Lethbridge Substance Use Discussion Paper
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Northwest Territories Territoires Du Nord-Ouest British Columbia
122° 121° 120° 119° 118° 117° 116° 115° 114° 113° 112° 111° 110° 109° n a Northwest Territories i d i Cr r eighton L. T e 126 erritoires du Nord-Oues Th t M urston L. h t n r a i u d o i Bea F tty L. r Hi l l s e on n 60° M 12 6 a r Bistcho Lake e i 12 h Thabach 4 d a Tsu Tue 196G t m a i 126 x r K'I Tue 196D i C Nare 196A e S )*+,-35 125 Charles M s Andre 123 e w Lake 225 e k Jack h Li Deze 196C f k is a Lake h Point 214 t 125 L a f r i L d e s v F Thebathi 196 n i 1 e B 24 l istcho R a l r 2 y e a a Tthe Jere Gh L Lake 2 2 aili 196B h 13 H . 124 1 C Tsu K'Adhe L s t Snake L. t Tue 196F o St.Agnes L. P 1 121 2 Tultue Lake Hokedhe Tue 196E 3 Conibear L. Collin Cornwall L 0 ll Lake 223 2 Lake 224 a 122 1 w n r o C 119 Robertson L. Colin Lake 121 59° 120 30th Mountains r Bas Caribou e e L 118 v ine i 120 R e v Burstall L. a 119 l Mer S 117 ryweather L. 119 Wood A 118 Buffalo Na Wylie L. m tional b e 116 Up P 118 r per Hay R ark of R iver 212 Canada iv e r Meander 117 5 River Amber Rive 1 Peace r 211 1 Point 222 117 M Wentzel L. -

Grassy Mountain Coal Project Project Description Summary
Benga Mining Limited operating as Riversdale Resources Grassy Mountain Coal Project Project Description Summary Prepared for: Prepared by Canadian Environmental Assessment Agency Millennium EMS Solutions Ltd. 22nd Floor, Place Bell Suite 325, 1925 – 18th Avenue NE 160 Elgin Street Calgary, AB T2E 7T8 Ottawa, ON K1A 0H3 On Behalf of: Riversdale Resources Limited Benga Mining Limited 12331 – 20th Avenue PO Box 660 Blairmore, AB T0K 0E0 March, 2015 File #14‐00201‐01 Riversdale Resources Limited Grassy Mountain Coal Project March 2015 Benga Mining Limited operating as Riversdale Resources 1.0 GENERAL INFORMATION AND CONTACTS 1.1 Project Overview Benga Mining Limited (Benga), a wholly owned subsidiary of Riversdale Resources Limited (Riversdale), is proposing to develop the Grassy Mountain Coal Project (the Project). The Project is located in south‐west Alberta near the Crowsnest Pass, approximately 7 km north of the community of Blairmore (Figure 1). The Project involves a surface coal mine, a coal preparation plant, and associated infrastructure including a coal conveyor system, a rail load‐out facility, an access corridor, maintenance shops, and other pertinent facilities (Figure 1). This Project Description has been prepared by Riversdale and is being submitted to the Canadian Environmental Assessment Agency (CEAA) as the designated Project is described in the Regulations Designating Physical Activities (CEAA SOR/2012‐147). The following document provides the pertinent project information as set out in the Prescribed Information for the Description of a Designated Project Regulations (CEAA SOR/2012‐148), and follows the Guide to Preparing a Description of a Designated Project Under the Canadian Environmental Assessment Act, 2012 (CEAA 2014). -

Alberta, 2021 Province of Canada
Quickworld Entity Report Alberta, 2021 Province of Canada Quickworld Factoid Name : Alberta Status : Province of Canada Active : 1 Sept. 1905 - Present Capital : Edmonton Country : Canada Official Languages : English Population : 3,645,257 - Permanent Population (Canada Official Census - 2011) Land Area : 646,500 sq km - 249,800 sq mi Density : 5.6/sq km - 14.6/sq mi Names Name : Alberta ISO 3166-2 : CA-AB FIPS Code : CA01 Administrative Subdivisions Census Divisions (19) Division No. 11 Division No. 12 Division No. 13 Division No. 14 Division No. 15 Division No. 16 Division No. 17 Division No. 18 Division No. 19 Division No. 1 Division No. 2 Division No. 3 Division No. 4 Division No. 5 Division No. 6 Division No. 7 Division No. 8 Division No. 9 Division No. 10 Towns (110) Athabasca Banff Barrhead Bashaw Bassano Beaumont Beaverlodge Bentley Black Diamond Blackfalds Bon Accord Bonnyville Bow Island Bowden Brooks Bruderheim Calmar Canmore Cardston Carstairs Castor Chestermere Claresholm Coaldale Coalhurst Cochrane Coronation Crossfield Crowsnest Pass Daysland Devon Didsbury Drayton Valley Drumheller Eckville Edson Elk Point Fairview Falher © 2019 Quickworld Inc. Page 1 of 3 Quickworld Inc assumes no responsibility or liability for any errors or omissions in the content of this document. The information contained in this document is provided on an "as is" basis with no guarantees of completeness, accuracy, usefulness or timeliness. Quickworld Entity Report Alberta, 2021 Province of Canada Fort MacLeod Fox Creek Gibbons Grande Cache Granum Grimshaw Hanna Hardisty High Level High Prairie High River Hinton Innisfail Killam Lac la Biche Lacombe Lamont Legal Magrath Manning Mayerthorpe McLennan Milk River Millet Morinville Mundare Nanton Okotoks Olds Oyen Peace River Penhold Picture Butte Pincher Creek Ponoka Provost Rainbow Lake Raymond Redcliff Redwater Rimbey Rocky Mountain House Sedgewick Sexsmith Slave Lake Smoky Lake Spirit River St. -

Targeted Residential Fire Risk Reduction a Summary of At-Risk Aboriginal Areas in Canada
Targeted Residential Fire Risk Reduction A Summary of At-Risk Aboriginal Areas in Canada Len Garis, Sarah Hughan, Paul Maxim, and Alex Tyakoff October 2016 Executive Summary Despite the steady reduction in rates of fire that have been witnessed in Canada in recent years, ongoing research has demonstrated that there continue to be striking inequalities in the way in which fire risk is distributed through society. It is well-established that residential dwelling fires are not distributed evenly through society, but that certain sectors in Canada experience disproportionate numbers of incidents. Oftentimes, it is the most vulnerable segments of society who face the greatest risk of fire and can least afford the personal and property damage it incurs. Fire risks are accentuated when property owners or occupiers fail to install and maintain fire and life safety devices such smoke alarms and carbon monoxide detectors in their homes. These life saving devices are proven to be highly effective, inexpensive to obtain and, in most cases, Canadian fire services will install them for free. A key component of driving down residential fire rates in Canadian cities, towns, hamlets and villages is the identification of communities where fire risk is greatest. Using the internationally recognized Home Safe methodology described in this study, the following Aboriginal and Non- Aboriginal communities in provinces and territories across Canada are determined to be at heightened risk of residential fire. These communities would benefit from a targeted smoke alarm give-away program and public education campaign to reduce the risk of residential fires and ensure the safety and well-being of all Canadian citizens. -
IOGC 2004-05 Annual Report
INDIAN OIL AND GAS CANADA 2004/2005 ANNUAL REPORT Published under the authority of the Minister of Indian Affairs and Northern Development Ottawa, 2005 www.ainc-inac.gc.ca 1-800-567-9604 TTY only 1-866-553-0554 QS-9003-010-EE-A1 Catalogue: R1-5/2005E ISBN: 0-662-42347-X © Minister of Public Works and Government Services Canada Cette publication peut aussi tre obtenue en français sous le titre : Pétrole et gas des Indiens du Canada Rapport annuel 2004-2005 TABLE OF CONTENTS OVERVIEW OF IOGC 4 IOGC Co-Management 12 Streamlining the 22 Production Board Royalty Process 1 Message from CEO 26 Planning and 2 Corporate Evolution 7 Indian Resource 13 Automation of Interest Corporate Services Council with Accounts Receivable 28 Wells Drilled 2 Statutory Authorities System KEY INITIATIVES Summary 3 Mandate 9 First Nations Oil OPERATIONS 32 Financial 3 Mission and Gas Initiative 16 Executive Operations 3 IOGC Organization Chart 12 Royalty with Certainty 18 Land IOGC 2004/2005 MESSAGE FROM THE CEO On behalf of everyone at Indian Oil and Gas Canada (IOGC), I am pleased to present the IOGC Annual Report 2004-2005.The report not only documents our evolving activities and highlights our accomplishments, but also illustrates some of the progress First Nations are making in the oil and gas industry. Having started as IOGC’s new Chief Executive Officer established over the past decade. During this time, the Blood, and Executive Director in January 2005, I hope to bring Siksika and White Bear First Nations have worked closely new energy and a fresh view into the position and into the with Indian Oil and Gas Canada to develop the capacity to organization while climbing the steep learning curve that assume control and management of their oil and gas resources. -
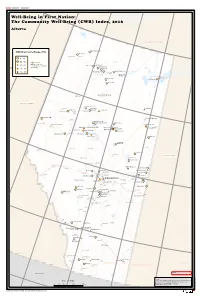
The Community Well-Being (CWB) Index, 2016
126° W 123° W 120° W 117° W 114° W 111° W Well-Being in First Nation: The Community Well-Being (CWB) Index, 2016 Alberta Bistcho Lake NORTHWEST TERRITORIES U¸ pper Hay River 212 CWB Index Score Range, 2016 H¸ ay Lake 209 ! Rainbow Lake Assumption ¸ ! N ° 0 0 - 49 6 ¸ Margaret 50 - 59 Higher scores Lake indicate a greater ·! 60 - 69 High Level !P B¸ ushe River 207 N level of socio-economic ° ¸ 7 Child Lake 164A 5 well-being. ¸ ^^ 70 - 79 Boyer 164 ¸ ¸ r John d'Or Prairie 215 Rive ! Peac e ^^ 80 - 100 Fort Vermilion 173B John D'Or !P !P Prairie ¸ La Crête !P Fox Lake Fox Lake 162 Fort Chipewyan ¸ Allison Bay 219 Tall Cree 173A ·! Dog Head 218 ·!!P Lake Athabasca ¸ Lake Tall Cree 173 Claire Richardson Lake r e v i R a c s a b a P h ! t Manning ALBERTA A BRITISH COLUMBIA Woo¸ dland Cree 226 ¸ Fort Mackay Fairview Woodland Grimshaw ¸ !P ¸ Cree 228 ^ !P P Loon Lake 235 ^ ! Little Buffalo Duncan's 151A Peace ·! River H¸ orse Lakes 152B Fort McMurray Falher " !P U¸ tikoomak Lake 155 P ¸ N ! ¸ Utikoomak Lake 155A Wabasca 166C ° 7 Beaverlodge 5 Gregoire Lake 176A Grande Prairie Utikuma North Wabasca " Lake Gordon " Lake ¸ ·! Lake Kapawe'no First Nation (Freeman 150B) Des¸ marais ·! Wabasca 166B ¸ Gregoire Lake 176 ! Wabasca 166A · ^ ¸ High Prairie !P Wabasca 166D ^ ·! Sucker Creek 150A Wabasca 166 ¸ ¸ Valleyview Sturgeon Lake 154 !P Lesser Slave Lake Drift Pile River 150 ! N · ° 4 ¸ 5 Swan River 150E Janvier 194 !P Slave Lake ¸ Jean Baptiste Gambler 183 Calling Lake Winefred Lake Fox Creek !PSwan Hills Grande Cache !P !P H¸ eart Lake 167 Athabasca Lac La !P Biche SASKATCHEWAN Whitecourt Lac La Biche !P !P B¸ eaver Lake 131 Barrhead Mayerthorpe !P !P Cold Hinton Lake !P ¸ !P White Fish Lake 128 ¸ Cold Lake 149B Edson Chip Lake ¸ Alexander 134 !P Alexis 133 Lac Grand Centre " Smoky Lake ¸ Ste. -
Environmental Effects
CEAA Project Description Summary Sundance 7 Project GENERAL INFORMATION 1. The project’s name, nature and proposed location. TransAlta MidAmerican Partnership (TAMA Power) is pleased to provide this Project Summary for the proposed Sundance 7 Project (the Project). TAMA Power is a partnership between TransAlta Corporation (TransAlta) and MidAmerican Energy Holdings Company. The Project would be located near the existing TransAlta coal-fired power generation facilities in central Alberta, and is planned to be a combined-cycle natural gas-fired power generation plant in a 2 x 1 configuration with a gross nominal generation capacity of 856 megawatts (MW). The Project will be located in a green field site in northwest and southwest quarter-sections of 10-52-4 West of the Fifth Meridian (W5M), approximately 7 kilometres (km) southwest of the Village of Wabamun, Alberta (Figure 1). It is anticipated the Project will be in service in late 2018, in anticipation of the programed retirement of coal-fired assets in the region. The Project will be a highly efficient combined cycle natural gas power plant and TAMA Power has incorporated low emission technology into the design to limit potential adverse environmental effects. The Project site was selected in order to take advantage of an existing power facility labor pool and infrastructure, thus reducing the footprint of new disturbance. 2. The proponent’s name and contact information and the name and contact information of their primary representative for the purpose of the description of the project. Name of the proponent: TransAlta MidAmerican Partnership Address of the proponent: TransAlta MidAmerican Partnership 110 - 12 Avenue SW Calgary, AB T2P 2M1 Principal contact person: Lois Miller Environmental Specialist TransAlta Corporation Telephone: 780-731-6000 Ext 6849 Facsimile: 780-731-6075 Email: [email protected] 1 June 2014 LEGEND 764 COUNTY OF BARRHEAD NO. -

First Nations and Indian Reserves Fire Losses, Alberta: 2000 - 2009 SOURCE: Office of the Fire Commissioner
First Nations and Indian Reserves Fire Losses, Alberta: 2000 - 2009 SOURCE: Office of the Fire Commissioner First Nations Reserve Fires Fire Deaths Fire Injuries $ Losses Siksika Nation 61 0 6 2,869,377 Blood Tribe 4 1 0 251,000 Cold Lake First Nations 7 0 1 279,633 Driftpile River Band 2 1 1 316,000 Enoch Cree Nation 16 1 0 1,355,988 Ermineskin Band 12 0 3 444,000 Athabasca Chipewyan First Nation 1 0 0 66,000 Fort McKay First Nation 1 0 0 135,000 Fort McMurray First Nation 1 0 0 59,980 Frog Lake First Nation 28 1 0 2,980,312 Jean Baptiste Gambler #183 1 1 0 30,000 Horse Lake Band 2 0 0 150,000 Chipewyan Prairie First Nation 2 0 0 135,000 Kehewin Cree Nation 6 0 0 714,824 Little Red River Cree Nation 2 0 0 76,000 Louis Bull Tribe 18 0 1 1,578,043 Montana Band 4 0 0 179,000 Onion Lake Band 1 0 0 71,245 Paul First Nation 6 0 0 2,350,000 Piikani Nation 5 0 0 189,570 Saddle Lake First Nation 6 0 0 216,651 Samson Cree Nation 43 0 1 3,583,203 First Nations Reserve Fires Fire Deaths Fire Injuries $ Losses Tsuu Tina Nation 27 0 1 691,373 Sturgeon Lake Band 6 0 0 237,821 Sucker Creek Band 2 0 0 327,000 Tallcree First Nation 1 0 0 40,000 Whitefish Lake First Nation 6 0 0 532,000 Alexander First Nation 7 0 1 31,705 Alexis First Nation #133 3 0 0 230,000 Beaver Lake Cree Nation 1 0 0 100,000 Bigstone Cree Nation 10 1 0 265,070 Saddle Lake #125 67 2 7 2,935,795 Whitefish Lake #128 33 0 0 1,941,042 Dene Tha First Nation 6 0 0 671,922 Loon River Cree Nation 1 0 0 40,760 Woodland Cree Band 3 2 0 145,000 Stoney (Chiniki) Band 1 0 0 40,000 Stoney (Wesley) -

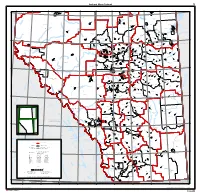
Sec H Aboriginal Consultation and Assessment
Section H Aboriginal Groups Consultation and Assessment Benga Mining Limited Grassy Mountain Coal Project Section H: Aboriginal Groups Consulation and Assessment Table of Contents Page H. ABORIGINAL GROUPS CONSULTATION AND ASSESSMENT ........................................ H-1 H.1 INTRODUCTION ........................................................................................................................... H-1 H.1.1 Aboriginal Consultation ........................................................................................................ H-2 H.2 ASSESSMENT METHODS ............................................................................................................ H-8 H.2.1 Project Setting and Background Information ..................................................................... H-9 H.2.2 Potential Effects on Aboriginal Valued Components ....................................................... H-9 H.2.3 Mitigation Measures ............................................................................................................ H-11 H.2.4 Characterization of Residual Effects .................................................................................. H-11 H.2.5 Cumulative Effects Assessment ......................................................................................... H-13 H.2.6 Follow-up and Monitoring Programs ............................................................................... H-13 H.2.7 Aboriginal Issues and Concerns ....................................................................................... -
South Part Alberta Partie Sud 16
South part Alberta Partie sud 16 120°W 119°W 118°W 117°W 116°W 115°W 114°W 113°W 112°W 111°W 110°W / Sturgeon Lake 154A, IRI 55°N Valleyview, T Heart Lake 167, IRI / 55°N Grande Prairie County No. 1, MD 18 818 / 18 018 12 840 19 006 Opportunity No. 17, MD 17 031 Sturgeon Lake 154, IRI 19 18 816 Lesser Slave River No.124, MD a c 17 033 s a b a h 17 t Big Lakes, MD A L 17 027 e a r Island Lake, SV c è la i 13 049 B v i Lac la Biche County, MD / che i Island Lake South, SV 12 037 R / / 13 051 r e West Athabasca County, MD v Whispering Hills, SV i Baptiste, SV 13 044 R 13 061 Swan Hills, T 13 057 / / 17 024 a c / s a b / a / / h / t Sunset Beach, SV Greenview No. 16, MD South Athabasca, T 18 015 A 13 047 Beaver Lake 131, IRI Baptiste, SV 13 048 Bondiss, SV Cold Lake 149B, IRI Boyle, VL 13 053 12 828 ld 13 055 / 13 046 12 815 Co / / ke / La Mewatha Beach, SV 13 045 Bonnyville No. 87, MD Cold Lake, CY / 12 004 12 002 18 Cold Lake / 149A, IRI Fox Creek, T 12 12 813 18 002 845 / / Larkspur, SV Cold Lake 13 033 Pelican Narrows, SV Bonnyville, T 149, IRI 12 013 12 009 / Glendon, VL 12 810 Woodlands County, MD Westlock County, MD / 12 012/ / 13 029 13 028 White Fish Lake 128, IRI 13 12 808 Smoky Lake County, MD / Thorhild County No. -

Cultural World Heritage and Indigenous Empowerment
G ENEVIÈVE S USEMIHL Cultural World Heritage and Indigenous Empowerment The Sites of SGang Gwaay and Head-Smashed-In Buffalo Jump1 ____________________ Zusammenfassung In SGang Gwaay an der Westküste des Inselarchipels Haida Gwaii zeugen Überreste von Langhäusern und Totempfählen von der traditionellen Lebensweise und Kultur der Haida. Head-Smashed-In Buffalo Jump (HSIBJ) im südlichen Alberta ist einer der ältesten, größten und am besten erhaltenen buffalo jumps in Nordamerika und ein einzigartiges Beispiel für die traditionelle Jagd- und Lebensweise der Prärieindianer. Beide Orte – von herausragender Bedeutung für die Haida und Blackfoot – wurden 1981 in die Liste der UNESCO Weltkulturerbestätten aufgenommen. Für die indigene Bevölkerung ist ihr kulturelles Erbe essentiell für die Wiederbelebung und Weiterfüh- rung ihrer kulturellen Eigenständigkeit. Die vorliegende Fallstudie vergleicht die ge- meinschaftlich-kooperativ verwaltete Kulturerbestätte SGang Gwaay mit dem von der Regierung Albertas verwalteten HSIBJ, untersucht die Bedeutung von Weltkulturerbe- stätten für die Stärkung, Sensibilisierung und Kompetenzerweiterung der Indianer Nordamerikas und zeigt, welchen signifikanten Einfluss Faktoren wie Eigentumsver- hältnisse und Administration, Beteiligung der indigenen Gemeinschaft im Manage- ment und die Erwartungen der Besucher auf die sozio-politische, kulturelle und spiri- tuelle Förderung und Entwicklung der indigenen Gruppen sowie auf die Narrative der Stätten haben. Abstract At the village of SGang Gwaay, located at the west coast of Haida Gwaii, the re- mains of large cedar long houses, together with a number of carved mortuary and memorial poles, illustrate the art and way of life of Haida society, bearing unique testimony to the culture of the Haida. Head-Smashed-In Buffalo Jump, located in the Porcupine Hills of Southern Alberta, is one of the oldest, largest and best preserved buffalo jumps in North America and an outstanding illustration of the subsistence hunting techniques of Plains nations. -
Diabetes by Community
Age-Adjusted Diabetes Prevalence by Alberta Community over 1,000 Population, 2011-2012 (ages ≥ 1 years) Siksika 146 Piikano 147 Saddle Lake 125 White Fish Lake 128 Blood 148 Ermineskin 138 Unipouheos 121 Stoney 142, 143, 144 Stony Plain 135 Big Lakes Opportunity No. 17 Fox Lake 162 Fox Creek Swan Hills Northern Sunrise County Cardston Rockyford McLennan Vilna Standard Strathmore High Prairie Kneehill County Valleyview Lac la Biche Wheatland County St. Paul County No. 19 Bassano Fort Macleod Rycroft Clyde Coronation Wood Buffalo Brooks Calmar Bruderheim Slave Lake Grande Cache Andrew Bon Accord Gibbons Northern Lights No. 22 Wetaskiwin Raymond Westlock Bonnyville No. 87 Magrath Athabasca County No. 12 Beiseker Morinville Mundare Devon High Level Castor Lac Ste. Anne County Edson Rainbow Lake Redwater Smoky Lake Warner Rocky Mountain House Redcliff Longview Hines Creek Oyen Two Hills Birch Hills County Edmonton Millet Newell County No. 4 Leduc Glendon Warburg Vegreville Thorhild Wabamun Milk River Mackenzie No. 23 Bonnyville Coalhurst Kitscoty Lamont Nampa Ponoka Thorsby Hinton Lethbridge Diabetes Westlock County St. Paul Legal Daysland Thorhild County No. 7 Ryley Hardisty Provost No. 52 Mayerthorpe Prevalence: Duchess Boyle Grande Prairie Manning Medicine Hat Killam Spruce Grove Tofield Camrose Trochu Drayton Valley It Matters Forestburg Elk Point Alberta Beach Lloydminster (Part) Breton Sangudo Crowsnest Pass Where You Live Picture Butte Grimshaw New Norway Peace River Irma New Sarepta Stony Plain Yellowhead County Wainwright Coaldale Whitecourt Onoway Camrose County No. 22 Stirling Fairview Grande Prairie County No. 1 Cardston County Parkland County Chestermere Sedgewick Prevalence is the number of cases of Wetaskiwin County No.