Primary Biliary Cirrhosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Successful Conservative Treatment of Pneumatosis Intestinalis and Portomesenteric Venous Gas in a Patient with Septic Shock
SUCCESSFUL CONSERVATIVE TREATMENT OF PNEUMATOSIS INTESTINALIS AND PORTOMESENTERIC VENOUS GAS IN A PATIENT WITH SEPTIC SHOCK Chen-Te Chou,1,3 Wei-Wen Su,2 and Ran-Chou Chen3,4 1Department of Radiology, Changhua Christian Hospital, Er-Lin branch, 2Department of Gastroenterology, Changhua Christian Hospital, 3Department of Biomedical Imaging and Radiological Science, National Yang-Ming University, and 4Department of Radiology, Taipei City Hospital, Taipei, Taiwan. Pneumatosis intestinalis (PI) and portomesenteric venous gas (PMVG) are alarming radiological findings that signify bowel ischemia. The management of PI and PMVG remain a challenging task because clinicians must balance the potential morbidity associated with unnecessary sur- gery with inevitable mortality if the necrotic bowel is not resected. The combination of PI, portal venous gas, and acidosis typically indicates bowel ischemia and, inevitably, necrosis. We report a patient with PI and PMVG caused by septic shock who completely recovered after conservative treatment. Key Words: bowel ischemia, computed tomography, pneumatosis intestinalis, portal venous gas, portomesenteric venous gas (Kaohsiung J Med Sci 2010;26:105–8) Pneumatosis intestinalis (PI) and portomesenteric CASE PRESENTATION venous gas (PMVG) are alarming radiologic findings that signify bowel ischemia [1]. PI and PMVG are A 78-year-old woman who presented with intermittent often described as an advanced sign of bowel injury, fever for 3 days was referred to the emergency depart- indicating irreversible injury caused by transmural ment of our hospital. The patient had a history of ischemia [2]. Bowel ischemia may be associated with type 2 diabetes mellitus, congestive heart failure, and perforation and has a high mortality rate. Many au- prior cerebral infarct. -

PAN: Upper GI Haemorrhage
International Journal of Research Studies in Medical and Health Sciences Volume 2, Issue 1, 2017, PP 7-10 ISSN : 2456-6373 http://dx.doi.org/10.22259/ijrsmhs.0201003 Visceral Microaneurysms of Polyarteritis Nodosa: Presentation with Recurrent Upper GI Haemorrhage needing Total Gastrectomy Dr Senthil Kumar MP MBBS, MS, FRCS (Edin), FRCS (Gen Surg) Additional Professor, Liver transplantation, ILBS, New Delhi, India Mr Dipankar Mukherjee MS FRCS (Glas), FRCS (Eng), FRCS (Gen Surg) Consultant Upper GI surgeon, Queens Hospital Romford, Essex, UK ABSTRACT: Polyarteritis nodosa (PAN) is a systemic necrotising vasculitis which is a rare but important cause of gastrointestinal bleeding. A sixty nine year old lady presented with life threatening upper gastrointestinal bleeding from the stomach. Multiple attempts at endoscopic localisation and therapy failed, as did one attempt at therapeutic splenic artery embolisation and two laparotomies. She finally underwent total gastrectomy. Gastric histology revealed necrotising arteritis consistent with polyarteritis nodosa. On retrospect she was found to have a number of features of polyarteritis nodosa, including the classic visceral microaneurysms on angiography. She responded to intravenous corticosteroids, but succumbed to a myocardial infarction three months later. Keywords: Polyarteritis nodosa; PAN; GI haemorrhage; Gastrectomy; Microaneurysms INTRODUCTION Although upper gastrointestinal haemorrhage is a commonly encountered clinical problem, it is a rare initial mode of presentation for a vasculitic process such as polyarteritis nodosa (PAN). Polyarteritis nodosa is a systemic necrotising vasculitis involving the medium and small sized arteries in many vascular beds. Though expansile arterial lesions (microaneurysms and ectasias) at arterial branch points are classical, occlusive arterial lesions may be at least equally and possibly more common.1 Gastrointestinal involvement includes bleeding, ulceration, infarction and perforation of hollow viscera including appendix and gall bladder. -
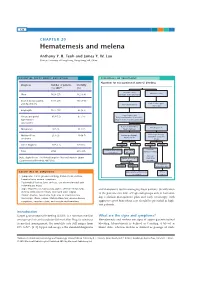
Hematemesis and Melena Chapter
126 CHAPTER 20 Hematemesis and melena Anthony Y. B. Teoh and James Y. W. Lau Chinese University of Hong Kong, Hong Kong SAR, China ESSENTIAL FACTS ABOUT CAUSATION ESSENTIALS OF TREATMENT Algorithm for management of acute GI bleeding Diagnosis Number of patients Mortality (%) 200716 (%) Major bleeding Minor bleeding Ulcer 1826 (27) 162 (8.9) (unstable hemodynamics) Erosive disease (gastric 1731 (26) 195 (14.1) Early elective upper and duodenum) Active resuscitation endoscopy Esophagitis 1177 (17) 65 (5.5) Urgent endoscopy Varices and portal 819 (12) 87 (14) Early administration of vasoactive hypertensive drugs in suspected variceal bleeding gastropathy Active ulcer bleeding Bleeding varices Malignancy 187 (3) 31 (17) Major stigmata Mallory-Weiss 213 (3) 10 (4.7) Endoscopic therapy Endoscopic therapy Adjunctive PPI Adjunctive vasoactive syndrome drugs Other diagnosis 797 (12) 125 (16) Success Failure Success Failure Continue Continue ulcer healing Recurrent Total 6750 675 (10) vasoactive drugs medications bleeding Variceal Data adapted from The United Kingdom National Audit in Upper Repeat endoscopic eradication Gastrointestinal Bleeding 2007 [16]. therapy program Sengstaken- Success Failure Blakemore tube ESSENTIALS OF DIAGNOSIS Angiographic embolization TIPS vs vs. surgery surgery • Symptoms: Coffee ground vomiting, hematemesis, melena, hematochezia, anemic symptoms • Past medical history: Liver cirrhosis, use of non-steroidal anti- inflammatory drugs • Signs: Hypotension, tachycardia, pallor, altered mental status, and therapeutic tool in managing these patients. Stratification melena or blood per rectum, decreased urine output of the patients into low- or high-risk groups aids in formulat- • Bloods: Anemia, raised urea, high urea to creatinine ratio • Endoscopy: Ulcers, varices, Mallory-Weiss tear, erosive disease, ing a clinical management plan and early endoscopy with neoplasms, vascular ectasia, and vascular malformations aggressive post-hemostasis care should be provided in high- risk patients. -

GASTROINTESTINAL COMPLAINT Nausea, Vomiting, Or Diarrhea (For Abdominal Pain – Refer to SO-501) I
DESCHUTES COUNTY ADULT JAIL SO-559 L. Shane Nelson, Sheriff Standing Order Facility Provider: October 17, 2018 STANDING ORDER GASTROINTESTINAL COMPLAINT Nausea, Vomiting, or Diarrhea (for Abdominal Pain – refer to SO-501) I. ASSESSMENT a. History i. Onset and duration ii. Frequency of vomiting, nausea, or diarrhea iii. Blood in stool or black stools? Blood in emesis or coffee-ground appearance? If yes, refer to SO-510 iv. Medications taken – do they help? v. Do they have abdominal pain? If yes, refer to SO-501 Abdominal Pain. vi. Do they have other symptoms – dysuria, urinary frequency, urinary urgency, urinary incontinence, vaginal/penile discharge, hematuria, fever, chills, flank pain, abdominal/pelvic pain in females or testicular pain in males, vaginal or penile lesions/sores? (if yes to any of the above – refer to Dysuria SO-522) vii. LMP in female inmates – if unknown, obtain HCG viii. History of substance abuse? Are they withdrawing? Refer to appropriate SO based on substance history and withdrawal concerns. ix. History of IBS or other known medical causes of chronic diarrhea, nausea, or vomiting? Have prescriptions been used for this in the past? x. History of abdominal surgeries? xi. Recent exposure to others with same symptoms? b. Exam i. Obtain Vital signs, including temperature ii. If complaints of dizziness or lightheadedness with standing, obtain orthostatic VS. iii. Is there jaundice present? iv. Are there signs of dehydration – tachycardia, tachypnea, lethargy, changes in mental status, dry mucous membranes, pale skin color, decreased skin turgor? v. Are you concerned for an Acute Gastroenteritis? Supersedes: March 20, 2018 Review Date: October 2020 Total Pages: 3 1 SO-559 October 17, 2018 Symptoms Exam Viruses cause 75-90% of acute gastroenteritis here in the US. -

Fever, Abdominal Pain, and Jaundice in a 43-Year-Old Woman
INTERNAL MEDICINE BOARD REVIEW DAVID L. LONGWORTH, MD, EDITOR JAMES K. STOLLER, MD, EDITOR KSRTI SHETTY, MD Dr. Shetty is a resident in internal medicine at the Cleveland Clinic. WILLIAM D. CAREY, MD Dr. Carey is head of the Section of Hepatology and director of the liver transplantation pro- gram at the Cleveland Clinic. He was recently president of the American College of Gastroenterology. Fever, abdominal pain, and jaundice in a 43-year-old woman WHAT IS THE DIAGNOSIS? 4 3-year-old Caucasian woman comes to the emergency room because of right On the basis of the clinical picture and upper abdominal pain that has lasted 2 1 laboratory data, what is the most likely days. The pain is dull and aching, is diagnosis? unrelated to food, and does not radiate. • Acute viral hepatitis AShe notes that her skin tone has become more • Acute cholecystitis yellowish lately, and her urine is dark. • Alcoholic hepatitis The patient says she has drunk three to • Acetaminophen toxicity four beers every day since the age of 18, and • Acute hepatic venous occlusion occasional drinks of vodka or gin on weekends. She abused intravenous drugs in her 20s, but This woman has the classic clinical triad of quit after successful drug rehabilitation. She alcoholic hepatitis: fever, jaundice, and tender has no history erf jaundice, hematemesis, mele- hepatomegaly.1 However, it is imperative to na, ascites, or encephalopathy. She has lost exclude other causes of abdominal pain, such approximately 15 lb over the past 6 months, as biliary tract obstruction, impaired hepatic and her appetite is poor. -

A Case of Pneumatosis Cytoides Intestinalis Successfully Treated by Inhalation of High Concentration Oxygen
Case Report A Case of Pneumatosis Cytoides Intestinalis Successfully Treated by Inhalation of High Concentration Oxygen JMAJ 48(10): 513–517, 2005 Toshihito Fujii,*1 Makoto Takaoka,*1 Yoshihiro Tagawa,*1 Takahiro Kitano,*1 Mika Ohmiya,*1 Yoshinari Hashimoto,*2 Kazuichi Okazaki*3 Abstract A 44-year-old man was referred to our hospital because of a positive fecal occult blood test. A barium enema study revealed numerous oval-shaped, elevated lesions with smooth surfaces in the region including the ascending colon. He was admitted to our hospital for investigation and therapy. Based on colonoscopic examination, we /5hoursןdiagnosed him as having pneumatosis cytoides intestinalis (PCI). He was treated with oxygen (5L/min day for 14 days) via a nasal cannula. Most of the multiple cysts diminished and some changed into white scars. The simplicity of oxygen therapy supports its use as a first-line treatment. Key words Pneumatosis cystoides interstinalis, High-concentration oxygen inhalation Family history: Not remarkable. Introduction Past exposure: No past exposure to trichloro- ethylene. Pneumatosis cystoides intestinalis (PCI) is a Present illness: The patient was found to be relatively rare condition in which numerous positive for fecal occult blood on a health screen- gas-filled cysts mainly containing nitrogen are ing, and was referred to our hospital for detailed formed within the intestinal wall. While idio- examination. An outpatient barium enema study pathic and secondary cases are known, the latter revealed numerous oval-shaped, elevated lesions may result from exposure to trichloroethylene, with smooth surfaces in the region from the chronic respiratory diseases such as pulmonary hepatic flexure to the ascending colon. -

Newborn Jaundice and Phototherapy
Newborn Jaundice/Phototherapy Jaundice is the yellow color seen in the skin of many newborns, and is usually harmless. Jaundice is caused by an excess of bilirubin in the blood. Bilirubin is made by the normal breakdown of red blood cells. Bilirubin is processed through the liver. Before the baby is born the mothers liver does this for the baby. After the baby is born, it might take a few days for the baby’s liver to get better at removing bilirubin. If the bilirubin becomes too high, it will need to be treated to prevent serious complications such as hearing loss, intellectual impairment and brain damage. A small instrument called a Bilimeter is used assess bilirubin levels. This is a non-invasive method and gives results in a matter of seconds. A graph is used to assess the age of an infant to the bilirubin level. If the level is moderate to high, a blood test is done to determine the exact level. Treatment for high bilirubin levels is done by phototherapy. Phototherapy is the use of special lights to help your baby break down the bilirubin. Treatment Expose as much of your baby’s skin to the lights as possible. A blood sample will be drawn on your baby to check the bilirubin level. This may happen more than once a day Keep your baby’s eyes covered with the mask provided while your baby is receiving phototherapy. while the lights are on. The baby can be in the room with you or in the nursery if Keep your baby under the lights as much as possible. -

Hepatitis A, Acute
Hepatitis A, Acute *NOTE-HIGHLIGHTED SECTION HAS BEEN REVISED IMMEDIATELY REPORTABLE DISEASE Per NJAC 8:57, healthcare providers and administrators shall immediately report by telephone confirmed and suspected cases of acute hepatitis A to the health officer of the jurisdiction where the ill or infected person lives, or if unknown, wherein the diagnosis is made. The health officer (or designee) must immediately institute the control measures listed below in section 6, “Controlling Further Spread,” regardless of weekend, holiday, or evening schedules. A directory of local health departments in New Jersey is available at http://www.state.nj.us/health/lh/directory/lhdselectcounty.shtml If the health officer is unavailable, the healthcare provider or administrator shall make the report to the Department by telephone to 609.826.5964, between 8:00 A.M. and 5:00 P.M. on non-holiday weekdays or to 609.392.2020 during all other days and hours. June 2019 Hepatitis A, Acute 1 THE DISEASE AND ITS EPIDEMIOLOGY A. Etiologic Agent Hepatitis A is caused by the hepatitis A virus (HAV), a ribonucleic acid (RNA) agent classified as a Picornavirus. There is only one serotype worldwide; it is slow-growing in living cells and resistant to heat, solvents, and acid. Depending on conditions, HAV can be stable in the environment for months. Heating foods at temperatures greater than 185°F (>85°C) for one minute or disinfecting surfaces with a 1:100 dilution of sodium hypochlorite (i.e., household bleach) in tap water is necessary to inactivate HAV. The major site of viral replication is in the liver. -

A Case of Pneumoperitoneum Secondary to Pneumatosis Intestinalis: Is Surgery Always Indicated?
Bahrain Medical Bulletin, Vol. 39, No. 2, June 2017 A Case of Pneumoperitoneum Secondary to Pneumatosis Intestinalis: Is Surgery Always Indicated? Lulwa Al Mannaei, MD* Essam Mazen Jumaa, Arab Board (Gen Surg)** Pneumatosis intestinalis (PI) is a rare condition, which could be associated with a spectrum of disorders that vary from mild to life-threatening. We report a case of an eighty-five-year-old male who presented with abdominal distension and vomiting. Examination revealed the presence of peritoneal signs, with abdominal and pelvic CT confirming PI of the small bowel, a relatively rare condition. The patient underwent an exploratory laparotomy, during which, a segment of the terminal ileum was resected and an ileostomy was fashioned. The patient, unfortunately, died one month postoperatively due to postoperative complications. This case demonstrates the need for risk stratification guidelines to decide conservative or surgical management in cases of PI in this age group. Bahrain Med Bull 2017; 39(2): 113 - 115 PI is the presence of multiple gas cysts in the walls of the The patient was a known case of hypertension, diabetes small and large intestines1. It could affect all ages and the mellitus type 2 and schizophrenia. He had been confined to bed estimated prevalence is 0.02% to 0.003% worldwide2. It could for some time. He had no past surgical history and no history be primary or secondary1. The latter is usually associated with of previous hospital admissions. higher mortality rates, whereas the former is mostly benign and often considered an incidental finding. Most patients are On examination, the patient was conscious; however, he was asymptomatic. -

Oxford American Handbook of Gastroenterology and Hepatology
Oxford American Handbook of Gastroenterology and Hepatology About the Oxford American Handbooks in Medicine The Oxford American Handbooks are pocket clinical books, providing practi- cal guidance in quick reference, note form. Titles cover major medical special- ties or cross-specialty topics and are aimed at students, residents, internists, family physicians, and practicing physicians within specifi c disciplines. Their reputation is built on including the best clinical information, com- plemented by hints, tips, and advice from the authors. Each one is carefully reviewed by senior subject experts, residents, and students to ensure that content refl ects the reality of day-to-day medical practice. Key series features • Written in short chunks, each topic is covered in a two-page spread to enable readers to fi nd information quickly. They are also perfect for test preparation and gaining a quick overview of a subject without scanning through unnecessary pages. • Content is evidence based and complemented by the expertise and judgment of experienced authors. • The Handbooks provide a humanistic approach to medicine – it’s more than just treatment by numbers. • A “friend in your pocket,” the Handbooks offer honest, reliable guidance about the diffi culties of practicing medicine and provide coverage of both the practice and art of medicine. • For quick reference, useful “everyday” information is included on the inside covers. Published and Forthcoming Oxford American Handbooks Oxford American Handbook of Clinical Medicine Oxford American Handbook -

FDA Warns About Rare Occurrence of Serious Liver Injury with Use of Hepatitis C Medicines Mavyret, Zepatier, and Vosevi in Some Patients with Advanced Liver Disease
FDA Drug Safety Communication FDA warns about rare occurrence of serious liver injury with use of hepatitis C medicines Mavyret, Zepatier, and Vosevi in some patients with advanced liver disease Safety Announcement [08-28-2019] The Food and Drug Administration (FDA) has received reports that the use of Mavyret, Zepatier, or Vosevi to treat chronic hepatitis C in patients with moderate to severe liver impairment has resulted in rare cases of worsening liver function or liver failure. All these medicines contain a hepatitis C virus (HCV) protease inhibitor and are not indicated for use in patients with moderate to severe liver impairment. In most patients, symptoms resolved or new onset worsening of liver function improved after stopping the medicine. These medicines have been widely used and are safe and effective in patients with no or mild liver impairment. In many of the reported cases, liver failure occurred in patients who had signs and symptoms of moderate to severe liver impairment (Child-Pugh B or C) or other serious liver problems and should not have been treated with these medicines. In some cases, patients were reported to have no cirrhosis or compensated cirrhosis with mild liver impairment (Child-Pugh A) despite having evidence of decreased platelets at baseline or an increase in the pressure within the portal vein that carries blood from the digestive organs to the liver. In addition, some cases had other significant pre-existing risk factors such as liver cancer, alcohol abuse, or serious medical illnesses associated with serious liver problems. These factors may have contributed to clinical worsening of liver function or liver failure during treatment with these hepatitis C medicines.