Clinical Anatomy of the Neck Region
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross Anatomy
www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY www.BookOfLinks.com Notice Medicine is an ever-changing science. As new research and clinical experience broaden our knowledge, changes in treatment and drug therapy are required. The authors and the publisher of this work have checked with sources believed to be reliable in their efforts to provide information that is complete and generally in accord with the standards accepted at the time of publication. However, in view of the possibility of human error or changes in medical sciences, neither the authors nor the publisher nor any other party who has been involved in the preparation or publication of this work warrants that the information contained herein is in every respect accurate or complete, and they disclaim all responsibility for any errors or omissions or for the results obtained from use of the information contained in this work. Readers are encouraged to confirm the infor- mation contained herein with other sources. For example and in particular, readers are advised to check the product information sheet included in the package of each drug they plan to administer to be certain that the information contained in this work is accurate and that changes have not been made in the recommended dose or in the contraindications for administration. This recommendation is of particular importance in connection with new or infrequently used drugs. www.BookOfLinks.com THE BIG PICTURE GROSS ANATOMY David A. Morton, PhD Associate Professor Anatomy Director Department of Neurobiology and Anatomy University of Utah School of Medicine Salt Lake City, Utah K. Bo Foreman, PhD, PT Assistant Professor Anatomy Director University of Utah College of Health Salt Lake City, Utah Kurt H. -
Anatomical Overview
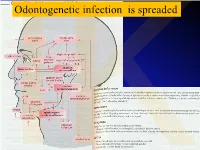
IKOdontogenetic infection is spreaded Možné projevy zlomenin a zánětů IKPossible signs of fractures or inflammations Submandibular space lies between the bellies of the digastric muscles, mandible, mylohyoid muscle and hyoglossus and styloglossus muscles IK IK IK IK IK Submandibulární absces Submandibular abscess IK Sběhlý submandibulární absces Submandibular abscess is getting down IK Submental space lies between the mylohyoid muscles and the investing layer of deep cervical fascia superficially IK IK Spatium peritonsillare IK IK Absces v peritonsilární krajině Abscess in peritonsilar region IK Fasciae Neck fasciae cervicales Demarcate spaces • fasciae – Superficial (investing): • f. nuchae, f. pectoralis, f. deltoidea • invests m. sternocleidomastoideus + trapezius • f. supra/infrahyoidea – pretrachealis (middle neck f.) • form Δ, invests infrahyoid mm. • vagina carotica (carotic sheet) – Prevertebral (deep cervical f.) • Covers scaleni mm. IK• Alar fascia Fascie Fascia cervicalis superficialis cervicales Fascia cervicalis media Fascia cervicalis profunda prevertebralis IKsuperficialis pretrachealis Neck spaces - extent • paravisceral space – Continuation of parafaryngeal space – Nervous and vascular neck bundle • retrovisceral space – Between oesophagus and prevertebral f. – Previsceral space – mezi l. pretrachealis a orgány – v. thyroidea inf./plx. thyroideus impar • Suprasternal space – Between spf. F. and pretracheal one IK– arcus venosus juguli 1 – sp. suprasternale suprasternal Spatia colli 2 – sp. pretracheale pretracheal 3 – -

Variant Origins of Arteries in the Carotid Triangle - a Case Report
Case Report 281 Variant Origins of Arteries in the Carotid Triangle - A Case Report B. V. Murlimanju, MD; Latha V. Prabhu, MS; Mangala M. Pai, MD; Dhanya Jayaprakash, MBBS; Vasudha V. Saralaya, MS The left superior laryngeal artery was observed arising from the external carotid artery instead of the superior thyroid artery in the cadaver of an approximately 70 year-old Asian man. In addition, on the same side, the superior thyroid artery arose from the common carotid artery 2 cm before the bifurcation instead of its usual origin from the external carotid artery. From the external carotid artery, the lingual and facial arteries arose from the com- mon linguofacial trunk. The nerves in the carotid triangle were normal in course. No varia- tions were observed on the right side carotid system. The multiple variations in this case have not been previously described. The embryogenesis of this combination of variations is not clear, but the anatomic consequences may have important clinical implications. As angiography has gained popularity in diagnostic approaches in recent years, it is essential to be aware of these variations so that they are not overlooked in differential diagnoses. (Chang Gung Med J 2012;35:281-4) Key words: artery, superior laryngeal, superior thyroid, common carotid, external carotid, vari- ant origin natomical variations in the carotid triangle in the STA from the left CCA is reported here. In the Athe neck are important, especially during surgi- literature, a few variations in origin have been cal and radiological intervention in the region. reported for both arteries,(1-3) but the combination of Normally, the superior laryngeal artery (SLA) is a variations reported in this case has not been previ- branch of the superior thyroid artery (STA). -
MSS 1. a Patient Presented to a Traumatologist with a Trauma Of
MSS 1. A patient presented to a traumatologist with a trauma of shoulder. What wall of axillary cavity contains foramen trilaterum and foramen quadrilaterum? a) anterior b) posterior c) lateral d) medial e) intermediate 2. A patient presented to a traumatologist with a trauma of leg, which he had sustained at a sport competition. Upon examination, damage of posterior muscle, that is attached to calcaneus by its tendon, was found. This muscle is: a) triceps surae b) tibialis posterior c) popliteus d) fibularis longus e) fibularis brevis 3. In the course of a cesarean section, an incision was made in the pubic area and vagina of rectus abdominis muscle was cut. What does anterior wall of the vagina of rectus abdominis muscle consist of? A. aponeurosis of m. transversus abdominis, m. obliquus internus abdominis. B. aponeurosis of m. transversus abdominis, m. pyramidalis. C. aponeurosis of m. obliquus internus abdominis, m. obliquus externus abdominis. D. aponeurosis of m. transversus abdominis, m. obliquus externus abdominis. E. aponeurosis of m. transversus abdominis, m. obliquus internus abdominis 4. A 30 year-old woman complained of pain in the lower part of her forearm. Traumatologist found that her radio-carpal joint was damaged. This joint is: A. complex, ellipsoid B.simple, ellipsoid C.complex, cylindrical D.simple, cylindrical E.complex condylar 5. A woman was brought by an ambulance to the emergency department with a trauma of the cervical part of her vertebral column. Radiologist diagnosed a fracture of a nonbifid spinous processes of one of her cervical vertebrae. Spinous process of what cervical vertebra is fractured? A.VI. -

DEPARTMENT of ANATOMY IGMC SHIMLA Competency Based Under
DEPARTMENT OF ANATOMY IGMC SHIMLA Competency Based Under Graduate Curriculum - 2019 Number COMPETENCY Objective The student should be able to At the end of the session student should know AN1.1 Demonstrate normal anatomical position, various a) Define and demonstrate various positions and planes planes, relation, comparison, laterality & b) Anatomical terms used for lower trunk, limbs, joint movement in our body movements, bony features, blood vessels, nerves, fascia, muscles and clinical anatomy AN1.2 Describe composition of bone and bone marrow a) Various classifications of bones b) Structure of bone AN2.1 Describe parts, blood and nerve supply of a long bone a) Parts of young bone b) Types of epiphysis c) Blood supply of bone d) Nerve supply of bone AN2.2 Enumerate laws of ossification a) Development and ossification of bones with laws of ossification b) Medico legal and anthropological aspects of bones AN2.3 Enumerate special features of a sesamoid bone a) Enumerate various sesamoid bones with their features and functions AN2.4 Describe various types of cartilage with its structure & a) Differences between bones and cartilage distribution in body b) Characteristics features of cartilage c) Types of cartilage and their distribution in body AN2.5 Describe various joints with subtypes and examples a) Various classification of joints b) Features and different types of fibrous joints with examples c) Features of primary and secondary cartilaginous joints d) Different types of synovial joints e) Structure and function of typical synovial -

Parts of the Body 1) Head – Caput, Capitus 2) Skull- Cranium Cephalic- Toward the Skull Caudal- Toward the Tail Rostral- Toward the Nose 3) Collum (Pl
BIO 3330 Advanced Human Cadaver Anatomy Instructor: Dr. Jeff Simpson Department of Biology Metropolitan State College of Denver 1 PARTS OF THE BODY 1) HEAD – CAPUT, CAPITUS 2) SKULL- CRANIUM CEPHALIC- TOWARD THE SKULL CAUDAL- TOWARD THE TAIL ROSTRAL- TOWARD THE NOSE 3) COLLUM (PL. COLLI), CERVIX 4) TRUNK- THORAX, CHEST 5) ABDOMEN- AREA BETWEEN THE DIAPHRAGM AND THE HIP BONES 6) PELVIS- AREA BETWEEN OS COXAS EXTREMITIES -UPPER 1) SHOULDER GIRDLE - SCAPULA, CLAVICLE 2) BRACHIUM - ARM 3) ANTEBRACHIUM -FOREARM 4) CUBITAL FOSSA 6) METACARPALS 7) PHALANGES 2 Lower Extremities Pelvis Os Coxae (2) Inominant Bones Sacrum Coccyx Terms of Position and Direction Anatomical Position Body Erect, head, eyes and toes facing forward. Limbs at side, palms facing forward Anterior-ventral Posterior-dorsal Superficial Deep Internal/external Vertical & horizontal- refer to the body in the standing position Lateral/ medial Superior/inferior Ipsilateral Contralateral Planes of the Body Median-cuts the body into left and right halves Sagittal- parallel to median Frontal (Coronal)- divides the body into front and back halves 3 Horizontal(transverse)- cuts the body into upper and lower portions Positions of the Body Proximal Distal Limbs Radial Ulnar Tibial Fibular Foot Dorsum Plantar Hallicus HAND Dorsum- back of hand Palmar (volar)- palm side Pollicus Index finger Middle finger Ring finger Pinky finger TERMS OF MOVEMENT 1) FLEXION: DECREASE ANGLE BETWEEN TWO BONES OF A JOINT 2) EXTENSION: INCREASE ANGLE BETWEEN TWO BONES OF A JOINT 3) ADDUCTION: TOWARDS MIDLINE -

432 Surgery Team Leaders
3 Common Neck Swellings Done By: Reviewed By: Othman.T.AlMutairi Ghadah Alharbi COLOR GUIDE: • Females' Notes • Males' Notes • Important • Additional Outlines Common Anatomy of the Neck Neck Ranula Swellings Dermoid cyst Thyroglossal cyst Branchial cysts Laryngocele Carotid body tumor Hemangioma Cystic Hygroma Inflammatory lymphadenopathy Malignant lymphadenopathy Thyroid related abnormalities Submandibular gland related abnormalities Sjogren's syndrome 1 Anatomy of the Neck: Quadrangular area (1): A quadrangular area can be delineated on the side of the neck. This area is subdivided by an obliquely prominent sternocleidomastoid muscle into anterior and posterior cervical triangles. Anterior cervical triangle is subdivided into four smaller triangles: -Submandibular triangle: Contains the submandibular salivary gland, hypoglossal nerve, mylohyiod muscle, and facial nerve. -Carotid triangle: Contains the carotid arteries and branches, internal jugular vein, and vagus nerve. -Omotracheal triangle: Includes the infrahyoid musculature and thyroid glands with the parathyroid glands. -Submental triangle: Beneath the chin. Figure 1: Anterior cervical muscles. 2 Posterior cervical triangle: The inferior belly of the omohyoid divides it into two triangles: -Occipital triangle: The contents include the accessory nerve, supraclavicular nerves, and upper brachial plexus. -Subclavian triangle: The contents include the supraclavicular nerves, Subclavian vessels, brachial plexus, suprascapular vessels, transverse cervical vessels, external jugular vein, and the nerve to the Subclavian muscle. The main arteries in the neck are the common carotids arising differently, one on each side. On the right, the common carotid arises at the bifurcation of the brachiocephalic trunk behind the sternoclavicular joint; on the left, it arises from the highest point on arch of the aorta in the chest. -

Ana Tomical Triangles J
43 ANA TOMICAL TRIANGLES J. LESLIE PACE, M.D. Department of Anatomy, Royal University of Malta Anatomical description is given of certain areas in the human hody which have :.l triangular sha!)e and which are of anatomical or surgical importance. There are at lea;,t 30 describe,d ,anatomical triangles, many of which receive eponymous names. Some are of nUlrked importance and well known e.g. Scarpa's femoral triangle, Hesselbach's inguinal triangle, H!ld Petit '5 lumbar triangle; others arc of relative1y minor importance and n.ot so well-known e.g. Elau's, Friteau's and Assezat's triangles. Anatomical trianlfles are described in various regions .of the body e.g. Macewen's ana Trautmann's in the head regiml, Beclaud's and PirDgoff's in the neck region, He'lSelbach '5, Henke '5, Petit's amI Grynfeltt's in the ,abdominal wall region and Searpa's Hnd Weber's in the lower limb Tf~gion. Their size varies, some being large e.g. Scarpa's triangle, others being very small e.g. Macewen's triangle. The bDundaries of these triangular areas may cDnsist of muscle borders e.g. the triangle .of Lannier and the variDUS tria,ngles of the neck; of n111sc1e borders and· bony cn1"fac(1,~ e.g. P(~lit'.~l tri,f)ng]c, t]1(' tria11['1]" ,C)f M'll"('ille J;lIlfl t1H~ tl"i[J11~le of Auscultation; of muscle borders and blood ves,ds e.g. Uesselbach's; of imaginary line, clrawn hetween fixed bony points e.g. -

Ministry of Education and Science of Ukraine Sumy State University 0
Ministry of Education and Science of Ukraine Sumy State University 0 Ministry of Education and Science of Ukraine Sumy State University SPLANCHNOLOGY, CARDIOVASCULAR AND IMMUNE SYSTEMS STUDY GUIDE Recommended by the Academic Council of Sumy State University Sumy Sumy State University 2016 1 УДК 611.1/.6+612.1+612.017.1](072) ББК 28.863.5я73 С72 Composite authors: V. I. Bumeister, Doctor of Biological Sciences, Professor; L. G. Sulim, Senior Lecturer; O. O. Prykhodko, Candidate of Medical Sciences, Assistant; O. S. Yarmolenko, Candidate of Medical Sciences, Assistant Reviewers: I. L. Kolisnyk – Associate Professor Ph. D., Kharkiv National Medical University; M. V. Pogorelov – Doctor of Medical Sciences, Sumy State University Recommended for publication by Academic Council of Sumy State University as а study guide (minutes № 5 of 10.11.2016) Splanchnology Cardiovascular and Immune Systems : study guide / С72 V. I. Bumeister, L. G. Sulim, O. O. Prykhodko, O. S. Yarmolenko. – Sumy : Sumy State University, 2016. – 253 p. This manual is intended for the students of medical higher educational institutions of IV accreditation level who study Human Anatomy in the English language. Посібник рекомендований для студентів вищих медичних навчальних закладів IV рівня акредитації, які вивчають анатомію людини англійською мовою. УДК 611.1/.6+612.1+612.017.1](072) ББК 28.863.5я73 © Bumeister V. I., Sulim L G., Prykhodko О. O., Yarmolenko O. S., 2016 © Sumy State University, 2016 2 Hippocratic Oath «Ὄμνυμι Ἀπόλλωνα ἰητρὸν, καὶ Ἀσκληπιὸν, καὶ Ὑγείαν, καὶ Πανάκειαν, καὶ θεοὺς πάντας τε καὶ πάσας, ἵστορας ποιεύμενος, ἐπιτελέα ποιήσειν κατὰ δύναμιν καὶ κρίσιν ἐμὴν ὅρκον τόνδε καὶ ξυγγραφὴν τήνδε. -

Neck Formation and Growth. MAIN TOPOGRAPHIC REGIONS in NECK
Neck formation and growth. MAIN TOPOGRAPHIC REGIONS IN NECK. ANATOMICAL BACKGROUND FOR URGENT LIFE SAVING PERFORMANCES. orofac Ivo Klepáček orofac Vymezení oblasti krku Extent of the neck region Sensitivní oblasti V1, V2, V3., plexus cervicalis orofac * * * * * orofac** * orofac orofac orofaccranial middle caudal orofac orofac Clinical classification of neck lymph nodes orofacClinical classification of neck lymphatic nodes: I - VI Nodi lymphatici out of regiones above: Perifacial, periparotic, retroauricular, suboccipital, retropharyngeal Metastasa v krčních uzlinách Metastasis in cervical orofaclymphonodi TOPOGRAPHIC REGIONS orofacand SPACES Regio colli anterior anterior neck triangle Trigonae : submentale, submandibulare, caroticum (musculare), regio suprasternalis Triangles : submental, submandibular, carotic (muscular), orofacsuprasternal region podkožní sval na povrchové krční fascii r. colli nervi facialis ovládá napětí kůže krku Platysma orofac proc. mastoideus manubrium sterni, clavicula Sternocleidomastoid m. n.accessorius (XI) + branches sternocleidomastoideus from plexus cervicalis orofac Punctum nervosum (Erb ´s point) : there C5 and C6 nerves are connected, + branches from suprascapulari and subclavian nerves orofacWilhelm Heinrich Erb (1840 - 1921), German neurologist orofac orofac mm. suprahyoid suprahyoidei and et mm. infrahyoid orofacinfrahyoidei muscles orofac Thyroid gland and vascular + nerve bundle in neck orofac orofac Žíly veins orofac štítná žláza příštitné orofactělísko a. thyroidea inferior n. laryngeus inferior -

Surface Anatomy
BODY ORIENTATION OUTLINE 13.1 A Regional Approach to Surface Anatomy 398 13.2 Head Region 398 13.2a Cranium 399 13 13.2b Face 399 13.3 Neck Region 399 13.4 Trunk Region 401 13.4a Thorax 401 Surface 13.4b Abdominopelvic Region 403 13.4c Back 404 13.5 Shoulder and Upper Limb Region 405 13.5a Shoulder 405 Anatomy 13.5b Axilla 405 13.5c Arm 405 13.5d Forearm 406 13.5e Hand 406 13.6 Lower Limb Region 408 13.6a Gluteal Region 408 13.6b Thigh 408 13.6c Leg 409 13.6d Foot 411 MODULE 1: BODY ORIENTATION mck78097_ch13_397-414.indd 397 2/14/11 3:28 PM 398 Chapter Thirteen Surface Anatomy magine this scenario: An unconscious patient has been brought Health-care professionals rely on four techniques when I to the emergency room. Although the patient cannot tell the ER examining surface anatomy. Using visual inspection, they directly physician what is wrong or “where it hurts,” the doctor can assess observe the structure and markings of surface features. Through some of the injuries by observing surface anatomy, including: palpation (pal-pā sh ́ ŭ n) (feeling with firm pressure or perceiving by the sense of touch), they precisely locate and identify anatomic ■ Locating pulse points to determine the patient’s heart rate and features under the skin. Using percussion (per-kush ̆ ́ŭn), they tap pulse strength firmly on specific body sites to detect resonating vibrations. And ■ Palpating the bones under the skin to determine if a via auscultation (aws-ku ̆l-tā sh ́ un), ̆ they listen to sounds emitted fracture has occurred from organs. -

On the Further History of Five Cases of Arterio-Venous Aneurysm of the Neck, with Some Remarks on the Condition Generally, and Its Treatment
J R Army Med Corps: first published as 10.1136/jramc-04-06-03 on 1 June 1905. Downloaded from ,41 ON THE FURTHER HISTORY OF FIVE CASES OF ARTERIO-VENOUS ANEURYSM OF THE NECK, WITH SOME REMARKS ON THE CONDITION GENERALLY, AND ITS TREATMENT. By G. H. MAKINS, C.B., F.R.C.S., Surgeon to St. Thomas'8 Hospital, &,c. THE cases upon which this communication are founded have already been published in my book on the ,. Surgery of the South African Campaign," but during the period of five years which has elapsed since, they were first under treatment changes have occurred in their condition which seem to render their history worthy of continuation. In again bringing them forward I take the opportunity of raising Protected by copyright. some questions with regard to arterio-venous communications ID general. (1) CAROTID ARTERIO-VENOUS ANEURYSM. The bullet (Mauser) entered at the right side of the pomum adami, and crossing' the larynx and the course of the left caI;otid vessels, emerged at the anterior border of the left trapezius two inches below the angle of the mandible. Immediate hffimorrhage occurred from the exit wound, but ceased spontaneously. At the end of some four hours, during which the patient had been removed 'to a field hospital, the bleeding recurred, and an incision was made http://militaryhealth.bmj.com/ by the surgeon-in-charge with the intention of ligaturing the carotid artery. During the preliminary stage of the operation, however, the bleeding ceased, and the vessel was not exposed nor ligatured. The patient was kept quiet for three weeks and then sent to the Base Hospital at Wynberg.