Immunoreactivity of CD99 in Non-Hodgkin's Lymphoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Expression of ALK1 and P80 in Inflammatory Myofibroblastic Tumor and Its Mesenchymal Mimics: a Study of 135 Cases Melissa H
Expression of ALK1 and p80 in Inflammatory Myofibroblastic Tumor and Its Mesenchymal Mimics: A Study of 135 Cases Melissa H. Cessna, M.D., Holly Zhou, M.D., Warren G. Sanger, Ph.D., Sherrie L. Perkins, M.D., Ph.D., Sheryl Tripp, M.T., Diane Pickering, M.S., Clark Daines, M.D., Cheryl M. Coffin, M.D. Department of Pathology, Primary Children’s Medical Center and University of Utah School of Medicine, Salt Lake City, Utah (MHC, HZ, SLP, ST, CD, CMC); and Department of Pediatrics, University of Nebraska Medical Center, Omaha, Nebraska (WGS, DP) between structural abnormalities involving 2p23 or Abnormalities of chromosome 2p23 with expres- additional copies of 2p23, it supports the concept of sion of ALK1 and p80 occur in both inflammatory ALK involvement in a larger group of neoplasms, myofibroblastic tumor (IMT) and anaplastic large some of which have other documented clonal ab- cell lymphoma. This immunohistochemical study normalities. In IMT, immunohistochemistry for investigates whether the ALK family of neoplasms ALK1 and p80 is useful as an indicator of a 2p23 includes fibroblastic–myofibroblastic, myogenic, abnormality, but it must be interpreted in the con- and spindle cell tumors. Formalin-fixed paraffin- text of histologic and other clinicopathologic data if embedded archival tissues from 10 IMTs and 125 used as an adjunct to differential diagnosis. other soft tissue tumors were stained for ALK1 and p80 with standard immunohistochemistry. ALK1 KEY WORDS: ALK gene rearrangements, ALK im- and/or p80 reactivity was observed in a cytoplasmic munohistochemistry, Anaplastic large cell lym- pattern in IMT (4/10; 40%), malignant peripheral phoma, Inflammatory myofibroblastic tumor. -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Characterization of FLT3-Itdmut Acute Myeloid Leukemia
Travaglini et al. Blood Cancer Journal (2020) 10:85 https://doi.org/10.1038/s41408-020-00352-9 Blood Cancer Journal ARTICLE Open Access Characterization of FLT3-ITDmut acute myeloid leukemia: molecular profiling of leukemic precursor cells Serena Travaglini1, Daniela Francesca Angelini 2, Valentina Alfonso1, Gisella Guerrera2,SerenaLavorgna1, Mariadomenica Divona1, Anna Maria Nardozza1, Maria Irno Consalvo1, Emiliano Fabiani1,MarcoDeBardi 2, Benedetta Neri3,FabioForghieri4, Francesco Marchesi5, Giovangiacinto Paterno1, Raffaella Cerretti1, Eva Barragan 6, Valentina Fiori7,SabrinaDominici7, Maria Ilaria Del Principe1, Adriano Venditti 1, Luca Battistini2, William Arcese1, Francesco Lo-Coco1, Maria Teresa Voso 1,2 and Tiziana Ottone1,2 Abstract Acute myeloid leukemia (AML) with FLT3-ITD mutations (FLT3-ITDmut) remains a therapeutic challenge, with a still high relapse rate, despite targeted treatment with tyrosine kinase inhibitors. In this disease, the CD34/CD123/CD25/CD99+ leukemic precursor cells (LPCs) phenotype predicts for FLT3-ITD-positivity. The aim of this study was to characterize the distribution of FLT3-ITD mutation in different progenitor cell subsets to shed light on the subclonal architecture of FLT3-ITDmut AML. Using high-speed cell sorting, we sequentially purified LPCs and CD34+ progenitors in samples from patients with FLT3-ITDmut AML (n = 12). A higher FLT3-ITDmut load was observed within CD34/CD123/CD25/CD99+ LPCs, as compared to CD34+ progenitors (CD123+/−,CD25−,CD99low/−)(p = 0.0005) and mononuclear cells (MNCs) (p < 0.0001). This was associated with significantly increased CD99 mean fluorescence intensity in LPCs. 1234567890():,; 1234567890():,; 1234567890():,; 1234567890():,; Significantly higher FLT3-ITDmut burden was also observed in LPCs of AML patients with a small FLT3-ITDmut clones at diagnosis. -

The Health-Related Quality of Life of Sarcoma Patients and Survivors In
Cancers 2020, 12 S1 of S7 Supplementary Materials The Health-Related Quality of Life of Sarcoma Patients and Survivors in Germany—Cross-Sectional Results of A Nationwide Observational Study (PROSa) Martin Eichler, Leopold Hentschel, Stephan Richter, Peter Hohenberger, Bernd Kasper, Dimosthenis Andreou, Daniel Pink, Jens Jakob, Susanne Singer, Robert Grützmann, Stephen Fung, Eva Wardelmann, Karin Arndt, Vitali Heidt, Christine Hofbauer, Marius Fried, Verena I. Gaidzik, Karl Verpoort, Marit Ahrens, Jürgen Weitz, Klaus-Dieter Schaser, Martin Bornhäuser, Jochen Schmitt, Markus K. Schuler and the PROSa study group Includes Entities We included sarcomas according to the following WHO classification. - Fletcher CDM, World Health Organization, International Agency for Research on Cancer, editors. WHO classification of tumours of soft tissue and bone. 4th ed. Lyon: IARC Press; 2013. 468 p. (World Health Organization classification of tumours). - Kurman RJ, International Agency for Research on Cancer, World Health Organization, editors. WHO classification of tumours of female reproductive organs. 4th ed. Lyon: International Agency for Research on Cancer; 2014. 307 p. (World Health Organization classification of tumours). - Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO Classification of Tumours of the Urinary System and Male Genital Organs—Part B: Prostate and Bladder Tumours. Eur Urol. 2016 Jul;70(1):106–19. - World Health Organization, Swerdlow SH, International Agency for Research on Cancer, editors. WHO classification of tumours of haematopoietic and lymphoid tissues: [... reflects the views of a working group that convened for an Editorial and Consensus Conference at the International Agency for Research on Cancer (IARC), Lyon, October 25 - 27, 2007]. 4. ed. -

Radiation-Associated Synovial Sarcoma
Radiation-Associated Synovial Sarcoma: Clinicopathologic and Molecular Analysis of Two Cases Jean-François Egger, M.D., Jean-Michel Coindre, M.D., Jean Benhattar, Ph.D., Philippe Coucke, M.D., Louis Guillou, M.D. University Institute of Pathology (J-FE, JB, LG) and Department of Radiooncology, University Hospital (PC), Lausanne, Switzerland; Bergonié Institute and University of Bordeaux II (J-MC), Bordeaux, France region, or viscera (1, 2). SS bears the t(X;18) (SYT- Development of a soft-tissue sarcoma is an infre- SSX) reciprocal translocation that seems to be spe- quent but well-known long-term complication of cific for this tumor type and can be routinely de- radiotherapy. Malignant fibrous histiocytomas, ex- tected in paraffin-embedded tissue using the traskeletal osteosarcomas, fibrosarcomas, malig- reverse transcriptase–polymerase chain reaction nant peripheral nerve sheath tumors, and angiosar- (RT-PCR; 3–6). Radiation-associated sarcomas are comas are most frequently encountered. Radiation- an infrequent but well-known long-term complica- associated synovial sarcomas are exceptional. We tion of radiotherapy (7–16). They occur in about report the clinicopathologic, immunohistochemi- 1/1000 patients who have undergone radiation cal, and molecular features of two radiation- therapy (7–11). Radiation-associated sarcomas are associated synovial sarcomas. One tumor developed defined as sarcomas arising in a previously irradi- in a 42-year-old female 17 years after external irra- ated field after a latency period of Ն2 years (12). diation was given for breast carcinoma; the other They usually show a more aggressive clinical course occurred in a 34-year-old female who was irradiated associated with shortened patient survival as com- at the age of 7 years for a nonneoplastic condition of pared with sporadic sarcomas (9–12, 14). -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -

Synovial Sarcoma: Recent Discoveries As a Roadmap to New Avenues for Therapy
Published OnlineFirst January 22, 2015; DOI: 10.1158/2159-8290.CD-14-1246 REVIEW Synovial Sarcoma: Recent Discoveries as a Roadmap to New Avenues for Therapy Torsten O. Nielsen 1 , Neal M. Poulin 1 , and Marc Ladanyi 2 ABSTRACT Oncogenesis in synovial sarcoma is driven by the chromosomal translocation t(X,18; p11,q11), which generates an in-frame fusion of the SWI/SNF subunit SS18 to the C-terminal repression domains of SSX1 or SSX2. Proteomic studies have identifi ed an integral role of SS18–SSX in the SWI/SNF complex, and provide new evidence for mistargeting of polycomb repression in synovial sarcoma. Two recent in vivo studies are highlighted, providing additional support for the importance of WNT signaling in synovial sarcoma: One used a conditional mouse model in which knock- out of β-catenin prevents tumor formation, and the other used a small-molecule inhibitor of β-catenin in xenograft models. Signifi cance: Synovial sarcoma appears to arise from still poorly characterized immature mesenchymal progenitor cells through the action of its primary oncogenic driver, the SS18–SSX fusion gene, which encodes a multifaceted disruptor of epigenetic control. The effects of SS18–SSX on polycomb-mediated gene repression and SWI/SNF chromatin remodeling have recently come into focus and may offer new insights into the basic function of these processes. A central role for deregulation of WNT–β-catenin sig- naling in synovial sarcoma has also been strengthened by recent in vivo studies. These new insights into the the biology of synovial sarcoma are guiding novel preclinical and clinical studies in this aggressive cancer. -

CD29 Identifies IFN-Γ–Producing Human CD8+ T Cells With
+ CD29 identifies IFN-γ–producing human CD8 T cells with an increased cytotoxic potential Benoît P. Nicoleta,b, Aurélie Guislaina,b, Floris P. J. van Alphenc, Raquel Gomez-Eerlandd, Ton N. M. Schumacherd, Maartje van den Biggelaarc,e, and Monika C. Wolkersa,b,1 aDepartment of Hematopoiesis, Sanquin Research, 1066 CX Amsterdam, The Netherlands; bLandsteiner Laboratory, Oncode Institute, Amsterdam University Medical Center, University of Amsterdam, 1105 AZ Amsterdam, The Netherlands; cDepartment of Research Facilities, Sanquin Research, 1066 CX Amsterdam, The Netherlands; dDivision of Molecular Oncology and Immunology, Oncode Institute, The Netherlands Cancer Institute, 1066 CX Amsterdam, The Netherlands; and eDepartment of Molecular and Cellular Haemostasis, Sanquin Research, 1066 CX Amsterdam, The Netherlands Edited by Anjana Rao, La Jolla Institute for Allergy and Immunology, La Jolla, CA, and approved February 12, 2020 (received for review August 12, 2019) Cytotoxic CD8+ T cells can effectively kill target cells by producing therefore developed a protocol that allowed for efficient iso- cytokines, chemokines, and granzymes. Expression of these effector lation of RNA and protein from fluorescence-activated cell molecules is however highly divergent, and tools that identify and sorting (FACS)-sorted fixed T cells after intracellular cytokine + preselect CD8 T cells with a cytotoxic expression profile are lacking. staining. With this top-down approach, we performed an un- + Human CD8 T cells can be divided into IFN-γ– and IL-2–producing biased RNA-sequencing (RNA-seq) and mass spectrometry cells. Unbiased transcriptomics and proteomics analysis on cytokine- γ– – + + (MS) analyses on IFN- and IL-2 producing primary human producing fixed CD8 T cells revealed that IL-2 cells produce helper + + + CD8 Tcells. -

Blood Flow Guides Sequential Support of Neutrophil Arrest and Diapedesis
RESEARCH ARTICLE Blood flow guides sequential support of neutrophil arrest and diapedesis by PILR-b 1 and PILR-a Yu-Tung Li, Debashree Goswami†, Melissa Follmer, Annette Artz, Mariana Pacheco-Blanco, Dietmar Vestweber* Vascular Cell Biology, Max Planck Institute of Molecular Biomedicine, Mu¨ nster, Germany Abstract Arrest of rapidly flowing neutrophils in venules relies on capturing through selectins and chemokine-induced integrin activation. Despite a long-established concept, we show here that gene inactivation of activating paired immunoglobulin-like receptor (PILR)-b1 nearly halved the efficiency of neutrophil arrest in venules of the mouse cremaster muscle. We found that this receptor binds to CD99, an interaction which relies on flow-induced shear forces and boosts chemokine-induced b2-integrin-activation, leading to neutrophil attachment to endothelium. Upon arrest, binding of PILR-b1 to CD99 ceases, shifting the signaling balance towards inhibitory PILR-a. This enables integrin deactivation and supports cell migration. Thus, flow-driven shear forces guide sequential signaling of first activating PILR-b1 followed by inhibitory PILR-a to prompt neutrophil arrest and then transmigration. This doubles the efficiency of selectin-chemokine driven neutrophil arrest by PILR-b1 and then supports transition to migration by PILR-a. DOI: https://doi.org/10.7554/eLife.47642.001 *For correspondence: [email protected] Present address: †Center for Global Infectious Disease Introduction Research, Seattle Childrens Host defense against pathogens depends on the recruitment of leukocytes to sites of infections Research Institute, Seattle, (Ley et al., 2007). Selectins capture leukocytes to the endothelial cell surface by binding to glyco- United States conjugates (McEver, 2015). -
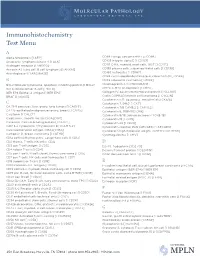
IHC Test Menu
Immunohistochemistry Test Menu A Alpha fetoprotein [I AFP] CD99 Ewings sarcoma PNET [I CD99] Anaplastic lymphoma kinase -1 [I ALK] CD103 Integrin alpha E [I CD103] Androgen receptor [I ANDRO]* CD117 C-Kit, myeloid, mast cells, GIST [I CD117] Annexin A1, hairy cell, B cell lymphoma [I ANXA1] CD138 plasma cells, subset epithelial cells [I CD138] Anti-Arginase-1 [I ARGINASE] CD163 histiocytes [I CD163] CDK4 cyclin-depdendent kinase-4, clone DCS-31 [I CDK4] B CDX2 colorectal carcinoma [I CDX2] BCL2 follicular lymphoma, apoptosis inhibiting protein [I BCL2] Chromogranin A [I CHROGRAN] BCL6 follicle center B-cell [I BCL6] CMYC C-MYC oncoprotein [I CMYC] BER EP4 Epithelial antigen [I BER EP4] Collagen IV, basement membrane protein [I CLLGIV] BRAF [I V600E] Cyclin D1/PRAD1 mantle cell lymphoma [I CYCLIN] Cytokeratin 5/6, squamous, mesothelial [I CK5/6] C Cytokeratin 7, 54kD [I CK7] CA 19-9 pancreas, liver, ovary, lung tumors [I CA19 9] Cytokeratin 7/8 CAM5.2 [I CAM 5.2] CA 125 epitheliod malignancies ovary, breast [I CA125] Cytokeratin 8, 35BH11 [I CK8] Calcitonin [I CALCT] Cytokeratin 8/18, adenocarcinoma [I CK8/18] Caldesmon, smooth muscle [I CALDSM] Cytokeratin 19 [I CK19] Calretinin; Calcium binding protein [I CALRT] Cytokeratin 20 [I CK20] CAM 5.2 Cytokeratin 7/Cytokeratin 8 [I CAM 5.2] Cytokeratin cocktail, PAN (AE1/AE3) [I AE1/AE3] Carcinoembryonic antigen (CEA) [I CEA] Cytokeratin high molecular weight; 34BE12 [I CK HMW] Cathepsin D, breast carcinoma [I CATHD] Cytomegalovirus [I CMV] CD1a cortical thymocyctes, Langerhans cells [I CD1a] -

The Role of Cytogenetics and Molecular Diagnostics in the Diagnosis of Soft-Tissue Tumors Julia a Bridge
Modern Pathology (2014) 27, S80–S97 S80 & 2014 USCAP, Inc All rights reserved 0893-3952/14 $32.00 The role of cytogenetics and molecular diagnostics in the diagnosis of soft-tissue tumors Julia A Bridge Department of Pathology and Microbiology, University of Nebraska Medical Center, Omaha, NE, USA Soft-tissue sarcomas are rare, comprising o1% of all cancer diagnoses. Yet the diversity of histological subtypes is impressive with 4100 benign and malignant soft-tissue tumor entities defined. Not infrequently, these neoplasms exhibit overlapping clinicopathologic features posing significant challenges in rendering a definitive diagnosis and optimal therapy. Advances in cytogenetic and molecular science have led to the discovery of genetic events in soft- tissue tumors that have not only enriched our understanding of the underlying biology of these neoplasms but have also proven to be powerful diagnostic adjuncts and/or indicators of molecular targeted therapy. In particular, many soft-tissue tumors are characterized by recurrent chromosomal rearrangements that produce specific gene fusions. For pathologists, identification of these fusions as well as other characteristic mutational alterations aids in precise subclassification. This review will address known recurrent or tumor-specific genetic events in soft-tissue tumors and discuss the molecular approaches commonly used in clinical practice to identify them. Emphasis is placed on the role of molecular pathology in the management of soft-tissue tumors. Familiarity with these genetic events -

WO 2018/067991 Al 12 April 2018 (12.04.2018) W !P O PCT
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2018/067991 Al 12 April 2018 (12.04.2018) W !P O PCT (51) International Patent Classification: achusetts 021 15 (US). THE BROAD INSTITUTE, A61K 51/10 (2006.01) G01N 33/574 (2006.01) INC. [US/US]; 415 Main Street, Cambridge, Massachu C07K 14/705 (2006.01) A61K 47/68 (2017.01) setts 02142 (US). MASSACHUSETTS INSTITUTE OF G01N 33/53 (2006.01) TECHNOLOGY [US/US]; 77 Massachusetts Avenue, Cambridge, Massachusetts 02139 (US). (21) International Application Number: PCT/US2017/055625 (72) Inventors; and (71) Applicants: KUCHROO, Vijay K. [IN/US]; 30 Fairhaven (22) International Filing Date: Road, Newton, Massachusetts 02149 (US). ANDERSON, 06 October 2017 (06.10.2017) Ana Carrizosa [US/US]; 110 Cypress Street, Brookline, (25) Filing Language: English Massachusetts 02445 (US). MADI, Asaf [US/US]; c/o The Brigham and Women's Hospital, Inc., 75 Francis (26) Publication Language: English Street, Boston, Massachusetts 021 15 (US). CHIHARA, (30) Priority Data: Norio [US/US]; c/o The Brigham and Women's Hospital, 62/405,835 07 October 2016 (07.10.2016) US Inc., 75 Francis Street, Boston, Massachusetts 021 15 (US). REGEV, Aviv [US/US]; 15a Ellsworth Ave, Cambridge, (71) Applicants: THE BRIGHAM AND WOMEN'S HOSPI¬ Massachusetts 02139 (US). SINGER, Meromit [US/US]; TAL, INC. [US/US]; 75 Francis Street, Boston, Mass c/o The Broad Institute, Inc., 415 Main Street, Cambridge, (54) Title: MODULATION OF NOVEL IMMUNE CHECKPOINT TARGETS CD4 FIG.