AAFP Response to VHA Health Professionals Scope of Practice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

June 9, 2020 the Honorable Nancy Pelosi the Honorable Mitch
June 9, 2020 The Honorable Nancy Pelosi The Honorable Mitch McConnell Speaker of the House of Representatives Senate Majority Leader U.S. Capitol Building, H-222 U.S. Capitol Building, S-230 Washington, DC 20515 Washington, DC 20510 The Honorable Kevin McCarthy The Honorable Charles Schumer House Republican Leader Senate Democratic Leader U.S. Capitol Building, H-204 U.S. Capitol Building, S-221 Washington, DC 20515 Washington, DC 20510 Dear Speaker Pelosi, Leader McConnell, Leader McCarthy, and Leader Schumer: The undersigned state, specialty, and national medical associations represent hundreds of thousands of frontline medical and mental health physicians who are diagnosing, testing, treating, and counseling millions of our nation’s patients in response to the COVID-19 pandemic. During this unprecedented national health emergency, physicians and other health care professionals have been putting themselves at risk every day while facing shortages of medical supplies and safety equipment, and making critical medical decisions based on changing directives and guidance. These physicians and other health care professionals are now facing the threat of years of costly litigation due to the extraordinary circumstances. As the House and Senate continue to work on the next COVID-19 relief package, we strongly urge you to include the targeted and limited liability protections that are in the bipartisan bill, H.R. 7059, the “Coronavirus Provider Protection Act.” The public health emergency triggered by the COVID-19 pandemic has created unprecedented challenges to our nation’s health care system. In addition to facing inadequate supplies and safety equipment, physicians, hospitals, and other frontline health care professionals have been faced with rapidly changing guidance and directives from all levels of government. -
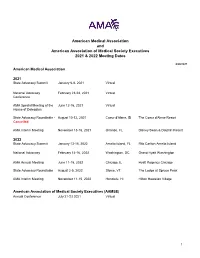
AMA and AAMSE 2021 & 2022 Meeting Dates
American Medical Association and American Association of Medical Society Executives 2021 & 2022 Meeting Dates 6/28/2021 American Medical Association 2021 State Advocacy Summit January 6-8, 2021 Virtual National Advocacy February 23-24, 2021 Virtual Conference AMA Special Meeting of the June 12-16, 2021 Virtual House of Delegates State Advocacy Roundtable - August 10-12, 2021 Coeur d'Alene, ID The Coeur d'Alene Resort Cancelled AMA Interim Meeting November 13-16, 2021 Orlando, FL Disney Swan & Dolphin Resort 2022 State Advocacy Summit January 13-15, 2022 Amelia Island, FL Ritz Carlton Amelia Island National Advocacy February 14-16, 2022 Washington, DC Grand Hyatt Washington AMA Annual Meeting June 11-15, 2022 Chicago, IL Hyatt Regency Chicago State Advocacy Roundtable August 2-5, 2022 Stowe, VT The Lodge at Spruce Peak AMA Interim Meeting November 11-15, 2022 Honolulu, HI Hilton Hawaiian Village American Association of Medical Society Executives (AAMSE) Annual Conference July 21-23 2021 Virtual 1 State Medical Society Meetings Alaska State Medical Association Annual Meeting May 8, 2021 Virtual Arizona Medical Association Annual Meeting April 16-17, 2021 Virtual Arkansas Medical Society Annual Meeting May 12, 2021 Virtual California Medical Association Annual Meeting October 23-24, 2021 Los Angeles, CA Marriott LA Live Colorado Medical Society Annual Meeting September 18, 2021 Virtual Connecticut State Medical Society Annual Meeting September, TBD, 2021 TBD TBD Florida Medical Association Annual Meeting July 31 - August 1, 2021 Orlando, -

American Medical Association Resident and Fellow Section
MEDICAL SOCIETY OF DELAWARE COUNCIL Resolution: 01 (A-19) Introduced by: Psychiatric Society of Delaware Neil S. Kaye, MD, DLFAPA Subject: Commitment to Ethics Whereas, The medical profession has adhered to a Code of Ethics since the 5th Century BCE; and Whereas, Such Codes have included the Oath of Hippocrates and the Oath of Maimonides; and Whereas, In 1803 Thomas Percival introduced our country’s first medical ethics standards; and Whereas, These codes were adopted by the AMA in 1847; and Whereas, The Code of Medical Ethics has been revised continuously, most recently in 2016; and Whereas, Forces from both within the house of medicine and outside of the house of medicine continually try to influence the practice of medicine; and Whereas, What has never changed in any of these ethical codes is the requirement that physicians focus 100% of their efforts on healing; therefore be it RESOLVED, That the Medical Society of Delaware will continue to recognize the AMA Code of Medical Ethics as binding on all decisions made by the organization and its members; and be it further RESOLVED, That the Medical Society of Delaware will actively resist all attempts to lessen its ethical standards as enumerated in the AMA Code of Medical Ethics. Fiscal Note: Undetermined 1American Medical Association. Code of Medical Ethics of the American Medical Association. Chicago, IL: American Medical Association; 2017 MEDICAL SOCIETY OF DELAWARE COUNCIL Resolution: 02 (A-19) Introduced by: Robert J. Varipapa, MD Subject: MSD Support of Medical Aid in Dying (MAID) -

Secretary of Veterans' Affairs
June 24, 2020 The Honorable Robert Wilkie Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary Wilkie: The undersigned medical associations and medical specialty societies are writing to register serious concerns with the Health Care Professional Practice in VA Memorandum (Memorandum) issued by the Office of the Under Secretary of Health on April 21, 2020, and underlying Directive 1899 (Directive). The undersigned organizations urge the Secretary to amend Directive 1899 as it relates to allowing non-physician healthcare professionals in 32 specialties to operate “within the full scope of their license, registration, or certification” and rescind the Memorandum as it relates to encouraging all VA medical facilities to allow CRNAs to practice without physician oversight during the national health emergency. The undersigned organizations are very concerned Directive 1899 preempts state scope of practice laws. Directive 1899 memorializes U.S. Department of Veterans Affairs (VA) policy allowing VA health care professionals to practice across state lines and establishes new policy allowing VA health care professionals to operate within the full scope of their license, registration, or certification. This combination in effect circumvents state scope of practice laws for the 32 health care professionals defined in the directive. Such a far-reaching expansion is overly broad, unnecessary and threatens the health and safety of patients within the VA system. As state scope of practice laws vary across these professions and across states, we urge the Secretary to amend the directive to defer to state scope of practice laws, similar to the language related to psychologists in Appendix B of the Directive. -

U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420
June 24, 2020 The Honorable Robert Wilkie Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary Wilkie: The undersigned medical associations and medical specialty societies are writing to register serious concerns with the Health Care Professional Practice in VA Memorandum (Memorandum) issued by the Office of the Under Secretary of Health on April 21, 2020, and underlying Directive 1899 (Directive). The undersigned organizations urge the Secretary to amend Directive 1899 as it relates to allowing non-physician healthcare professionals in 32 specialties to operate “within the full scope of their license, registration, or certification” and rescind the Memorandum as it relates to encouraging all VA medical facilities to allow CRNAs to practice without physician oversight during the national health emergency. The undersigned organizations are very concerned Directive 1899 preempts state scope of practice laws. Directive 1899 memorializes U.S. Department of Veterans Affairs (VA) policy allowing VA health care professionals to practice across state lines and establishes new policy allowing VA health care professionals to operate within the full scope of their license, registration, or certification. This combination in effect circumvents state scope of practice laws for the 32 health care professionals defined in the directive. Such a far-reaching expansion is overly broad, unnecessary and threatens the health and safety of patients within the VA system. As state scope of practice laws vary across these professions and across states, we urge the Secretary to amend the directive to defer to state scope of practice laws, similar to the language related to psychologists in Appendix B of the Directive. -
U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420
July 29, 2021 The Honorable Denis McDonough Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary McDonough: The undersigned physician organizations have recently learned of the Department of Veterans Affairs (VA) Supremacy Project. We are writing to express our serious concerns with the VA’s efforts to develop National Standards of Practice for physicians and other health professionals that supersede state scope of practice and licensure laws. In particular, we are dismayed that the VA has not provided a transparent process by which public stakeholders are provided an adequate opportunity to review and provide meaningful input into the standards of practice. Furthermore, based on what we have learned about the VA’s approach to developing the standards of practice for 48 categories of health professionals, we believe the VA has failed to consider that these health professionals do not operate in isolation but rather as a team. Yet, the VA is creating and moving standards forward independent of one another. In order to provide the best care for our Veterans, the VA must engage in a systematic examination of how all these standards will fit together and affect the health professional team. The policies the VA is seeking to overhaul will have implications for standards of care beyond the VA. It is therefore vitally important that the VA initiate a meaningful process for the collection, dissemination, and inclusion of stakeholder input as early into the process as possible. As physicians, we want to ensure that our nation’s Veterans receive the best medical care possible, including care from physician-led teams which research has shown results in the highest quality of care for patients.1 We therefore urge the VA to reconsider its implementation of the National Standards of Practice. -

July 16, 2019 the Honorable Frank Pallone, Jr. the Honorable Greg
July 16, 2019 The Honorable Frank Pallone, Jr. The Honorable Greg Walden Chairman Ranking Member Committee on Energy and Commerce Committee on Energy and Commerce 2125 Rayburn House Office Building 2322A Rayburn House Office Building Washington, DC 20515 Washington, DC 20515 Dear Chairman Pallone and Ranking Member Walden: The undersigned organizations believe a fair and equitable independent dispute resolution (IDR) process is an essential component of any surprise billing solution and should be included in any final bill coming out of the House Energy and Commerce Committee to ensure the legislation is balanced and does not result either in unfair payments to physicians or unreasonable bills to health plans. We fully support the central goal of the No Surprises Act to protect patients from surprise medical bills when they unknowingly receive services from out-of-network providers in in-network facilities. We also support the provisions in the No Surprises Act that would ensure patients are only responsible for in-network cost-sharing in these situations, and that their cost-sharing count toward in-network deductibles and out-of-pocket maximums. We also agree that patients should be taken out of any payment disputes between physicians and insurers that arise from these situations. However, once the patient is protected from surprise medical bills, it is equally important to ensure that the legislation does not create new imbalances in the private health care marketplace by undermining the ability of doctors to secure fair reimbursement for their services. The health insurance marketplace is already heavily consolidated. Instituting a federal government rate-setting scheme that allows private insurers to force discounted rates on physicians, hospitals and other health care providers based on their median 2019 in-network rates puts both network and non-network providers at a disadvantage and will result in sudden drops in reimbursement for emergency and nonemergency hospital-based care. -

Fs and Ethical with No Clear Consensus
Medical Professional Associations that Recognize Medical Aid in Dying A growing number of national and state medical organizations have endorsed or adopted a neutral position regarding medical aid in dying as an end-of-life option for mentally capable, terminally ill adults. Physician Support for Medical Aid in Dying Is Strong Medscape Poll, December 20161 A December 2016 Medscape poll of more than 7,500 U.S. physicians from more than 25 specialties demonstrated a significant increase in support for medical aid in dying from 2010. lethal doses of medications,”31% “strongly” Today well over half (57%) of the physicians supported this end-of-life care option. surveyed endorse the idea of medical aid in dying, agreeing that “Physician assisted death should be allowed for terminally ill patients.” The Maryland State Medical Society (MedChi) survey, June-July 20163 The Colorado Medical Society Member ➔ Six out of 10 Maryland physicians (60%) Survey, February 20162 supported changing the Maryland State ➔ Overall, 56% of CMS members are in favor of Medical Society’s position on Maryland’s “physician-assisted suicide, where adults in 2016 aid-in-dying legislation from opposing Colorado could obtain and use prescriptions the bill to supporting it (47%) or adopting a from their physicians for self-administered, neutral stance (13%). ➔ Among the physicians surveyed who were current members of the Maryland State Medical Society, 65 percent supported 1 Medscape Ethics Report 2016: Life, Death, and Pain, changing the organization’s position to December 23, 2016. Available from supporting the aid-in-dying bill (50.2%) or http://www.medscape.com/features/ slideshow/ethics2016-part2#page=2 adopting a neutral stance (14.6%). -

November 10, 2020 the Honorable
November 10, 2020 The Honorable Seema Verma Administrator Centers for Medicare & Medicaid Services 200 Independence Avenue SW, Room 445 Washington, DC 20201 Dear Administrator Verma: The undersigned organizations represent the hundreds of thousands of physicians who provide care for our nation’s patients every day. The COVID-19 (2019 novel coronavirus) public health emergency (PHE) has placed unprecedented strain on our physician members, including ongoing threats to their financial viability due to months of lost revenue from practice closures and/or operating at reduced capacity. In July and August 2020, the American Medical Association (AMA) surveyed 3,500 physicians who provided at least 20 hours of patient care per week prior to the pandemic.1 A strong majority (81%) of surveyed physicians said revenue was still lower than pre-pandemic, with an average drop in revenue of 32%. Compounding the financial stress of lost revenue, practices are also incurring additional costs for heightened infection control protocols and personal protective equipment (PPE). To help address the significant fiscal pressures placed on physicians by the COVID-19 pandemic, we urge the Centers for Medicare & Medicaid Services (CMS) to immediately implement and pay for Current Procedural Terminology® (CPT) code 99072 to compensate practices for the additional supplies and new staff activities required to provide safe patient care during the PHE. We recognize and appreciate the significant support and flexibility CMS has provided to physician practices. However, it is imperative that CMS specifically compensate physicians for the additional expenses involved in treating patients during the PHE. Practices incur significant costs in implementing the increased infection control measures required to provide safe care during the COVID-19 pandemic. -

Physicians' Foundation for Health Systems Excellence
INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATIO INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLENCE INNOVATION EXCELLEN INNOVATION -

February 12, 2021 the Honorable Nancy Pelosi Speaker U.S. House
February 12, 2021 The Honorable Nancy Pelosi The Honorable Charles Schumer Speaker Majority Leader U.S. House of Representatives U.S. Senate Washington, DC 20515 Washington, DC 20510 The Honorable Kevin McCarthy The Honorable Mitch McConnell Minority Leader Minority Leader U.S. House of Representatives U.S. Senate Washington, DC 20515 Washington, DC 20510 Dear Speaker Pelosi, Majority Leader Schumer, Leader McConnell, and Leader McCarthy: The American Medical Association and undersigned national specialty and state medical societies represent the vast majority of physicians practicing in the United States, many of whom continue to provide frontline care to Medicare patients as the COVID-19 global pandemic persists across the country. We are deeply concerned that persistently high COVID-19 rates will continue to stress the entire health care system, especially physician practices. To help alleviate the unrelenting fiscal demands of the pandemic, we strongly urge Congress to pass legislation that would extend the congressionally enacted moratorium on Medicare sequester cuts through the duration of the public health emergency (PHE). We appreciate that Congress recognized early on during the pandemic the severe financial strain facing our nation’s health care system, including physician practices, and provided a much-needed reprieve from the two percent Medicare payment sequester through the remainder of 2020 in the Coronavirus Aid, Relief, and Economic Security (CARES) Act. We also applaud Congress for including in the Consolidated Appropriations Act, 2021 an extension of the sequester moratorium until March 31, 2021. Even with the encouraging development and deployment of an effective vaccine, the fact remains that physician practices will continue to face overwhelming financial challenges and pressures associated with higher overhead costs (e.g., personal protective equipment) and lost revenue due to fewer patient visits and delayed elective procedures. -

US Department of Veterans Affairs
July 29, 2021 The Honorable Denis McDonough Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary McDonough: The undersigned physician organizations have recently learned of the Department of Veterans Affairs (VA) Supremacy Project. We are writing to express our serious concerns with the VA’s efforts to develop National Standards of Practice for physicians and other health professionals that supersede state scope of practice and licensure laws. In particular, we are dismayed that the VA has not provided a transparent process by which public stakeholders are provided an adequate opportunity to review and provide meaningful input into the standards of practice. Furthermore, based on what we have learned about the VA’s approach to developing the standards of practice for 48 categories of health professionals, we believe the VA has failed to consider that these health professionals do not operate in isolation but rather as a team. Yet, the VA is creating and moving standards forward independent of one another. In order to provide the best care for our Veterans, the VA must engage in a systematic examination of how all these standards will fit together and affect the health professional team. The policies the VA is seeking to overhaul will have implications for standards of care beyond the VA. It is therefore vitally important that the VA initiate a meaningful process for the collection, dissemination, and inclusion of stakeholder input as early into the process as possible. As physicians, we want to ensure that our nation’s Veterans receive the best medical care possible, including care from physician-led teams which research has shown results in the highest quality of care for patients.1 We therefore urge the VA to reconsider its implementation of the National Standards of Practice.