Physician As Military Officer: Conflicts Inof Pr Essional Duties
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Public Eye, Fall 2002
TheA PUBLICATION OF POLITICAL PublicEyeRESEARCH ASSOCIATES FALL 2002 • Volume XVI, No. 3 The Right Family Values The Christian Right’s “Defense of Marriage:” unpopular beliefs. Despite the First Amendment’s prohi- Democratic Rhetoric, Antidemocratic Politics bition against the establishment of religion by government, Christian conservatives By R. Claire Snyder cans oppose. While conservative Americans and their supporters often insist that Amer- are free to practice their beliefs and live their ica is really a “Christian nation.” They Introduction1 personal lives however they choose, the argue that the American founders believed government of the United States cannot he United States was founded as a that democratic political institutions would legitimately let those beliefs violate the “liberal democracy,” in which a secu- only work if grounded in religious mores T human rights of others in society. Similarly, lar government acts to protect the civil within civil society, emphasizing a comment it cannot generate public policy supporting rights and liberties of individuals rather made by John Adams: “Our Constitution a particular religious worldview or deny legal than imposing a particular vision of the was made only for a moral and religious peo- equality to certain groups of citizens. “good life” on its citizens. Equality before ple. It is wholly inadequate to the govern- the law constitutes one of the most funda- ment of any other.”9 William Bennett has mental principles of liberal democracy, as Liberal Democracy or Christian Nation? contributed greatly to this right-wing proj- does freedom from State-imposed religion. ect of revisionist historiography with the iberal political theory constitutes the These principles, enshrined in our found- publication of Our Sacred Honor: Words of ing documents, have become an almost Lmost important founding tradition of 5 Advice from the Founders, a volume that cat- universally accepted norm in U.S. -
CHELSEA RECORD Thursday, March 4, 2021
YOUR HOMETOWN NEWSPAPER SINCE 1890 VOLUME 120, No. 49 THURSDAY, MARCH 4, 2021 35 CENTS APPRECIATION Long-time School Committee member Liz McBride dies at 100 By Cary Shuman Mrs. Elizabeth “Liz” McBride, who served on the Chelsea School Com- mittee for many years and was a member of the Chelsea Kiwanis Club, died on March 1. She was 100 years old. McBride was a beloved public figure and attended numerous events hosted by local organizations and Elizabeth “Liz” McBride. was warmly welcomed by all. She had incredible en- Looking out over Chelsea from the height of the clocks on the City Hall Tower, one can see Boston and beyond. The vista ergy and spread her good- from the tower is incredible, and this rare view is courtesy of the full restoration of the tower that has started and should will efforts throughout the be completed by June. dren, and passionate about community. bicycle safety – she was a Mrs. McBride was a pi- great woman and we will Officials begin restoration of City Hall Tower, dome oneer in the local Kiwanis miss her terribly.” Club, becoming its first Ramirez said the mem- By Seth Daniel righting the clock and become expensive and here, we’ve re-done that female member. Kiwanis bers will be paying trib- even applying a new lay- disruptive. The tower sits roof four times. That was President Sylvia Ramirez ute to Mrs. McBride at While a lot of Chelsea er of gilding to the Hall’s right above the Council’s the driving force of this lauded Mrs. -

John Silber: Doing Well Doing Neocon Good
I (or perhaps a Givotian stooge entrepreneur, he realizes before If luck is with us, these charges such as Steve Dasbach, post- the other that the Party’s over, will serve as a successful pre- man from Indiana) will run for th<atthe members and donors emptive strike against a Silber national chair, preparatory for hawe been picked clean, and redux in Massachusetts politics. a drive for Nancy Lord for that the time has come to follow In the first place, unlike most President in ’96. (Only in the the Indian hustler Russell academics, Silber has been Libertarian Party does a rotten Means into other and greener making out like a bandit at BU, race by a presidential ticket pastures. Maybe some day the although, as the New York Times automatically set up the failed rest of the party will absorb the (Feb. 9) coyly adds, the ”news Vice-president for a promotion same lesson. articles have produced no clear four years hence.) The opposi- evidence of illegality by Dr. tion will coalesce either around Silber.” Thus, Silber earned a Mary Gingell for reelection, or total in 1991 of $414,715 in for one of her henchpeople to salary and bonuses from this succeed her. Other factions may John Silber: nonprofit institution of higher well surface. A combination of Doing Well Doing learning. And that’s only the ideological split and personal cash payout, For over the years, enmity should set up condi- Neocon Good BU has granted him $638,000 in tions for a doozy of a schism By ”loans” at little or no interest, after Salt Lake, with the losers M.N.R. -

Boston University Theta Tau
Boston University Theta Tau Table of Contents Letter from the Colony President………………………………………………………………………….3 Member Signatures……………………………………………………………………………………………...4 Member Profiles……..……………………………………………………………………………………………5 History of Boston University……………………………………………………………………………….16 History of the Boston University College of Engineering………………………………….......19 College of Engineering General Information………………………………………………………...22 History of the Boston University Colony……………………………………………………………...23 Letters of Recommendation………………………………………………………………………………..32 Boston University Colony of Theta Tau 2 Mr. Michael T. Abraham, Executive Director Theta Tau Professional Engineering Fraternity 1011 San Jacinto, Suite 205 Austin, TX 78701 Dear Brothers, I am honored to represent the Boston University Colony of Theta Tau in presenting our petition for chapter status. Over the past year, our colony has developed as an organization that truly respects and embodies the three pillars of Theta Tau: Service, Profession, and Brotherhood. Our colony has had the privilege of interacting with the national brotherhood on several occasions. This past summer, brothers from our colony represented Boston University at Theta Tau’s Leadership Academy. Their most important takeaway from this experience was the powerful sense of brotherhood that Theta Tau fosters and practices on a national level. As a colony, we seek to emulate that connection both between brothers, and with alumni in our immediate area. At our first annual Boston Local Alumni Networking Panel, we were lucky enough to host supportive alumni living in Boston. These brothers have since remained in contact with us as a support network to aid our colony in growing and succeeding as part of Theta Tau. As a member of our colony’s founding class I have seen firsthand the success our colony has achieved this past year. -

Neo-Conservatism and Corruption at Adelphi University, 1985-1997
The Twilight of Reason: Neo-Conservatism and Corruption at Adelphi University, 1985-1997 Daniel Rosenberg' During the administration of President Peter Diamandopoulos (1985- 1997), Adelphi University elicited considerable national attention. When faculty opposition to Diamandopoulos prompted the New York State Board of Regents to investigate reports of trustee and presidential malfeasance, the peculiar cir- cumstances at the Long Island institution became unprecedented matters of public scrutiny, drawing reporters from national, as well as local, media, and from publications dealing with higher education. Evidence before the Regents indicated exorbitant self-aggrandizement, extensive violations of non-profit and board procedures, and of ethical norms in education, leading the state body to remove the trustees in early 1997.* While the Regents' hearings and concurrent reporting publicly revealed the mercurial personality of Diamandopoulos, the coverage tended to obscure political factors, which facilitated and rationalized the operations of the presi- dent and his associates among the trustees. The following article will present an analysis of these dimensions in particular, giving relevant attention to, while leaving aside a fuller exposition of, the removal process. The president was a political animal, and not only in the customary sense of campus maneuvering, but one with clearly right-wing proclivities, notwith- standing his stated pursuit of an expansive "liberal learning." Despite the evi- dence of malfeasance, he attracted support from important organizations, national leaders, editorial boards, and foundations opposed to multiculturalism, campus unions, and the values of the 1960s perceived to be embodied within. However possessed (as the Regents hearings showed) of an overripe self- esteem, he was never abstractly opportunistic, but steered consistently right- ward. -
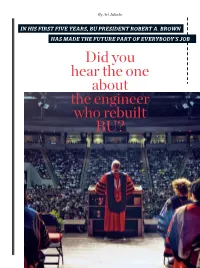
Did You Hear the One About the Engineer Who Rebuilt BU?
By Art Jahnke IN HIS FIRST FIVE YEARS, BU PRESIDENT ROBERT A. BROWN HAS MADE THE FUTURE PART OF EVERYBODY’S JOB Did you hear the one about the engineer who rebuilt BU? Winter–Spring 2011 BOSTONIA 27 222-512-51 BBostoniaWinter11_03.inddostoniaWinter11_03.indd 2727 22/4/11/4/11 22:36:36 PPMM “I MADE THE TRANSITION FROM COMPLICATED PHYSICAL SYSTEMS Five and a half years into Brown’s tenure, BU At last year’s Matriculation, he urged students to learn has seen four years of record surpluses and has quantitative reasoning and how to write clearly. increased financial aid to students. here were two to begin the job. By the time to pop up anytime, anywhere, have also set new records: things Robert Brown a new presidential search like targets in a Whack-A- prior to Brown’s presidency, promised himself he committee started talking to Mole game. the University had had only T would not get caught Brown in spring 2005, many “There were dead cats one gift of more than $10 mil- up in when he was consider- observers of higher educa- everywhere,” Brown recalls. lion. Since he took office, six ing taking the job of president tion were not looking at Bos- “And nobody wanted to bury large gifts account for more of Boston University. “One ton University as a model of them.” than $60 million. was what the Globe had writ- executive leadership. Ultimately, he says, he In September, the many ten about the University and The second item on dealt with the complexity by positive changes that Brown John Silber,” says Brown. -

Annual Report
ANNUAL REPORT 2015-2016 Table of Contents About the Elie Wiesel Center for Jewish Studies ........................................................................ 2 Director’s Message .............................................................................................................................. 3 Elie Wiesel (1928-2016) ..................................................................................................................... 4 People ....................................................................................................................................................... 6 .. Our Students ........................................................................................................................................... 6 Student Support .............................................................................................................................. 6 Undergraduate Student Highlight .............................................................................................. 7 Graduate Student Highlight: Samantha Pickette .......................................................................... 7 Leo Baeck Essay Prize .................................................................................................................................. 8 Faculty Highlights .................................................................................................................................... 8 Featured Faculty Publication ................................................................................................................... -

BU (Extreme) South
SPRING 2009 INSIDE: Do magnets repel sharks? arts&sciences Revered Dean Elsbeth Melville remembered Notorious traveling French sisters BU (extreme) South Geomorphologist David Marchant and his team of students discover Antarctica’s secret past C ONTENTS from the dean SPRING 2009 10 Open a newspaper or turn on a TV and it’s hard As all of us at BU come together to withstand this period of to avoid being bombarded by stories about economic uncertainty, Arts & Sciences remains strong. I am very “I felt that all the hours failed financial institutions, corporate layoffs, pleased to say that our ambitious program of faculty recruitment 12 and stock market tumbles. Indeed, these are is not affected by the freeze, and we are moving ahead with plans to they were in neither the troubling economic times. strengthen CAS, not only replacing faculty who retire or leave, but also classroom nor the library, This past fall, President Robert Brown expanding the faculty by as many as 100 new positions within the I was responsible for them.” faced the situation head-on. Rather than taking decade. The newest members of our faculty are impressive indeed. To a wait-and-see approach to the ongoing finan- get a sense of what they mean for the future of the College, I invite you Dean Elsbeth Melville (CAS’25) cial turmoil, he was one of the first university to take a look at the brief biographies in the roster of new appointments Photo courtesy of Craig O’Connell presidents to take serious proactive measures in the crisis. -

A Chilling of Discourse
Saint Louis University Law Journal Volume 50 Number 2 A Tribute to the Honorable Michael A. Article 13 Wolff (Winter 2006) 2006 A Chilling of Discourse David Barnhizer Cleveland State University, Cleveland-Marshall College of Law Follow this and additional works at: https://scholarship.law.slu.edu/lj Part of the Law Commons Recommended Citation David Barnhizer, A Chilling of Discourse, 50 St. Louis U. L.J. (2006). Available at: https://scholarship.law.slu.edu/lj/vol50/iss2/13 This Article is brought to you for free and open access by Scholarship Commons. It has been accepted for inclusion in Saint Louis University Law Journal by an authorized editor of Scholarship Commons. For more information, please contact Susie Lee. SAINT LOUIS UNIVERSITY SCHOOL OF LAW A CHILLING OF DISCOURSE DAVID BARNHIZER* I. INTRODUCTION ..................................................................................... 362 II. MULTICULTURALISM AND FRAGMENTATION ....................................... 365 III. LOSS OF OBJECTIVITY AND INTELLECTUAL INTEGRITY ....................... 370 IV. THE EFFECTS OF CHILLING ON THE INTEGRITY OF THE SCHOLAR .............................................................................................. 381 V. CHALLENGING “SOFT” REPRESSION ..................................................... 386 VI. CHILLING OF DISCOURSE THROUGH CONTROL OF ALLOWABLE SPEECH ............................................................................ 391 VII. CHILLING THROUGH INTOLERANCE AND THE SCHOLARSHIP OF RAGE ....................................................................... -

The Guardian, September 19, 1990
Wright State University CORE Scholar The Guardian Student Newspaper Student Activities 9-19-1990 The Guardian, September 19, 1990 Wright State University Student Body Follow this and additional works at: https://corescholar.libraries.wright.edu/guardian Part of the Mass Communication Commons Repository Citation Wright State University Student Body (1990). The Guardian, September 19, 1990. : Wright State University. This Newspaper is brought to you for free and open access by the Student Activities at CORE Scholar. It has been accepted for inclusion in The Guardian Student Newspaper by an authorized administrator of CORE Scholar. For more information, please contact [email protected]. e e uar 1an Issue No. 6, Volume 26 Wright State's Student Newspaper Wednesday, September 19, 1990 News Briefs ecopyright 1990, USA TODAY/Apple College Information Network Dugan fired for comments Gen. Michael Dugan was frred Monday as Air Force chief of staff after public comments about plans to bombard Iraq and personally target President Saddam Hussein. "He showed poor judgement at a very sensitive time," Defense Secretary Dick Cheney said after firing Dugan. 53, in the post only since July. Families richer in Florida Two Floridians - made instant million aires in the second largest lottery in U.S. history - still could not believe their luck Monday. Richard Piasecki, 58, a retired auto worker in New Sm~ and Tampa accountant Scott Smith, 35, are the first winners in Florida• s $106.5 million Bongo Bay entertains hundreds of Fall Fest spectators lottery. The six other winners, still unknown, have 180 days to come forward. WSU plans to remold image Shuttle meets fourth delay NASA Monday - for the fourth time since May - scrubbed the launch of the Kelly Keith Dunn shuttle Columbia after finding a poten Staff leading metropolitan university. -

The Absurd Enspaced a Darch Project Submitted To
THE ABSURD ENSPACED A DARCH PROJECT SUBMITTED TO THE GRADUATE DIVISION OF THE UNIVERSITY OF HAWAI‘I AT MĀNOA IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF DOCTOR OF ARCHITECTURE MAY 2016 By Chelsea Silvia DArch Committee: Lance Walters, Chairperson Arindam Chakrabarti Cathi Ho Schar Keywords: Absurd, Absurdism, Threshold Acknowledgements For my little brother, my mother, and my father. ii Abstract The contradictions between the ideal-reality, solid-void, and inside-outside are just a few of architecture’s most fundamental and accepted incompatibilities. Not exclusive to architecture, contradiction is ultimately a result of our human condition to seek out meaning and order in a meaningless, disorderly world. Albert Camus refers to this basic conflict between us and the universe as “absurdism” and lends only two solutions: a suicide or an acceptance. The purpose of this research is to enspace the absurd, which is to realize in architecture an acceptance of absurdity. This effort establishes that the opposing roles within contradiction are not two independent, separate forces up for casual omission (suicide) to ease complexity, but rather that these opposing roles are in fact two intimately entwined roles of the same part. The absurd is explored through Camus’ collected works as well as through precedents of absurd demonstration from literature to the arts and toward architecture. Undertaking the contradiction as the clearest articulation of the absurd and upon recognizing the threshold as the purest contradiction in architecture, this work finds the absurdity in architecture to be the threshold. Out of our human condition to search for reason and order, we separate spaces (functions) within architecture so we may make sense of them. -

Pressed but Not Crushed1 the UT Saga of Barbara Smith Conrad
Pressed but Not Crushed1 The UT Saga of Barbara Smith Conrad 1 Reference to 2 Corinthians 4:8. 1 CAST Last Year we had 61 scenes, and 14 actors. There were 4 males and 10 females. Last year’s cast assumed 24 characters: 7 were male, and 16 female. This proposal envisions 49 scenes. 14 actors again: There could be 5 males, and 9 females. The 2018 cast would assume 20 characters: 9 would be males, 11 females below. There is also a need for2 extras. The Barbara Group (African Americans): 1. Barbara Conrad 2. Father: Conrad Smith 3. Mother: Jerrie Lee Smith 4. Sister: Connie. 5. Cindy Chavez: Good College Friend, Roommate. The Anti Barbara Group: 6. Representative Joe Chapman of Sulphur Springs 7. Mrs. H.E. Howard, Chapman Donor. Moral Guardian. 8. Bo Angstrom. White Troublemaker #1 9. Ron Whitehead White Troublemaker #2 10. White Diva Rival #1 Martha Ann Kelly 11. White Diva Rival #2 Carol Cold 12. Reporter (Female). The University Group 13. Tom Sealy, UT Board of Regents Chair 14. John Silber, Visiting Philosophy Professor 15. Logan Wilson, UT President 16. Arno Nowotny, Progressive Dean 17. H.Y. McCown, “Apocalyptic HY.” Dean of Student Services 18. Edra Gustafson: White Woman Professor who first acts “Strange” Student Activists: 19. Maurie Suttle: Chair of Desegregation Committee 20. Joann Thompson: President of the University Religious Council Ancillary Roles (extras): 21. Ticket Takers TWO. 2 Part I: The Sending Scene 1: The Theme INT. BLACKSCREEN – CONTINUOUS SCREEN shows Bible verse in white text. NARRATOR (unseen) 2 Corinthians 4:8.