Developmental Coordination Disorder and Dysgraphia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Developmental Coordination Disorder and Dysgraphia: Signs and Symptoms, Diagnosis, and Rehabilitation
Neuropsychiatric Disease and Treatment Dovepress open access to scientific and medical research Open Access Full Text Article REVIEW Developmental coordination disorder and dysgraphia: signs and symptoms, diagnosis, and rehabilitation This article was published in the following Dove Press journal: Neuropsychiatric Disease and Treatment Maëlle Biotteau 1 Abstract: Developmental coordination disorder (DCD) is a common and well-recognized Jérémy Danna 2 neurodevelopmental disorder affecting approximately 5 in every 100 individuals worldwide. It Éloïse Baudou 3 has long been included in standard national and international classifications of disorders (especially Frédéric Puyjarinet 4 the Diagnostic and Statistical Manual of Mental Disorders). Children and adults with DCD may Jean-Luc Velay 2 come to medical or paramedical attention because of poor motor skills, poor motor coordination, Jean-Michel Albaret 1,5 and/or impaired procedural learning affecting activities of daily living. Studies show DCD persis- tence of 30–70% in adulthood for individuals who were diagnosed with DCD as children, with Yves Chaix 1,3 direct consequences in the academic realm and even beyond. In particular, individuals with DCD 1ToNIC, Toulouse NeuroImaging Center, are at increased risk of impaired handwriting skills. Medium-term and long-term prognosis depends University of Toulouse, Inserm, UPS, Toulouse, France; 2Cognitive on the timing of the diagnosis, (possible) comorbid disorders (and their diagnosis), the variability of Neurosciences Laboratory, CNRS-Aix signs and symptoms (number and intensity), and the nature and frequency of the interventions Marseille University, Marseille, France; individuals receive. We therefore chose to investigate the signs and symptoms, diagnosis, and 3Pediatric Neurology Unit, Children’s Hospital, Purpan University Hospital, rehabilitation of both DCD and developmental dysgraphia, which continues to receive far too little Toulouse, France; 4EuroMov Laboratory, attention in its own right from researchers and clinicians. -

Dyslexia and Dyscalculia Are the Same Thing
Dyscalculia and Dyslexia Two different issues, or part of the same problem? By Tony Attwood C.Ed., B.A., M.Phil. Chairman of The Dyscalculia Group, First and Best in Education Ltd. Dyscalculia is noted as an unexpected difficulty that some people have in dealing with mathematical problems. At its simplest we may note a child whose age and intellect suggests that he or she will be able to undertake a certain range of skills, but who in effect is unable to handle maths problems that we would expect to be well within his or her grasp. As a general introduction to the topic we may note that according to the American Journal of Paediatrics in 2001 dyscalculic children have “Normal or advanced language and other skills, often good visual memory for the printed word, (and) poor mental maths ability often with difficulty in the use of money, such as balancing a chequebook, making change and tipping. Often there is a fear of money and its transactions and difficulty with maths processes (e.g. addition, subtraction, multiplication) and concepts (e.g. sequencing of numbers). There is sometimes poor retention and retrieval of concepts, or an inability to maintain a consistency in grasping maths rules, poor sense of direction, easy disorientation, as well as difficulty with reading maps, telling the time and grappling with mechanical processes, difficulty with abstract concepts of time and direction, schedules, keeping track of time and the sequence of past and future events.” These children make, “Common mistakes in working with numbers including number reversals and omissions,” (and) “May have difficulty learning musical concepts, following directions in sports that demand sequencing or rules, and keeping track of scores and players during games such as cards and board games. -
Dysgraphia: How It Affects a Student’S Performance and What Can Be Done About It
Dysgraphia: How It Affects A Student’s Performance and What Can Be Done About It Alyssa L. Crouch Jennifer J. Jakubecy A Case Study Published in TEACHING Exceptional Children Plus Volume 3, Issue 3, January 2007 Copyright © 2007 by the author. This work is licensed to the public under the Creative Commons Attribution License. Dysgraphia: How It Affects A Student’s Performance and What Can Be Done About It Alyssa L. Crouch Jennifer J. Jakubecy Abstract The purpose of this study was to apply two techniques, drill activities and fine motor ac- tivities, to find whether they help improve the handwriting of a student with dysgraphia. This action research used an ABAB single subject design to find which technique worked better over an eight-week period. The results were inconclusive on which technique worked better. However, the combination of both improved the subject’s handwriting and increased his score by 50%. Therefore, this study suggests that using both techniques can help improve the problems associated with dysgraphia, especially in the area of handwrit- ing. Keywords handwriting, dysgraphia SUGGESTED CITATION: Crouch, A. L., & Jakubecy, J. J. (2007). Dysgraphia: How it affects a student’s performance and what can be done about it. TEACHING Exceptional Children Plus, 3(3) Article 5. Retrieved [date] from http://escholarship.bc.edu/education/tecplus/vol3/iss3/art5 “The ability to write is truly one of the most ing difficulties can be included under the la- important factors in the academic process.” bel of learning disabilities. Another reason is Timothy Dikowski that there is no consensus in the field on one definition or identification process for dys- Introduction graphia. -

The Basics About the 3 D's: Learning Disabilities
THE BASICS ABOUT THE 3 D’S: LEARNING DISABILITIES Cathy Johnson, M.A., C.C.C, S.L.T Licensed Speech/Language Pathologist Structured Literacy Teacher Speech, Language and Learning Center Johnson Academy of Therapeutic Learning Disclosure Neither I nor any member of my immediate family has a financial relationship or interest (currently or within the past 12 months) with any proprietary entity producing health care goods or services consumed by, or used on, patients related to the content of this CME activity. I do not intend to discuss an unapproved/investigative use of a commercial product/device. Agenda ● Three types of learning disabilities: Dyslexia, Dysgraphia, and Dyscalculia ● Definitions ● Signs and symptoms ● Frequently co‐occurring disorders to be aware of: ADHD (30% of those with dyslexia have coexisting AD/HD) &/or APD Learning Disabilities • Problems with age appropriate reading, spelling, and/or writing • A learning disability is not about how smart a person is but more about how they process sounds and language • Most people diagnosed with learning disabilities have average to superior intelligence Definition of Dyslexia ● Dyslexia is no longer diagnosed with regard to an IQ discrepancy. ● We have known this from research that came out in the early 1990s (e.g., Siegel 1992). ● This was officially changed in the DSM‐5 (2013). Definition of Dyslexia- IDA definition average to above average intellectual ability with an unexpected difficulty in reading 1. Dyslexia is a language‐based learning disability. 2. Dyslexia is hereditary and lifelong. 3. Dyslexia is more common than many people think. 4. Before school starts, dyslexia may not be obvious. -

Dysgraphia 101 Laura Dowdy, Stefanie Perry and Kelly Elias
12/2/2016 This is your Brain….. Dysgraphia 101 Laura Dowdy, Stefanie Perry and Kelly Elias This is your Brain Reading and Writing • Orthographic Coding: how the brain pays attention to, visually remembers and codes Orthographic Coding words and word parts relating them to spoken words (thru vs through) • Phonological Coding: segmenting spoken words (word sounds) into units, relate them to how the brain pays attention to, visually units in written words – breaking words apart and putting back together remembers and codes words and word parts • Morphological Coding: coding of base words (“root”) with suffixes and prefixes, for relating them to spoken words (thru vs through) example – corner vs builder • Verbal Working Memory – working memory that allows you to store and process letters and written words, listening comprehension and written sentences • RAN – measures ability to name familiar symbols/single letters, letter groups or words that are repeated across rows both accurately and rapidly • RAS – measures executive function of switching categories (attentional switches) an different 1 12/2/2016 quieter ei telescope sc preapproved er 2 12/2/2016 exclamation ti Phonological Coding Now your turn segmenting spoken words (word sounds) into • Drum roll please……… units, relate them to units in written words – breaking words apart and putting back together Morphological Coding Now Your Turn coding of base words (“root”) with suffixes and Movement Move prefixes, for example – corner vs builder Imaginary Imagine Sentence Sent Reality Real Depth -

Dysgraphia Madeline Brown Southeastern University - Lakeland, [email protected]
Southeastern University FireScholars Classical Conversations Spring 2019 Dysgraphia Madeline Brown Southeastern University - Lakeland, [email protected] Follow this and additional works at: https://firescholars.seu.edu/ccplus Part of the Disability and Equity in Education Commons, Elementary Education Commons, and the Special Education and Teaching Commons Recommended Citation Brown, Madeline, "Dysgraphia" (2019). Classical Conversations. 2. https://firescholars.seu.edu/ccplus/2 This Term Paper is brought to you for free and open access by FireScholars. It has been accepted for inclusion in Classical Conversations by an authorized administrator of FireScholars. For more information, please contact [email protected]. Brown !1 Madeline Brown Professor Veach CC ENG 1233 22 MAR 2019 Dysgraphia Introduction Envision a kindergarten student sitting in school with an assignment to copy. As she sits down, she already knows the challenge writing presents for her but does not speak up or say anything because this time probably will not be any different than when she requested help before. She has been labeled as a lazy writer and has never had the most readable handwriting. All of the other children around her finish the assignment and she inevitably she remains unable to complete the first sentence. This scene does not have to play out this way. Students in schools across the world are created uniquely with different strengths and weaknesses. Teacher to student ratio, few learning disability training resources, and confusion regarding whether a child has a legitimate learning challenge all contribute to the inability of schools to accurately detect early learning disabilities (Judd 97). Without proper training, some difficult to identify diagnoses of childhood learning and behavioral struggles include but are not limited to; Dyslexia, Autism, Dyspraxia, Attention Deficit Disorder, Dyscalculia, and Dysgraphia. -

What This Means for You As a Special Educator/Service Provider
Anne Arundel County – Department of Special Education Technical Assistant Bulletin (revised July 2017) Specific Learning Disability; Including Dyslexia; Dysgraphia; Dyscalculia September 2019 Overall Emphasis and Purpose: Specific Learning Disability (SLD) is one of the 13 categories of disability recognized by the IDEA. SLD is the only disability category for which the IDEA establishes special evaluation procedures, in addition to the general procedures that are used for all students with disabilities. The definition of a SLD is “a disorder in one or more of the basic psychological processes involved in understanding, or in using language spoken or written, that may manifest itself in the imperfect ability to listen, think, speak, read, write, spell, or do mathematical calculations.” During the 2017 legislative session, a bill was passed authorizing schools to identify dyslexia, dysgraphia, or dyscalculia, as subcategories under the overarching SLD classification. What this means for you as a Special What the Special Educator/Service Educator/Service Provider: Provider needs to do if not already doing: • The identification of a SLD requires that the student • Ensure that school staff are supported in implementing exhibit a pattern of strengths and weaknesses in research and/or evidence-based intervention for any performance, achievement, or both, relative to age, student who is struggling. Progress monitoring is a key State approved grade level standards, or intellectual component of determining the effectiveness of the development, as a result of a comprehensive intervention prior to considering the possibility of a evaluation. disability under the IDEA. • A student identified with a specific learning disability, • The IEP team must consider exclusionary factors, such with or without dyslexia, dysgraphia, or dyscalculia, as a lack of appropriate education, intellectual must also exhibit educational impact and require disability, visual, hearing, or motor impairment, specialized instruction. -
Dyslexia Or Ld in Reading: What Is the Difference?
DYSLEXIA OR LD IN READING: WHAT IS THE DIFFERENCE? Anise Flowers & Donna Black, Pearson Dyslexia or LD in Reading? TCASE 2017 Image by Photographer’s Name (Credit in black type) or Image by Photographer’s Name (Credit in white type) International Dyslexia Association Dyslexia is a specific learning disability that is neurological in origin. It is characterized by Dyslexia or LD in Reading: What difficulties with accurate and/or fluent word is the Difference? recognition and by poor spelling and decoding abilities. These difficulties typically result from a deficit in the phonological component of language that is often unexpected in relation to other cognitive abilities and the provision of Presented by effective classroom instruction. Secondary Anise Flowers, Ph.D. Donna Black, LSSP consequences may include problems in reading comprehension and reduced reading experience TCASE that can impede growth of vocabulary and January 2017 background knowledge. Presentation Title Arial Bold 7 pt 1 2 Dyslexia Identification and Services in Texas Dyslexia Definition (in Texas) Texas Education Code (TEC)§38.003 defines Texas Education Code (TEC)§38.003 definition: dyslexia and mandates testing and the provision of 1. “Dyslexia” means a disorder of constitutional instruction origin manifested by a difficulty in learning to State Board of Education (SBOE) adopts rules and read, write, or spell, despite conventional standards for administering testing and instruction instruction, adequate intelligence, and TEC §7.028(b) relegates responsibility for school sociocultural opportunity. compliance to the local school board 2. “Related disorders” include disorders similar to or 19 (TAC)§74.28 outlines responsibilities of districts related to dyslexia such as developmental auditory and charter schools in the delivery of services to imperceptions, dysphasia, specific developmental students with dyslexia dyslexia, developmental dysgraphia, and The Rehabilitation Act of 1973, §504, establishes developmental spelling disability. -

Dyslexia & Dysgraphia
Dyslexia & Dysgraphia Cena Holifield, Ph.D., CALT, QI The 3-D School, Executive Director William Carey University, Assistant Professor Oral Communication is a Natural Process Reading and Writing are not Natural Processes The lecture today will answer these questions…. • What is Dyslexia? • What is Dysgraphia? • How can these disorders be addressed? Specific Learning Disorders • Dyslexia Dysgraphia Reading Written Expression Specific Learning Disorder • a disorder in one or more of the basic psychological processes involved in understanding or in using language, spoken or written, which may manifest itself in an imperfect ability to listen, think, speak, read, write, spell or to do mathematical calculations. IDEA, 2004 Dyslexia is a specific learning disability that is neurological in origin. Students have difficulties with accurate and/or fluent word recognition and by poor spelling and decoding abilities. These difficulties typically result from a deficit in the phonological component of language. Difficulties are often unexpected in relation to cognitive ability and the provision of traditional classroom instruction. Secondary consequences may include problems in reading comprehension and reduced reading experience that can impede growth of vocabulary and background knowledge. Dysgraphia • Dysgraphia is a specific learning disability that is a neurological condition causing trouble with written expression. Students struggle with holding a pencil, organizing letters on a line, therefore, handwriting tends to be messy. Many struggle with -

Developmental Dyscalculia, Gender, and the Brain
510 ArchivesofDiseasein Childhood 1993; 68: 510-512 CURRENT TOPIC Arch Dis Child: first published as 10.1136/adc.68.4.510 on 1 April 1993. Downloaded from Developmental dyscalculia, gender, and the brain Varda Gross-Tsur, Orly Manor, Ruth S Shalev Background Aldenkamp reported that children in the 12-18 Developmental dyscalculia is a primary cognitive year age group had the most difficulties with disorder of childhood affecting the ability of an mathematics. 14 Seidenberg et al studied the otherwise intelligent and healthy child to learn academic achievement of 122 children ages 7-15 arithmetic.' Preliminary evidence indicates that years and found that this group was making less developmental dyscalculia is seen in 5-6% of academic progress than expected for their age normal children23 and is as prevalent as develop- and level of intelligence quotient (IQ); academic mental dyslexia or the attention deficit hyper- deficiencies were greatest in the area of arith- activity disorder.' One of the classifications of metic followed by spelling, reading comprehen- developmental dyscalculia subdivides dys- sion, and word recognition skills.'5 It has been calculia to: (1) alexia and agraphia for numbers, postulated that the 'speed factor type' oflearning (2) spatial dyscalculia, (3) anarithmetia (impair- disability in epileptic children was found to be ment of calculation per se), (4) attentional- related to underachievement in arithmetic.8 sequential dyscalculia, and (5) mixed type.4 Early age of seizure onset, age of the child, Rourke and Finlayson -
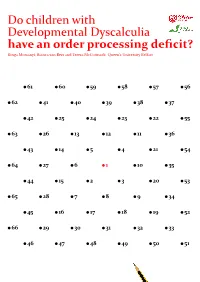
Do Children with Developmental Dyscalculia Havean Orderprocessing Deficit?
Do children with Developmental Dyscalculia have an order processing deficit? Kinga Morsanyi, Bianca van Bers and Teresa McCormack, Queen’s University Belfast 61 60 59 58 57 56 62 41 40 39 38 37 42 25 24 23 22 55 63 26 13 12 11 36 43 14 5 4 21 54 64 27 6 1 10 35 44 15 2 3 20 53 65 28 7 8 9 34 45 16 17 18 19 52 66 29 30 31 32 33 46 47 48 49 50 51 Contents Research highlights 2 Executive summary 5 The need for this research 7 Summary of aims 8 Methods 9 Key findings 14 Summary of key findings and recommendations 17 References 21 Acknowledgements 23 Appendix: Infographics 24 1 Research highlights Study 1: The prevalence of specific learning disorder in mathematics (SLDM or dyscalculia)1 This was the first prevalence study of SLDM since the publication of the new DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) diagnostic criteria in 2013. We considered data from 2,421 children (their level of intelligence and educational achievement in mathematics and English were recorded over several school years). We investigated the effects of gender, socio-economic status, special educational needs (other than issues related to mathematics), and whether the child spoke English as their first language on mathematics achievement. 5.7% of the sample was identified as having SLDM. Compared to earlier (DSM-IV) diagnostic criteria, the prevalence of SLDM was almost 6 times higher. A child was more than a 100 times more likely to receive a diagnosis of dyslexia than SLDM, although prevalence rates are expected to be similar. -

WORKING MEMORY & LEARNING DISABILITIES Working Memory Is
3/26/14 Working Memory is the FOUNDATION of Learning WORKING MEMORY & LEARNING DISABILITIES Tracy Packiam Alloway, PhD WM & Learning DisabiliKes DYSLEXIA (READING) • WHAT is the Core Deficit? • WHY is Working Memory is involved? • HOW to support Working Memory? 1 3/26/14 DYSLEXIA (READING) DYSLEXIA (READING) GENERAL STRATEGIES GENERAL STRATEGIES • Reduce working memory processing in • Keep track of their place in complex activities acKviKes – History Kmelines Rulers: reading & math problems – 45 + 98 45 +98 DYSLEXIA (READING) MATH (DYSCALCULIA) SPECIFIC STRATEGIES • Shorten acKviKes to reduce WM load – Sam worked with only 5 flowers – Repeated instructions just for him www.tracyalloway.com 2 3/26/14 Math (Dyscalculia) Math (Dyscalculia) GENERAL STRATEGIES GENERAL STRATEGIES • Use visual representaon to support working memory • Use visual representaon to support working memory • Algebra: negative exponents • Algebra: negative exponents www.tracyalloway.com Math (Dyscalculia) DCD (Motor) • Gross motor skills (large movements): SPECIFIC STRATEGIES – Poor balance: Riding a bicycle • Model the use of memory aids – Poor hand-eye co-ordination: Catching a ball & batting – Number lines • Fine motor skills (small movements): – Lack of manual dexterity: using cutlery, craft work, 1, 2, __, 4, __ playing musical instruments – Poor manipulative skills: Typing, handwriting and drawing, fastening clothes & tying shoelaces www.tracyalloway.com Alloway (2006) Working Memory & Neurodevelopmental Disorders. Psy Press 3 3/26/14 DCD (MOTOR) DCD (Motor) • Motor skills or Working Memory = Learning difficulties? • Two groups: – High Visual-Spatial Memory – Low Visual-Spatial Memory • Motor skills: Both groups will have low learning scores • Working Memory: Low VS Memory group will have lower learning scores • Low Visual-Spatial Memory group performed worse in Reading & Math – Even after accounting for IQ Alloway (2007) J.