Ultrasound-Guided Pain Interventions in Shoulder Region
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Isolated Avulsion Fracture of the Lesser Tuberosity of The
(aspects of trauma) Isolated Avulsion Fracture of the Lesser Tuberosity of the Humerus in an Adult: Case Report and Literature Review Aman Dhawan, MD, Kevin Kirk, DO, Thomas Dowd, MD, and William Doukas, MD solated avulsion fractures of also describe our operative technique, comminuted 3-cm lesser tuberosity the lesser tuberosity of the including use of heavy, nonabsorb- fracture fragment retracted approxi- proximal humerus are rare. able suture. mately 2 cm from the donor site We report the case of a right- (Figures 1B–1D). No biceps tendon Ihand–dominant woman in her early ASE EPORT subluxation or injury and no intra- C R 30s who sustained such an injury, A right-hand–dominant woman in articular pathology were noted. with an intact subscapularis tendon her early 30s presented with right The lesser tuberosity fracture was attached to the lesser tuberosity frag- shoulder pain 1 day after a fall down surgically repaired less than 2 weeks ment. Treatment included surgery to a flight of stairs. During the acci- after injury. Through a deltopectoral restore tension to the subscapularis dent, as her feet slipped out from approach, the rotator interval and muscle and maintain the force couple underneath her and her torso fell the 3×2-cm fracture fragment were about the shoulder joint. One year after injury, the patient reported no pain, excellent range of motion, and “[To be diagnosed] this injury...requires... return to activities. This case demonstrates the diag- careful review of orthogonal radiographs nostic challenge of this injury, which requires a high index of suspicion and and advanced imaging.” careful review of orthogonal radio- graphs and advanced imaging. -

Body Mechanics As the Rotator Cuff Gether in a Cuff-Shape Across the Greater and Lesser Tubercles the on Head of the Humerus
EXPerT CONTENT Body Mechanics by Joseph E. Muscolino | Artwork Giovanni Rimasti | Photography Yanik Chauvin Rotator Cuff Injury www.amtamassage.org/mtj WORKING WITH CLieNTS AFFecTED BY THIS COmmON CONDITION ROTATOR CUFF GROUP as the rotator cuff group because their distal tendons blend and attach to- The four rotator cuff muscles are gether in a cuff-shape across the greater and lesser tubercles on the head of the supraspinatus, infraspinatus, the humerus. Although all four rotator cuff muscles have specific concen- teres minor, and subscapularis (Fig- tric mover actions at the glenohumeral (GH) joint, their primary functional ure 1). These muscles are described importance is to contract isometrically for GH joint stabilization. Because 17 Before practicing any new modality or technique, check with your state’s or province’s massage therapy regulatory authority to ensure that it is within the defined scope of practice for massage therapy. the rotator cuff group has both mover and stabilization roles, it is extremely functionally active and therefore often physically stressed and injured. In fact, after neck and low back conditions, the shoulder is the most com- Supraspinatus monly injured joint of the human body. ROTATOR CUFF PATHOLOGY The three most common types of rotator cuff pathology are tendinitis, tendinosus, and tearing. Excessive physi- cal stress placed on the rotator cuff tendon can cause ir- ritation and inflammation of the tendon, in other words, tendinitis. If the physical stress is chronic, the inflam- matory process often subsides and degeneration of the fascial tendinous tissue occurs; this is referred to as tendinosus. The degeneration of tendinosus results in weakness of the tendon’s structure, and with continued Teres minor physical stress, whether it is overuse microtrauma or a macrotrauma, a rotator cuff tendon tear might occur. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Trapezius Origin: Occipital Bone, Ligamentum Nuchae & Spinous Processes of Thoracic Vertebrae Insertion: Clavicle and Scapul
Origin: occipital bone, ligamentum nuchae & spinous processes of thoracic vertebrae Insertion: clavicle and scapula (acromion Trapezius and scapular spine) Action: elevate, retract, depress, or rotate scapula upward and/or elevate clavicle; extend neck Origin: spinous process of vertebrae C7-T1 Rhomboideus Insertion: vertebral border of scapula Minor Action: adducts & performs downward rotation of scapula Origin: spinous process of superior thoracic vertebrae Rhomboideus Insertion: vertebral border of scapula from Major spine to inferior angle Action: adducts and downward rotation of scapula Origin: transverse precesses of C1-C4 vertebrae Levator Scapulae Insertion: vertebral border of scapula near superior angle Action: elevates scapula Origin: anterior and superior margins of ribs 1-8 or 1-9 Insertion: anterior surface of vertebral Serratus Anterior border of scapula Action: protracts shoulder: rotates scapula so glenoid cavity moves upward rotation Origin: anterior surfaces and superior margins of ribs 3-5 Insertion: coracoid process of scapula Pectoralis Minor Action: depresses & protracts shoulder, rotates scapula (glenoid cavity rotates downward), elevates ribs Origin: supraspinous fossa of scapula Supraspinatus Insertion: greater tuberacle of humerus Action: abduction at the shoulder Origin: infraspinous fossa of scapula Infraspinatus Insertion: greater tubercle of humerus Action: lateral rotation at shoulder Origin: clavicle and scapula (acromion and adjacent scapular spine) Insertion: deltoid tuberosity of humerus Deltoid Action: -

Humerus Weight: Norm Light Lesser Tubercle Ant Surface Bumps: Abs
Collection:______________ ID#:______________ Secondary ID#:______________ 1: _________ 2: _________ : ___ /____/ _____ :_________ Est. Age: Point1: _________ Point2: _________ Est. Sex: M / M? / ? / F? / F Range1: _________ Range2: _________ Cranium L & M & All R parietal depression: abs pres abs pres spheno-occipital synchondrosis: open closed occipital condyle lipping: abs ≥50% ≥75% abs ≥50% ≥75% Vertebral Column Midline Midline C1 lipping: abs ≥50% # scorable lipping: candlewax: C1 eburnation: abs pres C: (10) abs ≥3mm abs pres L1 spinous process: rnd flat ossified L1 sup body surface: NF PF RL FF GF flat porous T: (24) abs ≥5mm abs pres L1 inf body surface: NF PF RL FF GF flat porous L: (10) abs ≥5mm abs pres L5 superior margin: rnd shp lip(any) L5 inferior margin: rnd shp lip(any) DISH: abs ≥4 verts C T L L5 sup body surface: NF PF RL FF GF flat porous L5 inf body surface: NF PF RL FF GF flat porous S1 margin: rnd shp lipped S1-2 fusion: >1cm <1cm closed Sacral elbow: abs pres Sternum & Ribs L & All R & All R1 fusion: abs fused abs fused sternum central dorsal ridge: abs pres R2 rim profile: (2) reg irreg abs cone claw both R3-10 rim profile: (16) reg irreg abs cone claw both R2 shingle rib: (2) norm shingle R3-10 shingle ribs: (16) norm shingle Clavicle & Scapula L R clav med epiphysis fusion: NF PF RL FF NF PF RL FF clav med epiphysis gravel: abs pres abs pres clav med macroporosity: abs ≥3 many abs ≥3 many clav lateral macroporosity: abs ≥3 abs ≥3 scap glen fossa elevated shp & lip: abs <½ ≥½ abs <½ ≥½ Humerus L & All R humerus -

Chapter 5 the Shoulder Joint
The Shoulder Joint • Shoulder joint is attached to axial skeleton via the clavicle at SC joint • Scapula movement usually occurs with movement of humerus Chapter 5 – Humeral flexion & abduction require scapula The Shoulder Joint elevation, rotation upward, & abduction – Humeral adduction & extension results in scapula depression, rotation downward, & adduction Manual of Structural Kinesiology – Scapula abduction occurs with humeral internal R.T. Floyd, EdD, ATC, CSCS rotation & horizontal adduction – Scapula adduction occurs with humeral external rotation & horizontal abduction © McGraw-Hill Higher Education. All rights reserved. 5-1 © McGraw-Hill Higher Education. All rights reserved. 5-2 The Shoulder Joint Bones • Wide range of motion of the shoulder joint in • Scapula, clavicle, & humerus serve as many different planes requires a significant attachments for shoulder joint muscles amount of laxity – Scapular landmarks • Common to have instability problems • supraspinatus fossa – Rotator cuff impingement • infraspinatus fossa – Subluxations & dislocations • subscapular fossa • spine of the scapula • The price of mobility is reduced stability • glenoid cavity • The more mobile a joint is, the less stable it • coracoid process is & the more stable it is, the less mobile • acromion process • inferior angle © McGraw-Hill Higher Education. All rights reserved. 5-3 © McGraw-Hill Higher Education. All rights reserved. From Seeley RR, Stephens TD, Tate P: Anatomy and physiology , ed 7, 5-4 New York, 2006, McGraw-Hill Bones Bones • Scapula, clavicle, & humerus serve as • Key bony landmarks attachments for shoulder joint muscles – Acromion process – Humeral landmarks – Glenoid fossa • Head – Lateral border • Greater tubercle – Inferior angle • Lesser tubercle – Medial border • Intertubercular groove • Deltoid tuberosity – Superior angle – Spine of the scapula © McGraw-Hill Higher Education. -

Muscles of the Upper Limb.Pdf
11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles of the Upper Limb Pectoralis minor ORIGIN: INNERVATION: anterior surface of pectoral nerves ribs 3 – 5 ACTION: INSERTION: protracts / depresses scapula coracoid process (scapula) (Anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Serratus anterior Subclavius ORIGIN: INNERVATION: ORIGIN: INNERVATION: ribs 1 - 8 long thoracic nerve rib 1 ---------------- INSERTION: ACTION: INSERTION: ACTION: medial border of scapula rotates scapula laterally inferior surface of scapula stabilizes / depresses pectoral girdle (Lateral view) (anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Trapezius Levator scapulae ORIGIN: INNERVATION: ORIGIN: INNERVATION: occipital bone / spinous accessory nerve transverse processes of C1 – C4 dorsal scapular nerve processes of C7 – T12 ACTION: INSERTION: ACTION: INSERTION: stabilizes / elevates / retracts / upper medial border of scapula elevates / adducts scapula acromion / spine of scapula; rotates scapula lateral third of clavicle (Posterior view) (Posterior view) 1 11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles Moving Arm Rhomboids Pectoralis major (major / minor) ORIGIN: INNERVATION: ORIGIN: INNERVATION: spinous processes of C7 – T5 dorsal scapular nerve sternum / clavicle / ribs 1 – 6 dorsal scapular nerve INSERTION: ACTION: INSERTION: ACTION: medial border of scapula adducts / rotates scapula intertubucular sulcus / greater tubercle flexes / medially rotates / (humerus) adducts -

Bone Handout”)
The Skeletal System (“Bone Handout”) Bone Markings - as in Table 6.1, know categories, names, descriptions and categories of bone markings Common Fractures - as in Table 6.2, identify type from pictures The Axial Skeleton Skull Cranial bones frontal (supraorbital foramen) parietal temporal (mastoid process, external auditory(acoustic) meatus, styloid process, zygomatic process, stylomastoid foramen) occipital (foramen magnum, hypoglossal canal, occipital condyles) sphenoid (optic canal, superior orbital fissure, sella turcica, foramen rotundum, foramen ovale, foramen spinosum , greater wings, lesser wings) ethmoid (olfactory foramina) Relevant Figures: 7.4, 7.6, 7.7a, 7.9 Facial bones nasal maxilla (infraorbital foramen, inferior orbital fissure) zygomatic mandible (mental foramen, body, ramus, mandibular condyle) lacrimal (lacrimal fossa) palatine inferior nasal conchae vomer Relevant Figures: 7.4, 7.6, 7.7a Sutures coronal sagittal lambdoid squamous Relevant Figures: 7.4, 7.5 Paranasal Sinuses frontal sphenoidal maxillary ethmoidal Relevant Figures: 7.15 Fontanels anterior posterior sphenoidal mastoid Relevant Figures: 7.28 Hyoid bone Relevant Figures: 7.17 1 Vertebrae Parts of a “typical vertebra” using thoracic as example body vertebral arch (pedicle, lamina, vertebral foramen) intervertebral foramen transverse process spinous process superior articular process inferior articular process Divisions of vertebral column cervical (transverse foramina) thoracic (transverse costal facet - for tubercle of rib, superior and inferior costal -

Upper Extremity Scapula
Lab 6 FUNCTIONAL HUMAN ANATOMY LAB #6 UPPER/LOWER EXTREMITY OSTEOLOGY OSTEOLOGY: UPPER EXTREMITY SCAPULA: Borders: Medial (Vertebral) - most superior aspect called the Superior angle Lateral - most inferior aspect called the inferior angle Fossa: Supraspinous fossa Infraspinous fossa Subscapular fossa Glenoid fossa Other Features: acromion process coracoid process scapular spine scapular notch infraglenoid tubercle - located at the bottom of the glenoid fossa supraglenoid tubercle - located at the top of the glenoid fossa Note: the shape of the Glenoid fossa suggests that shoulder stability is heavily reliant on connective tissues surrounding the joint to prevent dislocation CLAVICLE: sternal end - blunt, articulates with the Manubrium acromial end - flat/bladelike, articulates with the Acromium process HUMERUS: head greater tubercle lesser tubercle interturbicular (bicipital) groove - located between the tubercles deltoid tuberosity shaft medial/lateral epicondyles capitulum - the part of the distal condyle that articulates with the Radius trochlea - the part of the distal condyle that articulates with the Ulna olecranon fossa coronoid fossa ULNA: 1 Lab 6 coronoid process olecranon process trochlear notch ulnar tuberosity body head (distal end) radial notch - where the proximal end of the radius articulates interosseous border (lateral side) styloid process RADIUS: body neck head (proximal end) radial tuberosity anterior oblique line interosseous border styloid process CARPAL BONES # of rows? # of bones? Which carpal primarily articulates -

Shoulder Anatomy
ShoulderShoulder AnatomyAnatomy www.fisiokinesiterapia.biz ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy ClavicleClavicle – Sternal end – Acromion end ScapulaScapula Acromion – Surfaces end Sternal Costal end Dorsal – Borders – Angles ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy Scapula 1. spine 2. acromion 3. superior border 4. supraspinous fossa 5. infraspinous fossa 6. medial (vertebral) border 7. lateral (axillary) border 8. inferior angle 9. superior angle 10. glenoid fossa (lateral angle) 11. coracoid process 12. superior scapular notch 13 subscapular fossa 14. supraglenoid tubercle 15. infraglenoid tubercle ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – head – anatomical neck – greater tubercle – lesser tubercle – greater tubercle – lesser tubercle – intertubercular sulcus (AKA bicipital groove) – deltoid tuberosity ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – Surgical Neck – Angle of Inclination 130-150 degrees – Angle of Torsion 30 degrees posteriorly ShoulderShoulder ComplexComplex ArticulationsArticulations SternoclavicularSternoclavicular JointJoint – Sternal end of clavicle with manubrium/ 1st costal cartilage – 3 degree of freedom – Articular Disk – Ligaments Capsule Anterior/Posterior Sternoclavicular Ligament Interclavicular Ligament Costoclavicular Ligament ShoulderShoulder ComplexComplex ArticulationsArticulations AcromioclavicularAcromioclavicular JointJoint – 3 degrees of freedom – Articular Disk – Ligaments Superior/Inferior -

Chapter 6 the Shoulder, Humerus, Elbow and Radius
Chapter 6 The shoulder, humerus, elbow and radius Scapulohumeral (shoulder) joint and humerus RADIOGRAPHIC TECHNIQUE Equipment The scapulohumeral joint may be radiographed with the horse standing if a high-output x-ray machine is available. Better-quality radiographs are generally obtained with the horse under general anaesthesia in lateral recumbency. With the horse anaesthetized, positioning is easier and longer exposure times can be used without risk of movement, so a lower output x- ray machine may be used. The radiation hazard to personnel is also reduced. Digital systems, or rare earth screens and appropriate fi lm, are essential due to the high exposures required to penetrate the large muscle mass in this area. A grid is recommended to reduce the effects of scattered radiation, and lead should be placed behind the cassette to limit back scatter. There is less soft tissue to penetrate cranially; therefore it may be necessary to repeat a view with different exposure factors in order to assess both the cranioproximal aspect of the humerus and the more caudally situated scapu- lohumeral joint properly. Alternatively an aluminium wedge fi lter can be used to modify the exposure. For mediolateral radiographs obtained with the horse standing, the cassette should be mounted in a holder and not hand held. Both mediolateral and oblique views are required for a complete assessment of the scapulohumeral joint, and in selected cases arthrography yields valuable additional information. Positioning Mediolateral view standing The forelimb to be examined is positioned next to the cassette and the limb is protracted as much as the horse will comfortably allow, to avoid super- imposition of the left and right shoulder joints (Figure 6.1). -
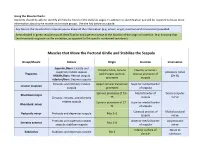
Muscle Charts: Students Should Be Able to Identify All Muscles Listed on the Daily Lab Pages
Using the Muscle Charts: Students should be able to identify all muscles listed on the daily lab pages. In addition to identification you will be required to know more information about some muscle and muscle groups. Use the key below as a guide. Any box on the muscle chart requires you to know all the information (e.g. action, origin, insertion and innervation) provided. Areas shaded in green require muscle identification and a general sense of the location of the origin or insertion. (e.g. knowing that the rhomboids originate on the vertebrae, as opposed to the specific numbered vertebrae). Muscles that Move the Pectoral Girdle and Stabilize the Scapula Group/Muscle Actions Origin Insertion Innervation Superior fibers: Elevate and Occipital bone, cervical Clavicle; acromion superiorly rotate scapula Accessory nerve Trapezius and thoracic spinous process and spine of Middle fibers: Retract scapula (CN XI) processes scapula Inferior fibers: Depress scapula Elevates and inferiorly rotates Upper cervical transverse Superior medial border Levator scapulae scapula processes of scapula Spinous processes of T2– Medial border of Dorsal scapular Rhomboid major Elevates, retracts, and inferiorly T5 scapula nerve rotates scapula Spinous processes of C7– Superior medial border Rhomboid minor T1 of scapula Coracoid process of Medial pectoral Pectoralis minor Protracts and depresses scapula Ribs 3–5 scapula nerve Protracts and superiorly rotates Anterior medial border Long thoracic Serratus anterior Ribs 1–8 scapula; stabilizes scapula of scapula nerve