSN 2249 – 4340 REVIEW ARTICLE Vol. 2, No. 4, pp. 661-676, December 2012 Astavarga plants – threatened medicinal herbs of the North-West Himalaya Acharya BALKRISHNA, Anupam SRIVASTAVA, Rajesh K. MISHRA, Shambhu P. PATEL, Rajiv K. VASHISTHA*, Ajay SINGH, Vikas JADON, Parul SAXENA Patanjali Ayurveda Research and Development Department, Patanjali Yogpeeth, Maharishi Dayanand Gram, Near Bahadrabad, Haridwar- 249405, Uttarakhand, India Article History: Received 24th September 2012, Revised 20th November 2012, Accepted 21st November 2012. Abstract: Astavarga eight medicinal plants viz., Kakoli (Roscoea purpurea Smith), Kshirkakoli (Lilium polyphyllum D. Don), Jeevak (Crepidium acuminatum (D. Don) Szlach), Rishbhak (Malaxis muscifera (Lindl.) Kuntze), Meda (Polygonatum verticillatum (Linn.) Allioni), Mahameda (P. -

Ayurveda's Immunity Boosting Measures for Self Care During COVID-19 Crisis Among All NSS Functionaries Under Your Jurisdiction
To, All the State NSS Officers, In the region, Punjab, Himachal Pradesh, U.T Chandigarh, Sub:- Ayurveda’s immunity boosting measures for self care during COVID 19 crisis-Reg. Madam/Sir, Kindly find attached herewith the Advisory of Ministry of AYUSH, Government of India received through Directorate of NSS, New Delhi. In this regard It is stated that as you are well aware that in the wake of the Covid 19 outbreak, entire mankind across the globe is suffering. While there is no medicine for COVID-19 as of now, it will be good to take preventive measures which boost our immunity in these times. We all know that prevention is better than cure. So enhancing the body’s natural defence system (immunity) plays an important role in maintaining optimum health. Further It is stated that Ministry of AYUSH recommends the following self-care guidelines for preventive health measures and boosting immunity with special reference to respiratory health. These are supported by Ayurvedic literature and scientific publications. Recommended Measures (I) General Measures 1. Drink warm water throughout the day. 2. Daily practice of Yogasana, Pranayama and meditation for at least 30 minutes as advised by Ministry of AYUSH (#YOGAatHome #StayHome #StaySafe) 3. Spices like Haldi (Turmeric), Jeera (Cumin), Dhaniya (Coriander) and Lahsun (Garlic) are recommended in cooking. (II) Ayurvedic Immunity Promoting Measures 1. Take Chyavanprash 10gm (1tsf) in the morning. Diabetics should take sugar free Chyavanprash. 2. Drink herbal tea / decoction (Kadha) made from Tulsi (Basil), Dalchini (Cinnamon), Kalimirch (Black pepper), Shunthi (Dry Ginger) and Munakka (Raisin) - once or twice a day. -

Riches of the Forest: Food, Spices, Crafts and Resins of Asia
Riches of the forest: Food spices crafts and resins Asia Riches of the forest: Food spices crafts and resins of Asia Editors Citlalli López Patricia Shanley Riches of the forest: Food spices crafts and resins of Asia Riches of the forest: Food spices crafts and resins of Asia Editors Citlalli López Patricia Shanley Scientific reviewer: Jenne de Beer Reviewer and copy editor: Tess Holderness Case study illustrations: Dadi Sungkowo Botanical illustrations: Ishak Syamsudin Layout design: Yani Saloh Layout: Eko Prianto © by Center for International Forestry Research All rights reserved Published in Printed in Desa Putra Indonesia ISBN Office address: Jalan CIFOR Situ Gede Sindang Barang Bogor Barat Indonesia Mailing address: PO Box JKPWB Jakarta Indonesia tel: () fax: () email: cifor@cgiarorg website: wwwciforcgiarorg Acknowledgements We would like to thank the restitution thematic working group especially Alfredo Fantini Rocío Alarcón Gallegos Paul HerschMartínez and Mariana CiavattaPantoja for their catalysing role and dedication to this project Marina Goloubinoff Jenne De Beer Koen Kusters Nicolas Césard Titin Suhartini and Ramadhani Achdiawan offered valuable assistance during the compilation of this volume The CIFORCommunications Unit Information Services Group especially Michael Hailu Yani Saloh and Eko Prianto also offered technical assistance and support This book was developed as part of CIFOR's broader NTFP Case Comparison Project led by Manuel RuizPérez and Brian Belcher who supported this publication throughout its development -
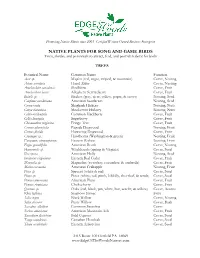
NATIVE PLANTS for SONG and GAME BIRDS Trees, Shrubs, and Perennials to Attract, Feed, and Provide Habitat for Birds
Promoting Native Plants since 2003 Certified Women Owned Business Enterprise NATIVE PLANTS FOR SONG AND GAME BIRDS Trees, shrubs, and perennials to attract, feed, and provide habitat for birds TREES Botanical Name Common Name Function Acer sp. Maples (red, sugar, striped, & mountain) Cover, Nesting Alnus serrulata Hazel Alder Cover, Nesting Amelanchier canadensis Shadblow Cover, Fruit Amelanchier laevis Allegheny Serviceberry Cover, Fruit Betula sp. Birches (grey, river, yellow, paper, & sweet) Nesting, Seed Carpinus caroliniana American hornbeam Nesting, Seed Carya ovata Shagbark Hickory Nesting, Nuts Carya tomentosa Mockernut Hickory Nesting, Nuts Celtis occidentalis Common Hackberry Cover, Fruit Celtis laevigata Sugarberry Cover, Fruit Chionanthus virginicus Fringe Tree Cover, Fruit Cornus alternifolia Pagoda Dogwood Nesting, Fruit Cornus florida Flowering Dogwood Cover, Fruit Crataegus sp. Hawthorns (Washington & green) Nesting, Fruit Euonymus atropurpureus Eastern Wahoo Nesting, Fruit Fagus grandifolia American Beech Cover, Nesting Hamamelis sp. Witchhazels (spring & Virginia) Cover, Seed Ilex opaca American Holly Nesting, Seed Juniperus virginiana Eastern Red Cedar Cover, Fruit Magnolia sp. Magnolias (sweetbay, cucumber, & umbrella) Cover, Fruit Malus coronaria American Crabapple Nesting, Fruit Picea sp. Spruces (white & red) Cover, Seed Pinus sp. Pines (white, red, pitch, loblolly, shortleaf, & scrub) Cover, Seed Prunus americana American Plum Cover, Fruit Prunus virginiana Chokecherry Cover, Fruit Quercus sp. Oaks (red, black, pin, white, bur, scarlet, & willow) Cover, Acorns Rhus typhina Staghorn Sumac Fruit Salix nigra Black Willow Cover, Nesting Salix discolor Pussy Willow Cover, Buds Sassafras albidum Common Sassafras Cover Sorbus americana American Mountain Ash Cover, Fruit Taxodium distichum Bald Cypress Cover, Seed Tsuga canadensis Canadian Hemlock Cover, Seed Thuja occidentalis Eastern Arborvitae Cover, Seed 2415 Route 100 Orefield PA 18069 www.EdgeOfTheWoodsNursery.com SHRUBS & VINES Aronia sp.