S. 1731) Was Introduced in the U.S
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

AAFP Letter to CMS on Prior Authorizations in Medicare
February 28, 2019 The Honorable Seema Verma Administrator Centers for Medicare & Medicaid Services U.S. Department of Health and Human Services Hubert H. Humphrey Building, Room 445–G 200 Independence Avenue, SW Washington, DC 20201 Dear Administrator Verma: The undersigned organizations are writing to urge the Centers for Medicare & Medicaid Services (CMS) to provide guidance to Medicare Advantage (MA) plans on prior authorization (PA) processes through its 2020 Call Letter. CMS’ guidance should direct plans to target PA requirements where they are needed most. Specifically, CMS should require MA plans to selectively apply PA requirements and provide examples of criteria to be used for such programs, including, for example, ordering/prescribing patterns that align with evidence- based guidelines and historically high PA approval rates. At a time when CMS has prioritized regulatory burden reduction in the patient-provider relationship through its Patients Over Paperwork initiative, we believe such guidance will help promote safe, timely, and affordable access to care for patients; enhance efficiency; and reduce administrative burden on physician practices. A Consensus Statement on Improving the Prior Authorization Process, issued by the AMA, the American Hospital Association, America’s Health Insurance Plans, the American Pharmacists Association, Blue Cross Blue Shield Association, and the Medical Group Management Association in January 2018, identified opportunities to improve the prior authorization process, with the goals of promoting safe, timely, and affordable access to evidence-based care for patients; enhancing efficiency; and reducing administrative burdens.1 It notes that the PA process can be burdensome for all involved—health care providers, health plans, and patients—and that plans should target PA requirements where they are needed most. -

June 9, 2020 the Honorable Nancy Pelosi the Honorable Mitch
June 9, 2020 The Honorable Nancy Pelosi The Honorable Mitch McConnell Speaker of the House of Representatives Senate Majority Leader U.S. Capitol Building, H-222 U.S. Capitol Building, S-230 Washington, DC 20515 Washington, DC 20510 The Honorable Kevin McCarthy The Honorable Charles Schumer House Republican Leader Senate Democratic Leader U.S. Capitol Building, H-204 U.S. Capitol Building, S-221 Washington, DC 20515 Washington, DC 20510 Dear Speaker Pelosi, Leader McConnell, Leader McCarthy, and Leader Schumer: The undersigned state, specialty, and national medical associations represent hundreds of thousands of frontline medical and mental health physicians who are diagnosing, testing, treating, and counseling millions of our nation’s patients in response to the COVID-19 pandemic. During this unprecedented national health emergency, physicians and other health care professionals have been putting themselves at risk every day while facing shortages of medical supplies and safety equipment, and making critical medical decisions based on changing directives and guidance. These physicians and other health care professionals are now facing the threat of years of costly litigation due to the extraordinary circumstances. As the House and Senate continue to work on the next COVID-19 relief package, we strongly urge you to include the targeted and limited liability protections that are in the bipartisan bill, H.R. 7059, the “Coronavirus Provider Protection Act.” The public health emergency triggered by the COVID-19 pandemic has created unprecedented challenges to our nation’s health care system. In addition to facing inadequate supplies and safety equipment, physicians, hospitals, and other frontline health care professionals have been faced with rapidly changing guidance and directives from all levels of government. -
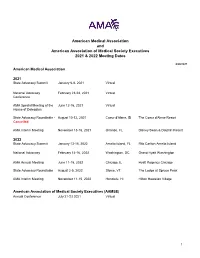
AMA and AAMSE 2021 & 2022 Meeting Dates
American Medical Association and American Association of Medical Society Executives 2021 & 2022 Meeting Dates 6/28/2021 American Medical Association 2021 State Advocacy Summit January 6-8, 2021 Virtual National Advocacy February 23-24, 2021 Virtual Conference AMA Special Meeting of the June 12-16, 2021 Virtual House of Delegates State Advocacy Roundtable - August 10-12, 2021 Coeur d'Alene, ID The Coeur d'Alene Resort Cancelled AMA Interim Meeting November 13-16, 2021 Orlando, FL Disney Swan & Dolphin Resort 2022 State Advocacy Summit January 13-15, 2022 Amelia Island, FL Ritz Carlton Amelia Island National Advocacy February 14-16, 2022 Washington, DC Grand Hyatt Washington AMA Annual Meeting June 11-15, 2022 Chicago, IL Hyatt Regency Chicago State Advocacy Roundtable August 2-5, 2022 Stowe, VT The Lodge at Spruce Peak AMA Interim Meeting November 11-15, 2022 Honolulu, HI Hilton Hawaiian Village American Association of Medical Society Executives (AAMSE) Annual Conference July 21-23 2021 Virtual 1 State Medical Society Meetings Alaska State Medical Association Annual Meeting May 8, 2021 Virtual Arizona Medical Association Annual Meeting April 16-17, 2021 Virtual Arkansas Medical Society Annual Meeting May 12, 2021 Virtual California Medical Association Annual Meeting October 23-24, 2021 Los Angeles, CA Marriott LA Live Colorado Medical Society Annual Meeting September 18, 2021 Virtual Connecticut State Medical Society Annual Meeting September, TBD, 2021 TBD TBD Florida Medical Association Annual Meeting July 31 - August 1, 2021 Orlando, -

AAFP Response to VHA Health Professionals Scope of Practice
January 7, 2021 Robert Wilkie Secretary Department of Veterans Affairs 810 Vermont Ave. NW, Room 1068 Washington, DC 20420 Re: RIN 2900–AQ94—Authority of VA Professionals to Practice Health Care Dear Secretary Wilkie, The undersigned physician organizations representing national specialty and state medical societies are writing in opposition to the Department of Veterans Affairs’ Interim Final Rule, entitled “Authority of VA Professionals to Practice Health Care,” which permits virtually all VHA-employed non-physician providers (NPPs) to practice without the clinical supervision of physicians and without regard to state scope of practice law. NPPs are an integral part of physician-led health care teams. However, NPPs cannot substitute for physicians especially when it comes to diagnosing complex medical conditions, developing comprehensive treatment plans, ensuring that procedures are properly performed, and managing highly involved and complicated patient cases. Nowhere is this more important than at the Department of Veterans Affairs (VA), which delivers multifaceted medical care to veterans, including those with traumatic brain injuries and other serious medical and mental health issues. As such, our nation’s veterans deserve high quality health care that is overseen by physicians. For the reasons below, the undersigned organizations strongly oppose the Interim Final Rule (IFR) and urge the VA to rescind the IFR and consider policy alternatives that prioritize physician led team-based care. The IFR violates the Administrative Procedure -

American Medical Association Resident and Fellow Section
MEDICAL SOCIETY OF DELAWARE COUNCIL Resolution: 01 (A-19) Introduced by: Psychiatric Society of Delaware Neil S. Kaye, MD, DLFAPA Subject: Commitment to Ethics Whereas, The medical profession has adhered to a Code of Ethics since the 5th Century BCE; and Whereas, Such Codes have included the Oath of Hippocrates and the Oath of Maimonides; and Whereas, In 1803 Thomas Percival introduced our country’s first medical ethics standards; and Whereas, These codes were adopted by the AMA in 1847; and Whereas, The Code of Medical Ethics has been revised continuously, most recently in 2016; and Whereas, Forces from both within the house of medicine and outside of the house of medicine continually try to influence the practice of medicine; and Whereas, What has never changed in any of these ethical codes is the requirement that physicians focus 100% of their efforts on healing; therefore be it RESOLVED, That the Medical Society of Delaware will continue to recognize the AMA Code of Medical Ethics as binding on all decisions made by the organization and its members; and be it further RESOLVED, That the Medical Society of Delaware will actively resist all attempts to lessen its ethical standards as enumerated in the AMA Code of Medical Ethics. Fiscal Note: Undetermined 1American Medical Association. Code of Medical Ethics of the American Medical Association. Chicago, IL: American Medical Association; 2017 MEDICAL SOCIETY OF DELAWARE COUNCIL Resolution: 02 (A-19) Introduced by: Robert J. Varipapa, MD Subject: MSD Support of Medical Aid in Dying (MAID) -

Secretary of Veterans' Affairs
June 24, 2020 The Honorable Robert Wilkie Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary Wilkie: The undersigned medical associations and medical specialty societies are writing to register serious concerns with the Health Care Professional Practice in VA Memorandum (Memorandum) issued by the Office of the Under Secretary of Health on April 21, 2020, and underlying Directive 1899 (Directive). The undersigned organizations urge the Secretary to amend Directive 1899 as it relates to allowing non-physician healthcare professionals in 32 specialties to operate “within the full scope of their license, registration, or certification” and rescind the Memorandum as it relates to encouraging all VA medical facilities to allow CRNAs to practice without physician oversight during the national health emergency. The undersigned organizations are very concerned Directive 1899 preempts state scope of practice laws. Directive 1899 memorializes U.S. Department of Veterans Affairs (VA) policy allowing VA health care professionals to practice across state lines and establishes new policy allowing VA health care professionals to operate within the full scope of their license, registration, or certification. This combination in effect circumvents state scope of practice laws for the 32 health care professionals defined in the directive. Such a far-reaching expansion is overly broad, unnecessary and threatens the health and safety of patients within the VA system. As state scope of practice laws vary across these professions and across states, we urge the Secretary to amend the directive to defer to state scope of practice laws, similar to the language related to psychologists in Appendix B of the Directive. -

State Medical Society Membership Requirements
State Medical Society Membership Requirements State Medical Society Representation‐ Updated June 2013 Recently, ASAM staff contacted each state medical society requesting required procedures for ASAM chapters to obtain official membership in the medical society’s governing body. Below are the responses received – Alaska: ASMA’s current bylaws call for House of Delegate members to be elected by the local medical society. There is no representation of specialty societies within the House of Delegates. Arizona: A state specialty or subspecialty society with 250 or fewer members shall be entitled to representation in the House of Delegates by one delegate and a specialty or subspecialty society with more than 250 members shall be entitled to 2 delegates if (1) the specialty or subspecialty is recognized by the American Board of Medical Specialties; (2) the specialty or subspecialty society has a minimum of twenty members practicing in Arizona; (3) the specialty or subspecialty society maintains an existing organization or structure with a slate of periodically elected officers, a constitution and bylaws and a frequency of meeting at least once a year; (4) by a vote of the House it shall be deemed to be in the best interests of the Association. Specialty or subspecialty society delegates shall be the society president or designee(s) who shall be members of the Association (http://www.azmed.org/arma‐governance). California: Each statewide specialty organization recognized by the House of Delegates shall be entitled to one (1) delegate and one (1) alternate. Specialty organizations having five hundred (500) or more members who are regular active members of CMA shall have one (1) additional delegate and alternate, plus one additional delegate and alternate for each full five hundred (500) members thereafter who are regular active members of CMA. -

U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420
June 24, 2020 The Honorable Robert Wilkie Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary Wilkie: The undersigned medical associations and medical specialty societies are writing to register serious concerns with the Health Care Professional Practice in VA Memorandum (Memorandum) issued by the Office of the Under Secretary of Health on April 21, 2020, and underlying Directive 1899 (Directive). The undersigned organizations urge the Secretary to amend Directive 1899 as it relates to allowing non-physician healthcare professionals in 32 specialties to operate “within the full scope of their license, registration, or certification” and rescind the Memorandum as it relates to encouraging all VA medical facilities to allow CRNAs to practice without physician oversight during the national health emergency. The undersigned organizations are very concerned Directive 1899 preempts state scope of practice laws. Directive 1899 memorializes U.S. Department of Veterans Affairs (VA) policy allowing VA health care professionals to practice across state lines and establishes new policy allowing VA health care professionals to operate within the full scope of their license, registration, or certification. This combination in effect circumvents state scope of practice laws for the 32 health care professionals defined in the directive. Such a far-reaching expansion is overly broad, unnecessary and threatens the health and safety of patients within the VA system. As state scope of practice laws vary across these professions and across states, we urge the Secretary to amend the directive to defer to state scope of practice laws, similar to the language related to psychologists in Appendix B of the Directive. -

July 22, 2020 the Honorable Seema Verma Administrator Centers For
July 22, 2020 The Honorable Seema Verma Administrator Centers for Medicare & Medicaid Services U.S. Department of Health and Human Services Hubert H. Humphrey Building, Room 445-G 200 Independence Avenue, SW Washington, DC 20201 Dear Administrator Verma: The undersigned organizations represent the hundreds of thousands of physicians who provide care for our nation’s Medicare patients every day. We are writing to strongly support the Centers for Medicare & Medicaid Services (CMS) decision to temporarily waive certain regulatory requirements during the COVID-19 pandemic. These temporary waivers, in extraordinary circumstances, have empowered physicians and non-physician health care professionals to focus on their patients and prevented a collapse of the health care system in the hardest hit areas of the country. However, we urge CMS to sunset the waivers involving scope of practice and licensure when the public health emergency (PHE) concludes. To our dismay, it is our understanding that some organizations have already been advocating to make the temporary waivers permanent—permanently diminishing physician oversight and supervision of patient care. While we are greatly appreciative of CMS’ rapid and substantial removal of regulatory barriers to allow physicians to continue providing care during the PHE, we also strive to continue to work with CMS to support patient access to physician-led care teams during and after the PHE. Throughout the coronavirus pandemic, physicians, nurses, and the entire health care community have been working side-by-side caring for patients and saving lives. Now more than ever, we need health care professionals working together as part of physician-led health care teams. -

ACCME Recognized State and Territory Medical Society Accreditors
ACCME Recognized State and Territory Medical Society Accreditors Medical Association of the State of Alabama Kansas Medical Society 19 South Jackson Street 623 S.W. 10th Ave. Montgomery, AL 36104-5144 Topeka, KS 66612 334-954-2500 785-235-2383 Arizona Medical Association Kentucky Medical Association 2401 West Peoria Avenue, Suite 130 9300 Shelbyville Road, Ste 850 Phoenix, AZ 85029-4790 Louisville, KY 40222-6301 602-347-6900 502-426-6200 California Medical Association Louisiana State Medical Society 1201 K Street, Suite #800 6767 Perkins Rd., Suite 100 Sacramento, CA 95814 Baton Rouge, LA 70808 800-786-4262 225-763-8500 Colorado Medical Society Maine Medical Association 7351 Lowry Blvd., Suite 110 Frank O. Stred Building Denver, CO 80230 30 Association Drive 720-859-1001 P.O. Box 190 Manchester, ME 04351 Florida Medical Association 207-622-3374 1430 Piedmont Drive East Tallahassee, FL 32308 MEDCHI, Maryland State Medical Society 850-224-6496 1211 Cathedral Street Baltimore, MD 21201 Medical Association of Georgia 410-539-0872 x 3307 1849 The Exchange, Suite 200 Atlanta, GA 30339 Massachusetts Medical Society 678-303-9290 860 Winter Street Waltham, MA 02451-1411 Hawaii Medical Association 781-434-7302 1360 S. Beretania St., Suite 200 Honolulu, HI 96814 Michigan State Medical Society 808-692-0900 120 West Saginaw P.O. Box 950 Illinois State Medical Society East Lansing, MI 48823 20 North Michigan Avenue, Suite 700 517-337-1351 Chicago, IL 60602 312-782-1654 x 4746 Minnesota Medical Association 1300 Godward Street NE, Suite 2500 Indiana State Medical Association Minneapolis, MN 55413 322 Canal Walk 612-362-3744 Indianapolis, IN 46202-3268 317-261-2060 Mississippi State Medical Association Iowa Medical Society 408 West Parkway Place 515 E. -
March 25, 2015 the Honorable John A
March 25, 2015 The Honorable John A. Boehner The Honorable Mitch McConnell Speaker Majority Leader U.S. House of Representatives United States Senate H-232 U.S. Capitol S-230 U.S. Capitol Washington, DC 20515 Washington, DC 20510 The Honorable Nancy Pelosi The Honorable Harry Reid Democratic Leader Democratic Leader U.S. House of Representatives United States Senate H-204 U.S. Capitol S-221 U.S. Capitol Washington, DC 20515 Washington, DC 20510 Dear Speaker Boehner, Leader Pelosi, Majority Leader McConnell and Leader Reid: The American Medical Association and the undersigned state medical associations are pleased to offer our strong support for H.R. 2, the “Medicare Access and CHIP Reauthorization Act” (MACRA), and we urge all members of the House and Senate to support its immediate passage. This legislation represents years of bipartisan effort to eliminate the fatally flawed sustainable growth rate (SGR) formula and implement new payment and delivery models that will promote high-quality care while reducing costs. In addition to stabilizing the Medicare program for our nation’s seniors, MACRA takes a balanced approach to addressing the health care needs of children and low-income Americans while promoting the long-term sustainability of the Medicare program. We are encouraged by the bipartisan leadership and collaboration that produced this legislation, and urge all members of the House and Senate to support passage before the expiration of the current Medicare patch. Sincerely, American Medical Association Medical Association of the -
U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420
July 29, 2021 The Honorable Denis McDonough Secretary U.S. Department of Veterans Affairs 810 Vermont Avenue NW, Room 1063B Washington, DC 20420 Dear Secretary McDonough: The undersigned physician organizations have recently learned of the Department of Veterans Affairs (VA) Supremacy Project. We are writing to express our serious concerns with the VA’s efforts to develop National Standards of Practice for physicians and other health professionals that supersede state scope of practice and licensure laws. In particular, we are dismayed that the VA has not provided a transparent process by which public stakeholders are provided an adequate opportunity to review and provide meaningful input into the standards of practice. Furthermore, based on what we have learned about the VA’s approach to developing the standards of practice for 48 categories of health professionals, we believe the VA has failed to consider that these health professionals do not operate in isolation but rather as a team. Yet, the VA is creating and moving standards forward independent of one another. In order to provide the best care for our Veterans, the VA must engage in a systematic examination of how all these standards will fit together and affect the health professional team. The policies the VA is seeking to overhaul will have implications for standards of care beyond the VA. It is therefore vitally important that the VA initiate a meaningful process for the collection, dissemination, and inclusion of stakeholder input as early into the process as possible. As physicians, we want to ensure that our nation’s Veterans receive the best medical care possible, including care from physician-led teams which research has shown results in the highest quality of care for patients.1 We therefore urge the VA to reconsider its implementation of the National Standards of Practice.