Influence of LPS, TNF, TGF-ß1 and IL-4 on the Expression of Mmps, Timps and Selected Cytokines in Rat Synovial Membranes Incubated in Vitro
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Single-Cell Transcriptional Atlas Identifies Extensive Heterogeneity in the Cellular Composition of Tendons
bioRxiv preprint doi: https://doi.org/10.1101/801266; this version posted October 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. A single-cell transcriptional atlas identifies extensive heterogeneity in the cellular composition of tendons Jacob B Swanson1, Andrea J De Micheli2, Nathaniel P Disser1, Leandro M Martinez1, Nicholas R Walker1,3, Benjamin D Cosgrove2, Christopher L Mendias1,3,* 1Hospital for Special Surgery, New York, NY, USA 2Meining School of Biomedical Engineering, Cornell University, Ithaca, NY, USA 3Department of Physiology and Biophysics, Weill Cornell Medical College, New York, NY, USA *Corresponding Author Christopher Mendias, PhD Hospital for Special Surgery 535 E 70th St New York, NY 10021 USA +1 212-606-1785 [email protected] Keywords: tenocyte; tendon fibroblast; pericyte; single-cell RNA sequencing bioRxiv preprint doi: https://doi.org/10.1101/801266; this version posted October 10, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Abstract Tendon is a dense, hypocellular connective tissue that transmits forces between muscles and bones. Cellular heterogeneity is increasingly recognized as an important factor in the biological basis of tissue homeostasis and disease, but little is known about the diversity of cells that populate tendon. Our objective was to explore the heterogeneity of cells in mouse Achilles tendons using single-cell RNA sequencing. We identified 13 unique cell types in tendons, including 4 previously undescribed populations of fibroblasts. -

Chromosomal Aberrations in Head and Neck Squamous Cell Carcinomas in Norwegian and Sudanese Populations by Array Comparative Genomic Hybridization
825-843 12/9/08 15:31 Page 825 ONCOLOGY REPORTS 20: 825-843, 2008 825 Chromosomal aberrations in head and neck squamous cell carcinomas in Norwegian and Sudanese populations by array comparative genomic hybridization ERIC ROMAN1,2, LEONARDO A. MEZA-ZEPEDA3, STINE H. KRESSE3, OLA MYKLEBOST3,4, ENDRE N. VASSTRAND2 and SALAH O. IBRAHIM1,2 1Department of Biomedicine, Faculty of Medicine and Dentistry, University of Bergen, Jonas Lies vei 91; 2Department of Oral Sciences - Periodontology, Faculty of Medicine and Dentistry, University of Bergen, Årstadveien 17, 5009 Bergen; 3Department of Tumor Biology, Institute for Cancer Research, Rikshospitalet-Radiumhospitalet Medical Center, Montebello, 0310 Oslo; 4Department of Molecular Biosciences, University of Oslo, Blindernveien 31, 0371 Oslo, Norway Received January 30, 2008; Accepted April 29, 2008 DOI: 10.3892/or_00000080 Abstract. We used microarray-based comparative genomic logical parameters showed little correlation, suggesting an hybridization to explore genome-wide profiles of chromosomal occurrence of gains/losses regardless of ethnic differences and aberrations in 26 samples of head and neck cancers compared clinicopathological status between the patients from the two to their pair-wise normal controls. The samples were obtained countries. Our findings indicate the existence of common from Sudanese (n=11) and Norwegian (n=15) patients. The gene-specific amplifications/deletions in these tumors, findings were correlated with clinicopathological variables. regardless of the source of the samples or attributed We identified the amplification of 41 common chromosomal carcinogenic risk factors. regions (harboring 149 candidate genes) and the deletion of 22 (28 candidate genes). Predominant chromosomal alterations Introduction that were observed included high-level amplification at 1q21 (harboring the S100A gene family) and 11q22 (including Head and neck squamous cell carcinoma (HNSCC), including several MMP family members). -

Negative Regulation of TIMP1 Is Mediated by Transcription Factor TWIST1
181-186.qxd 29/5/2009 01:25 ÌÌ ™ÂÏ›‰·181 INTERNATIONAL JOURNAL OF ONCOLOGY 35: 181-186, 2009 181 Negative regulation of TIMP1 is mediated by transcription factor TWIST1 HIROHIKO OKAMURA1, KAYA YOSHIDA2 and TATSUJI HANEJI1 Departments of 1Histology and Oral Histology and 2Fundamental Oral Health Science, Institute of Health Biosciences, The University of Tokushima Graduate School, Kuramoto, Tokushima 770-8504, Japan Received January 13, 2009; Accepted March 27, 2009 DOI: 10.3892/ijo_00000327 Abstract. TWIST1 is involved in tumor invasion and meta- process was mediated through suppression of the ARF/ stasis by promoting epithelial-to-mesenchymal transition. MDM2/p53 pathway (6). It was also reported that amplification However, the molecular target of TWIST1 involving this of Twist1 gene was associated with the development of mechanism is poorly understood. To identify the TWIST1- acquired resistance to anticancer drugs and ectopic expression regulated genes, we established the Saos-2 cells stably of Twist1 gene leads to resistance to microtubule disrupting expressing TWIST1 gene by transfecting TWIST1 cDNA into agents (7). TWIST1 is shown to affect AKT to mediate taxol the cells and performed a differential display approach by resistance in nasopharyngeal carcinoma cells and up- using annealing control primers. Here, we report that one of regulation of AKT2 by TWIST1 promoted cell survival, the genes that were down-regulated in TWIST1 expressing migration and invasion in breast cancer cells (8,9). The cells is predicted to be TIMP1. TIMP1 has been reported as increased expression of TWIST1 has been commonly used as the naturally occurring specific inhibitor of matrix metallo- molecular marker for EMT (10). -

The Diverse Roles of TIMP-3: Insights Into Degenerative Diseases of the Senescent Retina and Brain
cells Review The Diverse Roles of TIMP-3: Insights into Degenerative Diseases of the Senescent Retina and Brain Jennifer M. Dewing 1, Roxana O. Carare 1, Andrew J. Lotery 1,2 and J. Arjuna Ratnayaka 1,* 1 Clinical and Experimental Sciences, Faculty of Medicine, University of Southampton, MP806, Tremona Road, Southampton SO16 6YD, UK; [email protected] (J.M.D.); [email protected] (R.O.C.); [email protected] (A.J.L.) 2 Eye Unit, University Hospital Southampton NHS Foundation Trust, Southampton SO16 6YD, UK * Correspondence: [email protected]; Tel.: +44-238120-8183 Received: 13 November 2019; Accepted: 19 December 2019; Published: 21 December 2019 Abstract: Tissue inhibitor of metalloproteinase-3 (TIMP-3) is a component of the extracellular environment, where it mediates diverse processes including matrix regulation/turnover, inflammation and angiogenesis. Rare TIMP-3 risk alleles and mutations are directly linked with retinopathies such as age-related macular degeneration (AMD) and Sorsby fundus dystrophy, and potentially, through indirect mechanisms, with Alzheimer’s disease. Insights into TIMP-3 activities may be gleaned from studying Sorsby-linked mutations. However, recent findings do not fully support the prevailing hypothesis that a gain of function through the dimerisation of mutated TIMP-3 is responsible for retinopathy. Findings from Alzheimer’s patients suggest a hitherto poorly studied relationship between TIMP-3 and the Alzheimer’s-linked amyloid-beta (Aβ) proteins that warrant further scrutiny. This may also have implications for understanding AMD as aged/diseased retinae contain high levels of Aβ. Findings from TIMP-3 knockout and mutant knock-in mice have not led to new treatments, particularly as the latter does not satisfactorily recapitulate the Sorsby phenotype. -

Suramin Inhibits Osteoarthritic Cartilage Degradation by Increasing Extracellular Levels
Molecular Pharmacology Fast Forward. Published on August 10, 2017 as DOI: 10.1124/mol.117.109397 This article has not been copyedited and formatted. The final version may differ from this version. MOL #109397 Suramin inhibits osteoarthritic cartilage degradation by increasing extracellular levels of chondroprotective tissue inhibitor of metalloproteinases 3 (TIMP-3). Anastasios Chanalaris, Christine Doherty, Brian D. Marsden, Gabriel Bambridge, Stephen P. Wren, Hideaki Nagase, Linda Troeberg Arthritis Research UK Centre for Osteoarthritis Pathogenesis, Kennedy Institute of Downloaded from Rheumatology, University of Oxford, Roosevelt Drive, Headington, Oxford OX3 7FY, UK (A.C., C.D., G.B., H.N., L.T.); Alzheimer’s Research UK Oxford Drug Discovery Institute, University of Oxford, Oxford, OX3 7FZ, UK (S.P.W.); Structural Genomics Consortium, molpharm.aspetjournals.org University of Oxford, Old Road Campus Research Building, Old Road Campus, Roosevelt Drive, Headington, Oxford, OX3 7DQ (BDM). at ASPET Journals on September 29, 2021 1 Molecular Pharmacology Fast Forward. Published on August 10, 2017 as DOI: 10.1124/mol.117.109397 This article has not been copyedited and formatted. The final version may differ from this version. MOL #109397 Running title: Repurposing suramin to inhibit osteoarthritic cartilage loss. Corresponding author: Linda Troeberg Address: Kennedy Institute of Rheumatology, University of Oxford, Roosevelt Drive, Headington, Oxford OX3 7FY, UK Phone number: +44 (0)1865 612600 E-mail: [email protected] Downloaded -

Investigation of COVID-19 Comorbidities Reveals Genes and Pathways Coincident with the SARS-Cov-2 Viral Disease
bioRxiv preprint doi: https://doi.org/10.1101/2020.09.21.306720; this version posted September 21, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Title: Investigation of COVID-19 comorbidities reveals genes and pathways coincident with the SARS-CoV-2 viral disease. Authors: Mary E. Dolan1*,2, David P. Hill1,2, Gaurab Mukherjee2, Monica S. McAndrews2, Elissa J. Chesler2, Judith A. Blake2 1 These authors contributed equally and should be considered co-first authors * Corresponding author [email protected] 2 The Jackson Laboratory, 600 Main St, Bar Harbor, ME 04609, USA Abstract: The emergence of the SARS-CoV-2 virus and subsequent COVID-19 pandemic initiated intense research into the mechanisms of action for this virus. It was quickly noted that COVID-19 presents more seriously in conjunction with other human disease conditions such as hypertension, diabetes, and lung diseases. We conducted a bioinformatics analysis of COVID-19 comorbidity-associated gene sets, identifying genes and pathways shared among the comorbidities, and evaluated current knowledge about these genes and pathways as related to current information about SARS-CoV-2 infection. We performed our analysis using GeneWeaver (GW), Reactome, and several biomedical ontologies to represent and compare common COVID- 19 comorbidities. Phenotypic analysis of shared genes revealed significant enrichment for immune system phenotypes and for cardiovascular-related phenotypes, which might point to alleles and phenotypes in mouse models that could be evaluated for clues to COVID-19 severity. -

Telomere-To-Telomere Assembly of a Complete Human X Chromosome W
https://doi.org/10.1038/s41586-020-2547-7 Accelerated Article Preview Telomere-to-telomere assembly of a W complete human X chromosome E VI Received: 30 July 2019 Karen H. Miga, Sergey Koren, Arang Rhie, Mitchell R. Vollger, Ariel Gershman, Andrey Bzikadze, Shelise Brooks, Edmund Howe, David Porubsky, GlennisE A. Logsdon, Accepted: 29 May 2020 Valerie A. Schneider, Tamara Potapova, Jonathan Wood, William Chow, Joel Armstrong, Accelerated Article Preview Published Jeanne Fredrickson, Evgenia Pak, Kristof Tigyi, Milinn Kremitzki,R Christopher Markovic, online 14 July 2020 Valerie Maduro, Amalia Dutra, Gerard G. Bouffard, Alexander M. Chang, Nancy F. Hansen, Amy B. Wilfert, Françoise Thibaud-Nissen, Anthony D. Schmitt,P Jon-Matthew Belton, Cite this article as: Miga, K. H. et al. Siddarth Selvaraj, Megan Y. Dennis, Daniela C. Soto, Ruta Sahasrabudhe, Gulhan Kaya, Telomere-to-telomere assembly of a com- Josh Quick, Nicholas J. Loman, Nadine Holmes, Matthew Loose, Urvashi Surti, plete human X chromosome. Nature Rosa ana Risques, Tina A. Graves Lindsay, RobertE Fulton, Ira Hall, Benedict Paten, https://doi.org/10.1038/s41586-020-2547-7 Kerstin Howe, Winston Timp, Alice Young, James C. Mullikin, Pavel A. Pevzner, (2020). Jennifer L. Gerton, Beth A. Sullivan, EvanL E. Eichler & Adam M. Phillippy C This is a PDF fle of a peer-reviewedI paper that has been accepted for publication. Although unedited, the Tcontent has been subjected to preliminary formatting. Nature is providing this early version of the typeset paper as a service to our authors and readers. The text andR fgures will undergo copyediting and a proof review before the paper is published in its fnal form. -

Identification of Gene Expression and DNA Methylation of SERPINA5 and TIMP1 As Novel Prognostic Markers in Lower-Grade Gliomas
Identification of gene expression and DNA methylation of SERPINA5 and TIMP1 as novel prognostic markers in lower-grade gliomas Wen-Jing Zeng1,2,3,4, Yong-Long Yang5, Zhi-Peng Wen1,2, Peng Chen1,2, Xiao-Ping Chen1,2 and Zhi-Cheng Gong3,4 1 Department of Clinical Pharmacology, Xiangya Hospital, Central South University, Changsha, Hunan, China 2 Institute of Clinical Pharmacology, Central South University, Hunan Key Laboratory of Pharmacogenetics, Changsha, Hunan, China 3 Department of Pharmacy, Xiangya Hospital, Central South University, Changsha, Hunan, China 4 National Clinical Research Center for Geriatric Disorders (XIANGYA), Xiangya Hospital, Central South University, Changsha, Hunan, China 5 Department of Clinical Pharmacology Research Center, Changsha Carnation Geriatrics Hospital, Changsha, Hunan, China ABSTRACT Background. Lower-grade gliomas (LGGs) is characteristic with great difference in prognosis. Due to limited prognostic biomarkers, it is urgent to identify more molecular markers to provide a more objective and accurate tumor classification system for LGGs. Methods. In the current study, we performed an integrated analysis of gene expression data and genome-wide methylation data to determine novel prognostic genes and methylation sites in LGGs. Results. To determine genes that differentially expressed between 44 short-term survivors (<2 years) and 48 long-term survivors (≥2 years), we searched LGGs TCGA RNA-seq dataset and identified 106 differentially expressed genes. SERPINA5 and Submitted 11 October 2019 Accepted 9 May 2020 TIMP1 were selected for further study. Kaplan–Meier plots showed that SERPINA5 Published 3 June 2020 and TIMP1 expression were significantly correlated with overall survival (OS) and Corresponding authors relapse-free survival (RFS) in TCGA LGGs patients. -

TIMP1 Polyclonal Antibody Gene Summary: This Gene Belongs to the TIMP Gene Family
TIMP1 polyclonal antibody Gene Summary: This gene belongs to the TIMP gene family. The proteins encoded by this gene family are Catalog Number: PAB19116 natural inhibitors of the matrix metalloproteinases (MMPs), a group of peptidases involved in degradation Regulatory Status: For research use only (RUO) of the extracellular matrix. In addition to its inhibitory role against most of the known MMPs, the encoded protein is Product Description: Rabbit polyclonal antibody raised able to promote cell proliferation in a wide range of cell against synthetic peptide of TIMP1. types, and may also have an anti-apoptotic function. Transcription of this gene is highly inducible in response Immunogen: A synthetic peptide corresponding to to many cytokines and hormones. In addition, the C-terminus of human TIMP1. expression from some but not all inactive X chromosomes suggests that this gene inactivation is Host: Rabbit polymorphic in human females. This gene is located Reactivity: Human within intron 6 of the synapsin I gene and is transcribed in the opposite direction. [provided by RefSeq] Applications: IHC-P, WB-Re (See our web site product page for detailed applications information) Protocols: See our web site at http://www.abnova.com/support/protocols.asp or product page for detailed protocols Form: Lyophilized Purification: Immunoaffinity purification Isotype: IgG Recommend Usage: Western Blot (1 ug/mL) Immunohistochemistry (Formalin/PFA-fixed paraffin-embedded sections) (1 ug/mL) The optimal working dilution should be determined by the end user. Storage Buffer: Lyophilized from 0.9 mg NaCl, 0.2 mg Na2HPO4 (5 mg BSA, 0.05 mg sodium azide, 0.05 mg Thimerosal) Storage Instruction: Store at -20°C on dry atmosphere. -
![Anti-TIMP1 Antibody [2A5] (ARG10543)](https://docslib.b-cdn.net/cover/3318/anti-timp1-antibody-2a5-arg10543-843318.webp)
Anti-TIMP1 Antibody [2A5] (ARG10543)
Product datasheet [email protected] ARG10543 Package: 100 μg anti-TIMP1 antibody [2A5] Store at: -20°C Summary Product Description Mouse Monoclonal antibody [2A5] recognizes TIMP1 Tested Reactivity Hu Tested Application IHC-P, WB Host Mouse Clonality Monoclonal Clone 2A5 Isotype IgG1, kappa Target Name TIMP1 Antigen Species Human Immunogen Ovalbumin-conjugated synthetic peptide. (FQALGDAADIR) Conjugation Un-conjugated Alternate Names Erythroid-potentiating activity; TIMP; Collagenase inhibitor; Fibroblast collagenase inhibitor; TIMP-1; EPO; CLGI; Tissue inhibitor of metalloproteinases 1; HCI; Metalloproteinase inhibitor 1; EPA Application Instructions Application table Application Dilution IHC-P 1:8 WB 1:5 Application Note IHC-P: Antigen Retrieval: Microwave for 7 min at 950W in 0.01 M Sodium citrate buffer (pH 6.0) * The dilutions indicate recommended starting dilutions and the optimal dilutions or concentrations should be determined by the scientist. Positive Control IHC: formalin-fixed, paraffin-embedded colonic adenocarcinoma. Western blot: rhTIMP-1, 400 ng per lane. Calculated Mw 23 kDa Properties Form Liquid Purification Affinity purification with immunogen. Buffer PBS and 0.02% Sodium azide Preservative 0.02% Sodium azide Storage instruction For continuous use, store undiluted antibody at 2-8°C for up to a week. For long-term storage, aliquot and store at -20°C or below. Storage in frost free freezers is not recommended. Avoid repeated freeze/thaw cycles. Suggest spin the vial prior to opening. The antibody solution should be gently mixed www.arigobio.com 1/3 before use. Note For laboratory research only, not for drug, diagnostic or other use. Bioinformation Database links GeneID: 7076 Human Swiss-port # P01033 Human Gene Symbol TIMP1 Gene Full Name TIMP metallopeptidase inhibitor 1 Background This gene belongs to the TIMP gene family. -
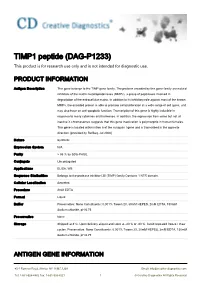
TIMP1 Peptide (DAG-P1233) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
TIMP1 peptide (DAG-P1233) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description This gene belongs to the TIMP gene family. The proteins encoded by this gene family are natural inhibitors of the matrix metalloproteinases (MMPs), a group of peptidases involved in degradation of the extracellular matrix. In addition to its inhibitory role against most of the known MMPs, the encoded protein is able to promote cell proliferation in a wide range of cell types, and may also have an anti-apoptotic function. Transcription of this gene is highly inducible in response to many cytokines and hormones. In addition, the expression from some but not all inactive X chromosomes suggests that this gene inactivation is polymorphic in human females. This gene is located within intron 6 of the synapsin I gene and is transcribed in the opposite direction. [provided by RefSeq, Jul 2008] Nature Synthetic Expression System N/A Purity > 95 % by SDS-PAGE. Conjugate Unconjugated Applications ELISA, WB Sequence Similarities Belongs to the protease inhibitor I35 (TIMP) family.Contains 1 NTR domain. Cellular Localization Secreted. Procedure 2mM EDTA Format Liquid Buffer Preservative: None Constituents: 0.001% Tween 20, 30mM HEPES, 2mM EDTA, 150mM Sodium chloride, pH 6.75 Preservative None Storage Shipped at 4°C. Upon delivery aliquot and store at -20°C or -80°C. Avoid repeated freeze / thaw cycles. Preservative: None Constituents: 0.001% Tween 20, 30mM HEPES, 2mM EDTA, 150mM Sodium chloride, pH 6.75 ANTIGEN -

Prognostic Significance of TIMP-1 in Non-Small Cell Lung Cancer
ANTICANCER RESEARCH 31: 4031-4038 (2011) Prognostic Significance of TIMP-1 in Non-small Cell Lung Cancer MARTIN PESTA1, VLASTIMIL KULDA2, RADEK KUCERA1, MILOS PESEK3, JINDRA VRZALOVA1, VACLAV LISKA4, LADISLAV PECEN1, VLADISLAV TRESKA4, JARMIL SAFRANEK4, MARKETA PRAZAKOVA1, ONDREJ VYCITAL4, JAN BRUHA4, LUBOS HOLUBEC5 and ONDREJ TOPOLCAN1 Departments of 1Internal Medicine II and 2Biochemistry, Faculty of Medicine in Pilsen, Charles University in Prague, Czech Republic; 3TRN Clinic, University Hospital and Medical Faculty in Pilsen, Czech Republic; Departments of 4Surgery and 5Oncology, University Teaching Hospital, Pilsen, Czech Republic Abstract. Tissue inhibitor of metalloproteinases 1 (TIMP1) the mortality 48.7/100 000 per year (1). Non-small cell lung regulates not only extracellular matrix catabolism but the cancer (NSCLC) accounts for 80% of all cases (2). major effect in tumor tissue is promotion of cell growth and Although there are tumor markers routinely used for solid anti-apoptotic activity. The aim of our study was to evaluate tumors, some of them having become gold standards (3), plasma TIMP1 levels and tissue TIMP1 mRNA expression as there is still an effort being made to search for new ones. prognostic markers in NSCLC patients. Patients and Tissue inhibitor of metalloproteinases 1 (TIMP1) has been Methods: We studied a group of 108 patients with NSCLC studied intensively over the last ten years and in colorectal who had undergone lung surgery. Estimation of TIMP1 cancer it seems to be promising as a prognostic marker in mRNA was performed by quantitative polymerase chain clinical use (4). A Danish-Australian endoscopy study group reaction (qPCR) and estimation of plasma TIMP1 protein on colorectal cancer detection is trying to use TIMP1 as a using enzyme-linked immunosorbent assay (ELISA).