Physical and Verbal Violence Against Health Care Workers
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Personality Traits As Risk Factors for Occupational Injury in Health Care Workers
PERSONALITY TRAITS AS RISK FACTORS FOR OCCUPATIONAL INJURY IN HEALTH CARE WORKERS By HILARY STEVENS MORGAN A DISSERTATION PRESENTED TO THE GRADUATE SCHOOL OF THE UNIVERSITY OF FLORIDA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF PHILOSOPHY UNIVERSITY OF FLORIDA 2007 1 © 2007 Hilary Stevens Morgan 2 To my parents who always stressed the value of education and instilled in their children a belief that anything was possible 3 ACKNOWLEDGMENTS I would like to thank my committee chair, Dr. Nancy Nivison Menzel, for her guidance, encouragement, and patience throughout this research study. I appreciate her knowledge of occupational health nursing and her commitment to provide leadership for this study despite moving over 2,000 miles westward. I gratefully acknowledge and extend my appreciation to the members of my committee, Jo Snider, PhD, Jiunn-Jye Sheu, PhD, and James V. Jessup, PhD. Each of them provided unique talents, time, and moral support during this study. I would like to thank Dr. Snider for her support during my struggles understanding psychology, Dr. Sheu for his patience in dealing with my epidemiology and study design questions and Dr. Jessup for his calm and encouragement in my moments of doubt. I also want to thank Seaborn Hunt, MD for his support of my returning to school. I know my absences in the office for school activities presented an additional burden on him, but he never wavered in his encouragement of my endeavors. The same appreciation is extended to Paula Murphy, Kathy Sandor, Ronnie Maxim, Vickie Hall, Milly Wilkinson and Renee' Brown who tolerated, with good graces, my vacillating moods throughout this long process. -

Injury Prevention in Day Laborers
Injury Prevention in Day Laborers: Job-specific Fact Sheets LauraLaura Cristal Cristal Magaña Magaña1,1 ,Noah Noah Seixas Seixas22,, PhD;PhD; JaniceJanice CampCamp2,MSN, MSPH, CIHCIH 1Oregon1Oregon State State University; University; 2 Dept2Dept of of Environmental Environmental andand OccupationalOccupational Health Sciences, University ofof WashingtonWashington Occupational Injury Prevention for Jornaleros Results Occupational Injury Prevention for JornalerosThe first set of factResults sheets were created on the following topics: PROBLEM: • HRI to target summerFact sheets jornalero were jobs created on the following topics: Jornaleros, orPROBLEM: day laborers, experience higher injury rates than the average • Maintenance and•Heat cleaning related topics, illness including: (HRI) to target summer jornalero jobs worker. DifferentJornaleros factors, or dayput laborersthem at , increasedexperience risk, higher including injury ratesdaily than the • Chemicals •Maintenance and cleaning topics, including: variation in employeraverage andworker. job, and Different minimal factors safety puttraining them. Casa at increased Latina (CL) risk, including • Lifting and carrying•Chemicals is a worker centerdaily invariation Seattle whichin employer supports and Latino job, jornalerosand minimal. safety training. Casa • Organic dust •Lifting and carrying Latina (CL) is a worker center in Seattle which supports Latino • Biological hazards •Organic dust SOLUTION: jornaleros. •Biological hazards Previously, surveysSOLUTION: conducted at CL found that -

"Employer's Report of Occupational Injury Or Illness" (Form 5020)
State of California Please complete in triplicate (type if possible) Mail two copies to: OSHA CASE NO. EMPLOYER'S REPORT OF OCCUPATIONAL INJURY OR ILLNESS FATALITY Any person who makes or causes to be made any California law requires employers to report within five days of knowledge every occupational injury or illness which results in lost time beyond the knowingly false or fraudulent material statement or date of the incident OR requires medical treatment beyond first aid. If an employee subsequently dies as a result of a previously reported injury or material representation for the purpose of obtaining or illness, the employer must file within five days of knowledge an amended report indicating death. In addition, every serious injury, illness, or death denying workers compensation benefits or payments is guilty of a felony. must be reported immediately by telephone or telegraph to the nearest office of the California Division of Occupational Safety and Health. 1. FIRM NAME Ia. Policy Number Please do not use this column 2. MAILING ADDRESS: (Number, Street, City, Zip) E 2a. Phone Number M CASE NUMBER P L 3. LOCATION if different from Mailing Address (Number, Street, City and Zip) 3a. Location Code O OWNERSHIP Y E 4. NATURE OF BUSINESS; e.g.. Painting contractor, wholesale grocer, sawmill, hotel, etc. 5. State unemployment insurance acct.no R 6. TYPE OF EMPLOYER: INDUSTRY Private State County City School District Other Gov't, Specify: 7. DATE OF INJURY / ONSET OF ILLNESS 8. TIME INJURY/ILLNESS OCCURRED 9. TIME EMPLOYEE BEGAN WORK 10. IF EMPLOYEE DIED, DATE OF DEATH (mm/dd/yy) (mm/dd/yy) AM PM AM PM OCCUPATION 1 1. -
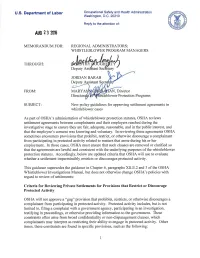
New Policy Guidelines for Approving Settlement Agreements in Whistleblower Cases
U.S. Department of Labor Occupational Safety and Health Administration Washington, D.C. 20210 Reply to the attention of: AUG 23 20\S MEMORANDUM FOR: REGIONAL ADMINISTRATORS; WHISTLEBLOWER PROGRAM MANAGERS THROUGH: ~~~~'¥/::lJ JORDAN BARAB ~ Y>~ ~eputy Assistant Secr(j-;f FROM: MARY A AN, Director us tleblower Protection Programs SUBJECT: New policy guidelines for approving settlement agreements in whistleblower cases As part of OSHA' s administration of whistle blower protection statutes, OSHA reviews settlement agreements between complainants and their employers reached during the investigative stage to ensure they are fair, adequate, reasonable, and in the public interest, and that the employee's consent was knowing and voluntary. In reviewing these agreements OSHA sometimes encounters provisions that prohibit, restrict, or otherwise discourage a complainant from participating in protected activity related to matters that arose during his or her employment. In those cases, OSHA must ensure that such clauses are removed or clarified so that the agreements are lawful and consistent with the underlying purposes of the whistle blower protection statutes. Accordingly, below are updated criteria that OSHA will use to evaluate whether a settlement impermissibly restricts or discourages protected activity. This guidance supersedes the guidance in Chapter 6, paragraphs XII.E.2 and 3 of the OSHA Whistleblower Investigations Manual, but does not otherwise change OSHA's policies with regard to review of settlements: Criteria for Reviewing Private Settlements for Provisions that Restrict or Discourage Protected Activity OSHA will not approve a "gag" provision that prohibits, restricts, or otherwise discourages a complainant from participating in protected activity. Protected activity includes, but is not limited to, filing a complaint with a government agency, participating in an investigation, testifying in proceedings, or otherwise providing information to the government. -

Introduction to Mobbing in the Workplace and an Overview of Adult Bullying
1: Introduction to Mobbing in the Workplace and an Overview of Adult Bullying Workplace Bullying Clinical and Organizational Perspectives In the early 1980s, German industrial psychologist Heinz Leymann began work in Sweden, conducting studies of workers who had experienced violence on the job. Leymann’s research originally consisted of longitudinal studies of subway drivers who had accidentally run over people with their trains and of banking employees who had been robbed on the job. In the course of his research, Leymann discovered a surprising syndrome in a group that had the most severe symptoms of acute stress disorder (ASD), workers whose colleagues had ganged up on them in the workplace (Gravois, 2006). Investigating this further, Leymann studied workers in one of the major Swedish iron and steel plants. From this early work, Leymann used the term “mobbing” to refer to emotional abuse at work by one or more others. Earlier theorists such as Austrian ethnologist Konrad Lorenz and Swedish physician Peter-Paul Heinemann used the term before Leymann, but Leymann received the most recognition for it. Lorenz used “mobbing” to describe animal group behavior, such as attacks by a group of smaller animals on a single larger animal (Lorenz, 1991, in Zapf & Leymann, 1996). Heinemann borrowed this term and used it to describe the destructive behavior of children, often in a group, against a single child. This text uses the terms “mobbing” and “bullying” interchangeably; however, mobbing more often refers to bullying by more than one person and can be more subtle. Bullying more often focuses on the actions of a single person. -

The Effects of Working Time on Productivity and Firm Performance: a Research Synthesis Paper
For information on the Conditions of Work and Employment Branch, please contact: Phone: (+41 22) 799 67 54 Fax: (+41 22) 799 84 51 [email protected] International Labour Office, The effects of working time Conditions of Work and Employment Branch on productivity and firm performance: 4, route des Morillons CH-1211 Geneva 22 a research synthesis paper Switzerland www.ilo.org/travail Lonnie Golden CONDITIONS OF WORK AND EMPLOYMENT SERIES No. 33 TRAVAIL ISSN 2226-8944 Conditions of Work and Employment Series No. 33 Conditions of Work and Employment Branch The Effects of Working Time on Productivity and Firm Performance: a research synthesis paper Prepared by Lonnie Golden1 Research synthesis paper initially prepared for the Tripartite Meeting of Experts on Working Time Arrangements (2011) INTERNATIONAL LABOUR OFFICE – GENEVA 1 Professor of Economics and Labor Studies, Penn State University, Abington College, [email protected]. Copyright © International Labour Organization 2012 First published 2012 Publications of the International Labour Office enjoy copyright under Protocol 2 of the Universal Copyright Convention. Nevertheless, short excerpts from them may be reproduced without authorization, on condition that the source is indicated. For rights of reproduction or translation, application should be made to ILO Publications (Rights and Permissions), International Labour Office, CH-1211 Geneva 22, Switzerland, or by email: [email protected]. The International Labour Office welcomes such applications. Libraries, institutions and other users registered with reproduction rights organizations may make copies in accordance with the licences issued to them for this purpose. Visit www.ifrro.org to find the reproduction rights organization in your country. ILO Cataloguing in Publication Data Golden, Lonnie The effects of working time on productivity and firm performance: a research synthesis paper/ prepared by Lonnie Golden ; International Labour Office, Conditions of Work and Employment Branch. -

Hawaii Administrative Rules
§12-52.1 HAWAII ADMINISTRATIVE RULES TITLE 12 DEPARTMENT OF LABOR AND INDUSTRIAL RELATIONS SUBTITLE 8 DIVISION OF OCCUPATIONAL SAFETY AND HEALTH PART 1 GENERAL, LEGAL, AND ADMINISTRATIVE PROVISIONS FOR OCCUPATIONAL SAFETY AND HEALTH CHAPTER 52.1 RECORDING AND REPORTING OCCUPATIONAL INJURIES AND ILLNESSES §12-52.1-1 State amendments to 29 CFR 1904 [Changes have been compiled.] §12-52.1-2 Incorporation to federal standard Historical note: Chapter 12-52.1 is based substantially upon chapter 12-52. [Eff 7/12/82; am 5/28/83; am 8/15/87; am 9/30/94; am 2/8/97; am 7/10/97; am 7/6/99; R 12/29/01] §12-52.1-2 Incorporation of federal standard. Title 29, Code of Federal Regulations, Part 1904, entitled “Occupational Injury and Illness Recording and Reporting Requirements” published by the Office of the Federal Register, National Archives and Records Administration on January 19, 2001; and the amendments published on October 12, 2001; July 1, 2002; December 17, 2002; and June 30, 2003, are made part of this chapter, except as provided in section 12-52.1-1. [Eff 12/29/01; am 1/10/03; am 5/21/04; am 5/5/05] (Auth: HRS §396-4) (Imp: HRS §396-4) 1 §12-52.1 SUBPART A -- PURPOSE §1904.0 Purpose. The purpose of this rule (Part 1904) is to require employers to record and report work- related fatalities, injuries and illnesses. Note to §1904.0: Recording or reporting a work-related injury, illness, or fatality does not mean that the employer or employee was at fault, that an OSHA rule has been violated, or that the employee is eligible for workers' compensation or other benefits. -

Construction-Related Presentations from the October, 2009 National Occupational Injury Research Symposium (Noirs)
NOIRS 2009 Construction Presentations and Posters CONSTRUCTION-RELATED PRESENTATIONS FROM THE OCTOBER, 2009 NATIONAL OCCUPATIONAL INJURY RESEARCH SYMPOSIUM (NOIRS) NOTE: See http://www.cdc.gov/niosh/noirs/2008/abstracts2008.html for full list of all abstracts NOTE: See http://www.cdc.gov/niosh/noirs/2008/participants2008.html for list of participants and contact information Session: A1.0 Title: Describing and Preventing Falls From Heights in Construction Moderator: Paul Becker A1.1 Title: Observation of Fall Risks in Residential Construction Sites Authors: Kaskutas V, Dale AM, Lipscomb H, Gaal J, Fuchs M, Nolan J, Patterson D, Evanoff B Introduction: Workers are exposed to many fall risks at residential construction sites. Methods to quantify these risks are needed. Methods: Two experienced journeymen carpenters used a 52-item validated observational audit to evaluate the fall prevention behaviors of unionized carpenters at residential construction sites in the St. Louis area. Collaboration with the local carpenters’ apprenticeship program, a joint union/contractor partnership, facilitated access to worksites. We computed the frequency of observations meeting the audit safety criteria. Results: Multiple stages of construction were assessed at 197 worksites representing small, medium, and large contractors. Ladders were observed at 72% of the sites; however, extension ladders were not secured 88% of the time and stepladders were used inappropriately 49% of the time. Carpenters stood and balanced on 3½-inch boards, one story in the air while installing floor joists and roof trusses 81% and 93% of the time, respectively. Unprotected walking surfaces were identified with a warning line 18% of the time, and controlled access zones met OSHA guidelines only 2% of the time. -

Assessing Occupational Safety and Health Training
Assessing Occupational Safety and Health Training A Literature Review Prepared by: Alexander Cohen, PhD Michael J. Colligan, PhD With Technical Assistance from: Raymond Sinclair Jerry Newman Ronald Schuler June 1998 Disclaimer Mention of company names or products does not constitute endorsement by the National Institute for Occupational Safety and Health (NIOSH), Centers for Disease Control and Prevention (CDC). This document is in the public domain and may be freely copied or reprinted. Copies of this and other NIOSH documents are available from the National Institute for Occupational Safety and Health Publications Dissemination 4676 Columbia Parkway Cincinnati, Ohio 45226-1998 To receive information on other occupational safety and health issues, call 1-800-35-NIOSH (1-800-356-4674), or visit NIOSH Home Page on the World Wide Web at http://www.cdc.gov/niosh Email: [email protected] DHHS (NIOSH) Publication No. 98-145 ii ■ Foreword Occupational safety and health training remains a fundamental element in workplace hazard control pro- grams. As training objectives, recognition of job hazards, learning safe work practices and appreciating other preventive measures are expected to contribute to the goal of reducing occupational risk of injury and disease. This report reviews data found in the literature reflecting the significance of training in meeting these kinds of objectives and outcomes. As will be seen, there is much positive evidence but the results seem very selective and highly qualified. An analysis to identify factors underlying a successful training experience is also presented and does confirm basic principles of learning. Here too, however, important gaps are noted in the available data. -

Unemployment and Workplace Safety: New Evidence on the Pro-Cyclicality of U.S
Essays in Health and Labor Economics by Matthew James Butler A dissertation submitted in partial satisfaction of the requirements of the degree of Doctor of Philosophy in Economics in the GRADUATE DIVISION of the UNIVERSITY OF CALIFORNIA, BERKELEY Committee in Charge: Professor Enrico Moretti, Chair Professor David Card Professor William Dow Fall 2011 Essays in Health and Labor Economics Copyright 2011 by Matthew James Butler Abstract Essays in Health and Labor Economics by Matthew James Butler Doctor of Philosophy in Economics University of California, Berkeley Professor Enrico Moretti, Chair This dissertation examines how occupational injuries vary with the business cycle, the relationship between healthcare staffing levels and patient outcomes, and whether workers are compensated for changes in occupational risk. In the first chapter I examine how fatal and non-fatal occupational injury rates vary over the business cycle. Past research on the relationship between workplace safety and the business cycle has found only non-fatal accidents to be pro-cyclical. The failure of previous research to convincingly identify a pro- cyclical fatality relationship has led researchers to focus on a claims reporting moral hazard explanation of the pro-cyclicality of non-fatal injuries. Using state and firm level workplace safety data and local area unemployment rates, I find that workplace safety is pro-cyclical in both fatal and non-fatal injury rates, contrary to previous research. The occupational fatality rate elasticity (-0.15) is larger in magnitude than its non-fatality counterpart (-0.10). The next chapter explores how a change in nurse staffing levels for intensive care patients improved patient outcomes in Arizona. -

Federal Register / Vol. 61, No. 23 / Friday, February 2, 1996 / Proposed Rules
4030 Federal Register / Vol. 61, No. 23 / Friday, February 2, 1996 / Proposed Rules DEPARTMENT OF LABOR 8:30 am on March 26, 1996 and understanding (MOU), BLS retained extending through March 28th, if responsibility for conducting the Occupational Safety and Health necessary. Annual Survey Of Occupational Injuries Administration ADDRESSES: Comments are to be And Illnesses, while responsibility for submitted in writing in quadruplicate, administering the recordkeeping system 29 CFR Parts 1904 and 1952 or 1 original (hard copy) and 1 disk was transferred to OSHA (ex. 6). [Docket No. R±02] (51¤4′′ or 31¤2′′) in WP 5.0, 5.1, 5.2, 6.0 or OSHA's responsibility includes ASCII. Note: Any information not developing, publishing, and providing Occupational Injury and Illness contained on disk; e.g., studies, articles, outreach for recordkeeping regulations Recording and Reporting etc. must be submitted in quadruplicate. and instructions. In 1991, OSHA created Requirements All comments shall be submitted to: the Office of Statistics to assume these Docket Officer, Docket No. R±02, responsibilities and to meet the data AGENCY: Occupational Safety and Health needs of the agency. Administration (OSHA), Department of Occupational Safety and Health Labor. Administration, Room N±2625, U.S. Purpose of the Records Department of Labor, 200 Constitution ACTION: Notice of Proposed rule. The injury and illness records are Avenue NW., Washington, DC 20210, intended to have multiple purposes. SUMMARY telephone (202) 219±7894. Comments of : The Occupational Safety and One purpose is to provide information Health Administration (OSHA) proposes 10 pages or less may be transmitted by for employers and employees, raising to revise Title 29 of the Code of Federal facsimile to (202) 219±5046 provided their awareness of the kinds of injuries Regulations Part 1904, Recording and the original and 4 copies of the and illnesses occurring in the workplace Reporting Occupational Injuries and comment are sent to the Docket Officer and their related hazards. -

Occupational Injury Or Illness Reporting Procedure
County of San Bernardino Department of Behavioral Health Occupational Injury or Illness Reporting Procedure Effective Date 7/94 Approval Date 11/17/06 Purpose To inform employees of the procedure to follow when employees or volunteers are involved in incidents that result in Occupational Injury or Illness. Definitions Occupationalinjury/iliness: An occupational injury or illness is one that arises out of employment or is suffered in the course of employment. Emergency: An emergency is defined here as an event that occurs in the workplace or in connection with employment that results in any serious injury requiring immediate attention, or necessitating medical treatment after or before physician's normal office hours. In cases of emergency, call 9-911. Workers' County employees and volunteers are protected under California Workers' Compensation Compensation laws for occupational injuries or illness. General The Personal Physician Request-Occupational Injury/Illness form must Information be completed prior to an injury or illness if there is a preference to be seen by a personal physician other than a county physician. Rolesl All occupational accidents, illnesses and incidents must be reported and Responsibilities handled by staff as stated below: Roles Responsibilities Employee (with on- • Immediately notify the supervisor or designee by telephone duty injury or illness) or in person. If unable to do so, ask someone to make the call • Complete the Employee's Claim for Workers Compensation Benefits form and submit it to the immediate supervisor or designee. (This form is to be completed only if medical treatment is needed or has already been received) 8FT 06-7020 Safety Page 1 of 3 County of San Bernardino Department of Behavioral Health Roles Responsibilities Employee (with on • If not filing a workers' compensation claim, record all minor duty injury or illness) injuries not requiring medical attention on the "First Aid (continued) Log" (located in the work area) and obtain the supervisor's signature on the log.