Recent Advances Susan Pynea*, David R Adamsb and Nigel
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gene Symbol Gene Description ACVR1B Activin a Receptor, Type IB
Table S1. Kinase clones included in human kinase cDNA library for yeast two-hybrid screening Gene Symbol Gene Description ACVR1B activin A receptor, type IB ADCK2 aarF domain containing kinase 2 ADCK4 aarF domain containing kinase 4 AGK multiple substrate lipid kinase;MULK AK1 adenylate kinase 1 AK3 adenylate kinase 3 like 1 AK3L1 adenylate kinase 3 ALDH18A1 aldehyde dehydrogenase 18 family, member A1;ALDH18A1 ALK anaplastic lymphoma kinase (Ki-1) ALPK1 alpha-kinase 1 ALPK2 alpha-kinase 2 AMHR2 anti-Mullerian hormone receptor, type II ARAF v-raf murine sarcoma 3611 viral oncogene homolog 1 ARSG arylsulfatase G;ARSG AURKB aurora kinase B AURKC aurora kinase C BCKDK branched chain alpha-ketoacid dehydrogenase kinase BMPR1A bone morphogenetic protein receptor, type IA BMPR2 bone morphogenetic protein receptor, type II (serine/threonine kinase) BRAF v-raf murine sarcoma viral oncogene homolog B1 BRD3 bromodomain containing 3 BRD4 bromodomain containing 4 BTK Bruton agammaglobulinemia tyrosine kinase BUB1 BUB1 budding uninhibited by benzimidazoles 1 homolog (yeast) BUB1B BUB1 budding uninhibited by benzimidazoles 1 homolog beta (yeast) C9orf98 chromosome 9 open reading frame 98;C9orf98 CABC1 chaperone, ABC1 activity of bc1 complex like (S. pombe) CALM1 calmodulin 1 (phosphorylase kinase, delta) CALM2 calmodulin 2 (phosphorylase kinase, delta) CALM3 calmodulin 3 (phosphorylase kinase, delta) CAMK1 calcium/calmodulin-dependent protein kinase I CAMK2A calcium/calmodulin-dependent protein kinase (CaM kinase) II alpha CAMK2B calcium/calmodulin-dependent -

Stimulating the Expression of Sphingosine Kinase 1 (Sphk1) Is Bene�Cial to Reduce Acrylamide-Induced Nerve Cell Damage
Stimulating the Expression of Sphingosine Kinase 1 (SphK1) is Benecial to Reduce Acrylamide-Induced Nerve Cell Damage Yong-Hui Wu ( [email protected] ) Harbin Medical University https://orcid.org/0000-0002-4838-2947 Sheng-Yuan Wang Harbin Medical University Xiao-Li Wang Harbin Medical University Rui Xin Harbin Medical University Ye Xin Harbin Medical University Rui Wang Harbin Medical University Kun Ma Harbin Medical University Cui-Ping Yu Harbin Medical University Dan Zhang Harbin Medical University Xiao-Rong Zhou Harbin Medical University Wei-Wei Ma Harbin Medical University Chao Wang Harbin Medical University Research Keywords: Acrylamide, SphKl, Neurotoxicity, Apoptosis, MAPK pathway Posted Date: September 28th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-80914/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Stimulating the expression of sphingosine kinase 1 (SphK1) is beneficial to reduce acrylamide-induced nerve cell damage Sheng-Yuan Wang1, Xiao-Li Wang1, Rui Xin1, Ye Xin1, Rui Wang1, Kun Ma2, Cui-Ping Yu1, Dan Zhang1, Xiao-Rong Zhou1, Wei-Wei Ma3, Chao Wang4, Yong-Hui Wu1* 1 Department of Occupational Health, Public Health College, Harbin Medical University, Harbin, P. R. 2 Department of Hygienic Toxicology, Public Health College, Harbin Medical University, Harbin, P. R. 3 Harbin Railway Center for Disease Control and Prevention, Harbin, P. R. 4 Health Commission of Heilongjiang Province. * Address correspondence to this author at: The Department of Occupational Health, Public Health College, Harbin Medical University, 157 Baojian Road, Nan gang District, Harbin, People’s Republic of China 150086. Phone: +86-451-8750-2827, Fax: +86-451-8750-2827, E-mail: [email protected]. -

Lipid Metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives
cancers Review Lipid metabolic Reprogramming: Role in Melanoma Progression and Therapeutic Perspectives 1, 1, 1 2 1 Laurence Pellerin y, Lorry Carrié y , Carine Dufau , Laurence Nieto , Bruno Ségui , 1,3 1, , 1, , Thierry Levade , Joëlle Riond * z and Nathalie Andrieu-Abadie * z 1 Centre de Recherches en Cancérologie de Toulouse, Equipe Labellisée Fondation ARC, Université Fédérale de Toulouse Midi-Pyrénées, Université Toulouse III Paul-Sabatier, Inserm 1037, 2 avenue Hubert Curien, tgrCS 53717, 31037 Toulouse CEDEX 1, France; [email protected] (L.P.); [email protected] (L.C.); [email protected] (C.D.); [email protected] (B.S.); [email protected] (T.L.) 2 Institut de Pharmacologie et de Biologie Structurale, CNRS, Université Toulouse III Paul-Sabatier, UMR 5089, 205 Route de Narbonne, 31400 Toulouse, France; [email protected] 3 Laboratoire de Biochimie Métabolique, CHU Toulouse, 31059 Toulouse, France * Correspondence: [email protected] (J.R.); [email protected] (N.A.-A.); Tel.: +33-582-7416-20 (J.R.) These authors contributed equally to this work. y These authors jointly supervised this work. z Received: 15 September 2020; Accepted: 23 October 2020; Published: 27 October 2020 Simple Summary: Melanoma is a devastating skin cancer characterized by an impressive metabolic plasticity. Melanoma cells are able to adapt to the tumor microenvironment by using a variety of fuels that contribute to tumor growth and progression. In this review, the authors summarize the contribution of the lipid metabolic network in melanoma plasticity and aggressiveness, with a particular attention to specific lipid classes such as glycerophospholipids, sphingolipids, sterols and eicosanoids. -

Targeting the Sphingosine Kinase/Sphingosine-1-Phosphate Signaling Axis in Drug Discovery for Cancer Therapy
cancers Review Targeting the Sphingosine Kinase/Sphingosine-1-Phosphate Signaling Axis in Drug Discovery for Cancer Therapy Preeti Gupta 1, Aaliya Taiyab 1 , Afzal Hussain 2, Mohamed F. Alajmi 2, Asimul Islam 1 and Md. Imtaiyaz Hassan 1,* 1 Centre for Interdisciplinary Research in Basic Sciences, Jamia Millia Islamia, Jamia Nagar, New Delhi 110025, India; [email protected] (P.G.); [email protected] (A.T.); [email protected] (A.I.) 2 Department of Pharmacognosy, College of Pharmacy, King Saud University, Riyadh 11451, Saudi Arabia; afi[email protected] (A.H.); [email protected] (M.F.A.) * Correspondence: [email protected] Simple Summary: Cancer is the prime cause of death globally. The altered stimulation of signaling pathways controlled by human kinases has often been observed in various human malignancies. The over-expression of SphK1 (a lipid kinase) and its metabolite S1P have been observed in various types of cancer and metabolic disorders, making it a potential therapeutic target. Here, we discuss the sphingolipid metabolism along with the critical enzymes involved in the pathway. The review provides comprehensive details of SphK isoforms, including their functional role, activation, and involvement in various human malignancies. An overview of different SphK inhibitors at different phases of clinical trials and can potentially be utilized as cancer therapeutics has also been reviewed. Citation: Gupta, P.; Taiyab, A.; Hussain, A.; Alajmi, M.F.; Islam, A.; Abstract: Sphingolipid metabolites have emerged as critical players in the regulation of various Hassan, M..I. Targeting the Sphingosine Kinase/Sphingosine- physiological processes. Ceramide and sphingosine induce cell growth arrest and apoptosis, whereas 1-Phosphate Signaling Axis in Drug sphingosine-1-phosphate (S1P) promotes cell proliferation and survival. -

Sphingosine-1-Phosphate As a Mediator Involved in Development of Fibrotic Diseases
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Kanazawa University Repository for Academic Resources Sphingosine-1-phosphate as a mediator involved in development of fibrotic diseases 著者 Takuwa Yoh, Ikeda Hitoshi, Okamoto Yasuo, Takuwa Noriko, Yoshioka Kazuaki journal or Biochimica et Biophysica Acta - Molecular and publication title Cell Biology of Lipids volume 1831 number 1 page range 185-192 year 2013-01-01 URL http://hdl.handle.net/2297/32827 doi: 10.1016/j.bbalip.2012.06.008 Sphingosine-1-phosphate as a mediator involved in development of fibrotic diseases Yoh Takuwa1§, Hitoshi Ikeda2, Yasuo Okamoto1, Noriko Takuwa1,3, Kazuaki Yoshioka1 1Department of Physiology, Kanazawa University School of Medicine, Kanazawa, Japan, 2Department of Clinical Laboratory Medicine, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan, 3Ishikawa Prefectural Nursing University, Kahoku, Japan §Corresponding author: Yoh Takuwa, M.D., Ph.D., Department of Physiology, Kanazawa University School of Medicine, 13-1 Takara-machi, Kanazawa, 920-8640, Japan, TEL: +81-76-265-2165, FAX: +81-76-234-4223, e-mail: [email protected] 1 Abstract Fibrosis is a pathological process characterized by massive deposition of extracellular matrix (ECM) such as type I/III collagens and fibronectin that are secreted by an expanded pool of myofibroblasts, which are phenotypically altered fibroblasts with more contractile, proliferative, migratory and secretory activities. Fibrosis occurs in various organs including the lung, heart, liver and kidney, resulting in loss of normal tissue architecture and functions. Myofibroblasts could originate from multiple sources including tissue-resident fibroblasts, epithelial and endothelial cells through mechanisms of epithelial/endothelial-mesenchymal transition (EMT/EndMT), and bone marrow-derived circulating progenitors called fibrocytes. -

Kinase-Targeted Cancer Therapies: Progress, Challenges and Future Directions Khushwant S
Bhullar et al. Molecular Cancer (2018) 17:48 https://doi.org/10.1186/s12943-018-0804-2 REVIEW Open Access Kinase-targeted cancer therapies: progress, challenges and future directions Khushwant S. Bhullar1, Naiara Orrego Lagarón2, Eileen M. McGowan3, Indu Parmar4, Amitabh Jha5, Basil P. Hubbard1 and H. P. Vasantha Rupasinghe6,7* Abstract The human genome encodes 538 protein kinases that transfer a γ-phosphate group from ATP to serine, threonine, or tyrosine residues. Many of these kinases are associated with human cancer initiation and progression. The recent development of small-molecule kinase inhibitors for the treatment of diverse types of cancer has proven successful in clinical therapy. Significantly, protein kinases are the second most targeted group of drug targets, after the G-protein- coupled receptors. Since the development of the first protein kinase inhibitor, in the early 1980s, 37 kinase inhibitors have received FDA approval for treatment of malignancies such as breast and lung cancer. Furthermore, about 150 kinase-targeted drugs are in clinical phase trials, and many kinase-specific inhibitors are in the preclinical stage of drug development. Nevertheless, many factors confound the clinical efficacy of these molecules. Specific tumor genetics, tumor microenvironment, drug resistance, and pharmacogenomics determine how useful a compound will be in the treatment of a given cancer. This review provides an overview of kinase-targeted drug discovery and development in relation to oncology and highlights the challenges and future potential for kinase-targeted cancer therapies. Keywords: Kinases, Kinase inhibition, Small-molecule drugs, Cancer, Oncology Background Recent advances in our understanding of the fundamen- Kinases are enzymes that transfer a phosphate group to a tal molecular mechanisms underlying cancer cell signaling protein while phosphatases remove a phosphate group have elucidated a crucial role for kinases in the carcino- from protein. -
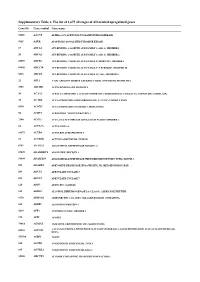
Supplementary Table 1. the List of 1,675 All Stages of AD-Related Upregulated Genes
Supplementary Table 1. The list of 1,675 all stages of AD-related upregulated genes Gene ID Gene symbol Gene name 51146 A4GNT ALPHA-1,4-N-ACETYLGLUCOSAMINYLTRANSFERASE 9625 AATK APOPTOSIS-ASSOCIATED TYROSINE KINASE 19 ABCA1 ATP-BINDING CASSETTE, SUB-FAMILY A (ABC1), MEMBER 1 20 ABCA2 ATP-BINDING CASSETTE, SUB-FAMILY A (ABC1), MEMBER 2 10058 ABCB6 ATP-BINDING CASSETTE, SUB-FAMILY B (MDR/TAP), MEMBER 6 89845 ABCC10 ATP-BINDING CASSETTE, SUB-FAMILY C (CFTR/MRP), MEMBER 10 5826 ABCD4 ATP-BINDING CASSETTE, SUB-FAMILY D (ALD), MEMBER 4 25 ABL1 V-ABL ABELSON MURINE LEUKEMIA VIRAL ONCOGENE HOMOLOG 1 3983 ABLIM1 ACTIN BINDING LIM PROTEIN 1 30 ACAA1 ACETYL-COENZYME A ACYLTRANSFERASE 1 (PEROXISOMAL 3-OXOACYL-COENZYME A THIOLASE) 35 ACADS ACYL-COENZYME A DEHYDROGENASE, C-2 TO C-3 SHORT CHAIN 8310 ACOX3 ACYL-COENZYME A OXIDASE 3, PRISTANOYL 56 ACRV1 ACROSOMAL VESICLE PROTEIN 1 2180 ACSL1 ACYL-COA SYNTHETASE LONG-CHAIN FAMILY MEMBER 1 86 ACTL6A ACTIN-LIKE 6A 93973 ACTR8 ACTIN-RELATED PROTEIN 8 91 ACVR1B ACTIVIN A RECEPTOR, TYPE IB 8747 ADAM21 ADAM METALLOPEPTIDASE DOMAIN 21 27299 ADAMDEC1 ADAM-LIKE, DECYSIN 1 56999 ADAMTS9 ADAM METALLOPEPTIDASE WITH THROMBOSPONDIN TYPE 1 MOTIF, 9 105 ADARB2 ADENOSINE DEAMINASE, RNA-SPECIFIC, B2 (RED2 HOMOLOG RAT) 109 ADCY3 ADENYLATE CYCLASE 3 113 ADCY7 ADENYLATE CYCLASE 7 120 ADD3 ADDUCIN 3 (GAMMA) 125 ADH1C ALCOHOL DEHYDROGENASE 1A (CLASS I), ALPHA POLYPEPTIDE 9370 ADIPOQ ADIPONECTIN, C1Q AND COLLAGEN DOMAIN CONTAINING 165 AEBP1 AE BINDING PROTEIN 1 4299 AFF1 AF4/FMR2 FAMILY, MEMBER 1 173 AFM AFAMIN 79814 AGMAT AGMATINE -

The Effects of Bone Marrow Adipocytes on Metabolic Regulation in Metastatic Prostate Cancer" (2017)
Wayne State University Wayne State University Dissertations 1-1-2017 The ffecE ts Of Bone Marrow Adipocytes On Metabolic Regulation In Metastatic Prostate Cancer Jonathan Diedrich Wayne State University, Follow this and additional works at: https://digitalcommons.wayne.edu/oa_dissertations Part of the Oncology Commons Recommended Citation Diedrich, Jonathan, "The Effects Of Bone Marrow Adipocytes On Metabolic Regulation In Metastatic Prostate Cancer" (2017). Wayne State University Dissertations. 1797. https://digitalcommons.wayne.edu/oa_dissertations/1797 This Open Access Dissertation is brought to you for free and open access by DigitalCommons@WayneState. It has been accepted for inclusion in Wayne State University Dissertations by an authorized administrator of DigitalCommons@WayneState. THE EFFECTS OF BONE MARROW ADIPOCYTES ON METASTATIC PROSTATE CANCER CELL METABOLISM AND SIGNALLING by JONATHAN DRISCOLL DIEDRICH DISSERTATION Submitted to the Graduate School of Wayne State University, Detroit, Michigan in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY 2017 MAJOR: CANCER BIOLOGY Approved By: Advisor Date © COPYRIGHT BY JONATHAN DIEDRICH 2017 All Rights Reserved DEDICATION To my Family, Friends, and Wally ii ACKNOWLEDGMENTS When I joined the Podgorski laboratory in April of 2014, I had finished my rotations and spent some time in a collaborating laboratory honing my technical and creative thinking skills to become a valuable asset to her team; however, I was still unprepared for the exciting journey it would be through Izabela’s laboratory over the last three years. I was extremely lucky to have landed in Dr. Podgorski’s laboratory and will be forever thankful for the tremendous support she has given me to aid in my development as an independent investigator. -

A Phase I Study of ABC294640, a First-In-Class Sphingosine Kinase-2 Inhibitor, in Patients with Advanced Solid Tumors Carolyn D
Published OnlineFirst April 18, 2017; DOI: 10.1158/1078-0432.CCR-16-2363 Cancer Therapy: Clinical Clinical Cancer Research A Phase I Study of ABC294640, a First-in-Class Sphingosine Kinase-2 Inhibitor, in Patients with Advanced Solid Tumors Carolyn D. Britten1, Elizabeth Garrett-Mayer2, Steven H. Chin1, Keisuke Shirai1, Besim Ogretmen3, Tricia A. Bentz4, Alan Brisendine4, Kate Anderton4, Susan L. Cusack5, Lynn W. Maines5, Yan Zhuang5, Charles D. Smith5, and Melanie B. Thomas1 Abstract Purpose: Sphingosine kinases (SK1 and SK2) regulate tumor nausea, vomiting, and fatigue. Among the 4 patients at 750 mg growth by generating the mitogenic and proinflammatory lipid bid, one haddose-limiting grade 3 nausea and vomiting, and 2 were sphingosine 1-phosphate (S1P). This phase I study investigated unable to complete cycle 1 due to diverse drug-related toxicities. the safety, pharmacokinetics, pharmacodynamics, and antitumor The 500 mg bid dose level was established as the recommended activity of ABC294640, a first-in-class orally available inhibitor of phase II dose. ABC294640 administration resulted in decreases in SK2. S1P levels over the first 12 hours, withreturn to baseline at 24 hours. Experimental Design: Escalating doses of ABC294640 were The best response was a partial response in a patient with cholan- administered orally to patients with advanced solid tumors in giocarcinoma at 250 mg qd, and stable disease was observed in 6 sequential cohorts at the following dose levels: 250 mg qd, 250 patients with various solid tumors across dose levels. mg bid, 500 mg bid, and 750 mg bid, continuously in cycles of 28 Conclusions: At 500 mg bid, ABC294640 is well tolerated days. -

Sphingosine Kinase 1–Mediated Inhibition of Fas Death Signaling in Rheumatoid Arthritis B Lymphoblastoid Cells
ARTHRITIS & RHEUMATISM Vol. 54, No. 3, March 2006, pp 754–764 DOI 10.1002/art.21635 © 2006, American College of Rheumatology Sphingosine Kinase 1–Mediated Inhibition of Fas Death Signaling in Rheumatoid Arthritis B Lymphoblastoid Cells Xiujun Pi, Shi-Yu Tan, Michael Hayes, Liqun Xiao, James A. Shayman, Song Ling, and Joseph Holoshitz Objective. It is becoming increasingly apparent increased levels of S1P. Real-time PCR analysis showed that B cells play an important role in the pathogenesis higher SPHK-1 mRNA expression levels in RA patients of rheumatoid arthritis (RA). Due to the scarcity of B compared with paired controls. Increased SPHK-1 (but cells in RA, it has been technically difficult to function- not SPHK-2) mRNA levels were observed in synovial ally characterize B cell apoptosis in this disease. As a tissue from RA patients. Competitive inhibitors of necessary first step to identify candidate aberrations, we SPHK reversed the resistance of RA LCLs to Fas- investigated Fas-mediated signaling events in immortal- induced apoptosis. Additionally, resistance to Fas- ized peripheral blood B lymphoblastoid cell lines mediated signaling was reversed by siRNA oligonucleo- (LCLs) from patients with RA and controls. tides specific for SPHK-1 but not by oligonucleotides Methods. Cell death was determined by the MTS specific for SPHK-2. assay, and apoptosis was detected by the TUNEL assay Conclusion. These findings demonstrate disease- and DNA laddering. Proteolytic activation of caspase 3 specific resistance to Fas-mediated death signaling in was determined by immunoblotting, and its enzymatic patients with RA and implicate increased SPHK-1 ac- activity was determined by a fluorometric technique. -

An Entirely Specific Type I A-Kinase Anchoring Protein That Can
An entirely specific type I A-kinase anchoring PNAS PLUS protein that can sequester two molecules of protein kinase A at mitochondria Christopher K. Meansa, Birgitte Lygrenb, Lorene K. Langeberga, Ankur Jainc, Rose E. Dixond, Amanda L. Vegad, Matthew G. Golda, Susanna Petrosyane, Susan S. Taylorf, Anne N. Murphye, Taekjip Hac,g, Luis F. Santanad, Kjetil Taskenb, and John D. Scotta,1 aHoward Hughes Medical Institute, Department of Pharmacology, University of Washington School of Medicine, 1959 Pacific Avenue NE, Seattle, WA 98195; bBiotechnology Center of Oslo and Center for Molecular Medicine Norway, Nordic European Molecular Biology Laboratory Partnership, University of Oslo, N-0317 Oslo, Norway; cCenter for Biophysics and Computational Biology, University of Illinois at Urbana-Champaign, Urbana, IL 61822; dDepartment of Physiology and Biophysics, University of Washington, Seattle, WA 98195; eDepartment of Pharmacology, University of California at San Diego, La Jolla, CA 92093; fHoward Hughes Medical Institute, Department of Chemistry and Biochemistry, University of California at San Diego, La Jolla, CA 92093; and gHoward Hughes Medical Institute, Department of Physics and Center for the Physics of Living Cells, University of Illinois at Urbana-Champaign, Urbana, IL 61822 Edited by* Joseph A. Beavo, University of Washington School of Medicine, Seattle, WA, and approved October 5, 2011 (received for review May 6, 2011) A-kinase anchoring proteins (AKAPs) tether the cAMP-dependent Two C subunit genes encode the ubiquitously expressed Cα and protein kinase (PKA) to intracellular sites where they preferentially Cβ isoforms (14). The four R subunit genes are subdivided into phosphorylate target substrates. Most AKAPs exhibit nanomolar two classes: type I [RI (RIα and RIβ)] and type II [RII (RIIα and affinity for the regulatory (RII) subunit of the type II PKA holoen- RIIβ)] (15–17). -

Dema and Faust Et Al., Suppl. Material 2020.02.03
Supplementary Materials Cyclin-dependent kinase 18 controls trafficking of aquaporin-2 and its abundance through ubiquitin ligase STUB1, which functions as an AKAP Dema Alessandro1,2¶, Dörte Faust1¶, Katina Lazarow3, Marc Wippich3, Martin Neuenschwander3, Kerstin Zühlke1, Andrea Geelhaar1, Tamara Pallien1, Eileen Hallscheidt1, Jenny Eichhorst3, Burkhard Wiesner3, Hana Černecká1, Oliver Popp1, Philipp Mertins1, Gunnar Dittmar1, Jens Peter von Kries3, Enno Klussmann1,4* ¶These authors contributed equally to this work 1Max Delbrück Center for Molecular Medicine in the Helmholtz Association (MDC), Robert- Rössle-Strasse 10, 13125 Berlin, Germany 2current address: University of California, San Francisco, 513 Parnassus Avenue, CA 94122 USA 3Leibniz-Forschungsinstitut für Molekulare Pharmakologie (FMP), Robert-Rössle-Strasse 10, 13125 Berlin, Germany 4DZHK (German Centre for Cardiovascular Research), Partner Site Berlin, Oudenarder Strasse 16, 13347 Berlin, Germany *Corresponding author Enno Klussmann Max Delbrück Center for Molecular Medicine Berlin in the Helmholtz Association (MDC) Robert-Rössle-Str. 10, 13125 Berlin Germany Tel. +49-30-9406 2596 FAX +49-30-9406 2593 E-mail: [email protected] 1 Content 1. CELL-BASED SCREENING BY AUTOMATED IMMUNOFLUORESCENCE MICROSCOPY 3 1.1 Screening plates 3 1.2 Image analysis using CellProfiler 17 1.4 Identification of siRNA affecting cell viability 18 1.7 Hits 18 2. SUPPLEMENTARY TABLE S4, FIGURES S2-S4 20 2 1. Cell-based screening by automated immunofluorescence microscopy 1.1 Screening plates Table S1. Genes targeted with the Mouse Protein Kinases siRNA sub-library. Genes are sorted by plate and well. Accessions refer to National Center for Biotechnology Information (NCBI, BLA) entries. The siRNAs were arranged on three 384-well microtitre platres.