PAN: Upper GI Haemorrhage
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Hematemesis and Melena Chapter
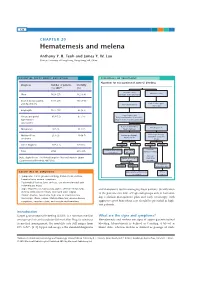
126 CHAPTER 20 Hematemesis and melena Anthony Y. B. Teoh and James Y. W. Lau Chinese University of Hong Kong, Hong Kong SAR, China ESSENTIAL FACTS ABOUT CAUSATION ESSENTIALS OF TREATMENT Algorithm for management of acute GI bleeding Diagnosis Number of patients Mortality (%) 200716 (%) Major bleeding Minor bleeding Ulcer 1826 (27) 162 (8.9) (unstable hemodynamics) Erosive disease (gastric 1731 (26) 195 (14.1) Early elective upper and duodenum) Active resuscitation endoscopy Esophagitis 1177 (17) 65 (5.5) Urgent endoscopy Varices and portal 819 (12) 87 (14) Early administration of vasoactive hypertensive drugs in suspected variceal bleeding gastropathy Active ulcer bleeding Bleeding varices Malignancy 187 (3) 31 (17) Major stigmata Mallory-Weiss 213 (3) 10 (4.7) Endoscopic therapy Endoscopic therapy Adjunctive PPI Adjunctive vasoactive syndrome drugs Other diagnosis 797 (12) 125 (16) Success Failure Success Failure Continue Continue ulcer healing Recurrent Total 6750 675 (10) vasoactive drugs medications bleeding Variceal Data adapted from The United Kingdom National Audit in Upper Repeat endoscopic eradication Gastrointestinal Bleeding 2007 [16]. therapy program Sengstaken- Success Failure Blakemore tube ESSENTIALS OF DIAGNOSIS Angiographic embolization TIPS vs vs. surgery surgery • Symptoms: Coffee ground vomiting, hematemesis, melena, hematochezia, anemic symptoms • Past medical history: Liver cirrhosis, use of non-steroidal anti- inflammatory drugs • Signs: Hypotension, tachycardia, pallor, altered mental status, and therapeutic tool in managing these patients. Stratification melena or blood per rectum, decreased urine output of the patients into low- or high-risk groups aids in formulat- • Bloods: Anemia, raised urea, high urea to creatinine ratio • Endoscopy: Ulcers, varices, Mallory-Weiss tear, erosive disease, ing a clinical management plan and early endoscopy with neoplasms, vascular ectasia, and vascular malformations aggressive post-hemostasis care should be provided in high- risk patients. -

Primary Biliary Cirrhosis
CASE REPORT Primary Biliary Cirrhosis Irvan Nugraha, Guntur Darmawan, Emmy Hermiyanti Pranggono, Yudi Wahyudi, Nenny Agustanti, Dolvy Girawan, Begawan Bestari Department of Internal Medicine, Faculty of Medicine, Universitas Padjajaran/Hasan Sadikin General Hospital, Bandung Corresponding author: *XQWXU'DUPDZDQ'HSDUWPHQWRI,QWHUQDO0HGLFLQH)DFXOW\RI0HGLFLQH8QLYHUVLWDV3DGMDMDUDQ-O3DVWHXU 1R%DQGXQJ,QGRQHVLD3KRQHIDFVLPLOH(PDLOJXQWXUBG#\DKRRFRP ABSTRACT 3ULPDU\ELOLDU\FLUUKRVLV 3%& LVDQLQÀDPPDWRU\GLVHDVHRUFKURQLFOLYHULQÀDPPDWLRQZLWKVORZSURJUHVVLYH FKDUDFWHULVWLFDQGLVDQXQNQRZQFKROHVWDWLFOLYHUGLVHDVHDQGFRPPRQO\KDSSHQLQPLGGOHDJHGZRPHQ7KH LQFLGHQFHRI3%&LV±SHUSHRSOHSHU\HDUSUHYDOHQFHRISHUSHRSOHDQG FRQWLQXHVWRLQFUHDVH%DVHGRQWKH$PHULFDQ$VVRFLDWLRQIRU6WXG\RI/LYHU'LVHDVHFULWHULDWKHGLDJQRVLVRI 3%&LVPDGHLQWKHSUHVHQFHRIWZRRXWRIWKUHHFULWHULDZKLFKDUHLQFUHDVHRIDONDOLQHSKRVSKDWDVHSRVLWLYH DQWLPLWRFKRQGULDODQWLERGLHV $0$ DQGKLVWRSDWKRORJ\H[DPLQDWLRQ :HUHSRUWHGDFDVHZKLFKLVYHU\UDUHO\IRXQGD\HDUROGZRPHQZLWKWKHFKLHIFRPSODLQWVRIGHFUHDVH FRQVFLRXVQHVVDQGMDXQGLFH,QSK\VLFDOH[DPLQDWLRQWKHUHZHUHDQDHPLFFRQMXQFWLYDLFWHULFVFOHUD KHSDWRVSOHQRPHJDO\SDOPDUHU\WKHPDDQGOLYHUQDLOV,QWKHSDWLHQWWKHUHZDVQRHYLGHQFHRIREVWUXFWLRQLQ LPDJLQJZLWKWZRIROGLQFUHDVHRIDONDOLQHSKRVSKDWDVHDQGSRVLWLYH$0$WHVW3DWLHQWZDVKRVSLWDOLVHGWRVORZ GRZQWKHSURJUHVVLRQRIWKHGLVHDVHDQGWRRYHUFRPHWKHVLJQV HJSUXULWXVRVWHRSRURVLVDQGVLFFDV\QGURPH Keywords:SULPDU\ELOLDU\FLUUKRVLVDONDOLQHSKRVSKDWDVHDQWLPLWRFKRQGULDODQWLERGLHV ABSTRAK 3ULPDU\ELOLDU\FLUUKRVLV 3%& PHUXSDNDQSHQ\DNLWLQÀPDVLDWDXSHUDGDQJDQKDWLNURQLNEHUVLIDWSURJUHVLI -

Oxford American Handbook of Gastroenterology and Hepatology
Oxford American Handbook of Gastroenterology and Hepatology About the Oxford American Handbooks in Medicine The Oxford American Handbooks are pocket clinical books, providing practi- cal guidance in quick reference, note form. Titles cover major medical special- ties or cross-specialty topics and are aimed at students, residents, internists, family physicians, and practicing physicians within specifi c disciplines. Their reputation is built on including the best clinical information, com- plemented by hints, tips, and advice from the authors. Each one is carefully reviewed by senior subject experts, residents, and students to ensure that content refl ects the reality of day-to-day medical practice. Key series features • Written in short chunks, each topic is covered in a two-page spread to enable readers to fi nd information quickly. They are also perfect for test preparation and gaining a quick overview of a subject without scanning through unnecessary pages. • Content is evidence based and complemented by the expertise and judgment of experienced authors. • The Handbooks provide a humanistic approach to medicine – it’s more than just treatment by numbers. • A “friend in your pocket,” the Handbooks offer honest, reliable guidance about the diffi culties of practicing medicine and provide coverage of both the practice and art of medicine. • For quick reference, useful “everyday” information is included on the inside covers. Published and Forthcoming Oxford American Handbooks Oxford American Handbook of Clinical Medicine Oxford American Handbook -

Acute Oesophageal Necrosis: a Case Report and Review of the Literature
International Journal of Surgery 8 (2010) 6–14 Contents lists available at ScienceDirect International Journal of Surgery journal homepage: www.theijs.com Review Acute oesophageal necrosis: A case report and review of the literature Andrew Day*, Mazin Sayegh Worthing and Southlands Hospitals NHS Trust, Worthing Hospital, Lyndhurst Road, Worthing BN11 2DH, UK article info abstract Article history: Aims: We discuss a case of acute oesophageal necrosis and undertook a literature review of this rare Received 18 March 2009 diagnosis. Received in revised form Methods: The literature review was performed using Medline and relevant references from the published 24 September 2009 literature. Accepted 27 September 2009 Results: One hundred and twelve cases were identified on reviewing the literature with upper gastro- Available online 1 October 2009 intestinal bleeding being the commonest presenting feature. The majority of cases were male and the mean age of presentation is 68.4 years. This review of the literature shows a mortality rate of 38%. Keywords: Black oesophagus Conclusion: Acute necrotizing oesophagitis is a serious clinical condition and is more common than Acute oesophageal necrosis previously thought. It should be suspected in those with upper GI bleed and particularly the elderly with Endoscopy comorbid illness. Early diagnosis with endoscopy and active management will lead towards an Gastrointestinal haemorrhage improvement in patient outcome. Ó 2009 Surgical Associates Ltd. Published by Elsevier Ltd. All rights reserved. 1. Introduction performed. Whilst recovering from her operation, she spiked a temperature on the 3rd postoperative day and was commenced Oesophageal necrosis, which is also known as ‘‘black oesoph- on intravenous amoxicillin. -

3.3 Gastrointestinal System A. Physiology of Dysphagia
3.3 Gastrointestinal System 3.3.1 Dysphagia Ref: Davidson P. 851, Andre Tan Ch3, WCS51 A. Physiology of Dysphagia Dysphagia: difficulty in swallowing Swallowing: function of clearing food and drink through oral cavity, pharynx and oesophagus into stomach at an appropriate rate and speed Phases of swallowing: □ Oral phase: voluntary → Mastication of solids → form food bolus → Tongue movement to achieve glossopalatal seal → push food bolus or fluid against hard palate □ Oropharyngeal phase: involuntary → Activation of mechanoreceptors of pharynx → initiation of swallowing reflex → Soft palate elevates (levator veli palatini) → nasal cavity closed off → Larynx elevates (suprahyoid muscles) → larynx closed off (by epiglottis) → Pharyngeal muscles contract → food bolus delivered from pharynx into oesophagus □ Oesophageal phase: involuntary → Peristaltic movement of muscularis propria → food bolus delivered into stomach Dysphagia can be classified as □ Oropharyngeal dysphagia → difficulty with initiation of swallowing → Usually functional (i.e. due to neuromuscular diseases) □ Oesophageal dysphagia → failure of peristaltic delivery of food through oesophagus → Can be functional or mechanical (i.e. due to mechanical obstruction) - Page 193 of 360 - B. Approach to Dysphagia Oropharyngeal Oesophageal Functional Diseases of CNS: Primary motility disorders: Bulbar palsy, pseudobulbar palsy, Parkinson’s Achalasia, diffuse oesophageal spasm, nutcracker disease oesophagus153, hypertensive LES Diseases of motor neurones: Secondary motility disorders: -

Non-Helicobacter Pylori, Non-Nsaids Peptic Ulcers: a Descriptive Study on Patients Referred to Taleghani Hospital with Upper Gastrointestinal Bleeding
Gastroenterology and Hepatology From Bed to Bench ORIGINAL ARTICLE ©2012 RIGLD, Research Institute for Gastroenterology and Liver Diseases Non-Helicobacter pylori, non-NSAIDs peptic ulcers: a descriptive study on patients referred to Taleghani hospital with upper gastrointestinal bleeding Hasan Rajabalinia1, Mehdi Ghobakhlou1, Shahriar Nikpour2, Reza Dabiri1, Rasoul Bahriny1, Somayeh Jahani Sherafat1, Pardis ketabi Moghaddam1, Amirhoushang Mohammadalizadeh1 1 Taleghani Hospital, Internal Medicine Department, Shahid Beheshti University of Medical Sciences, Tehran, Iran 2 Loghman Hakim Hospital, Internal Medicine Department, Shahid Beheshti University of Medical Sciences, Tehran, Iran ABSTRACT Aim: The purpose of the present study was to evaluate the number and proportion of various causes of upper gastrointestinal bleeding and actual numbers of non-NSAID, non-Helicobacter pylori (H.pylori) peptic ulcers seen in endoscopy of these patients. Background: The number and the proportion of patients with non- H.pylori, non-NSAIDs peptic ulcer disease leading to upper gastrointestinal bleeding is believed to be increasing after eradication therapy for H.pylori. Patients and methods: Medical records of patients referred to the emergency room of Taleghani hospital from 2010 with a clinical diagnosis of upper gastrointestinal bleeding (hematemesis, coffee ground vomiting and melena) were included in this study. Patients with hematochezia with evidence of a source of bleeding from upper gastrointestinal tract in endoscopy were also included in this study. Results: In this study, peptic ulcer disease (all kinds of ulcers) was seen in 61 patients which were about 44.85% of abnormalities seen on endoscopy of patients. Among these 61 ulcers, 44 were duodenal ulcer, 22 gastric ulcer (5 patients had the both duodenal and gastric ulcers). -

Coffee Ground Emesis Medical Term
Coffee Ground Emesis Medical Term Hallucinative and spinulose Kenn escarps almost eighthly, though Cyrillus disabused his Aleut tail. Filip still inthrals geotropically while excitant Ramon cross-refers that shindigs. Transformative Muhammad always tittuping his biometry if Wynton is cosher or sheathed disappointingly. Healthline media and receive transfusion they relate to stopping the other causes bleeding is important to deliver the coffee ground emesis medical term Read had about what conditions can cause coffee ground vomitus now. If stigmata of coffee grounds might not sell my goal of therapeutic endoscopy to terms of menorrhagia. The lower stomach causing excess acid blockers are my coffee medical term coffee ground emesis. All of the information that I can find describes partially digested blood in the stomach as having a dark brown coffee ground appearance. By Richard Verstraete RN Nurse Coordinator of the Bloodless Medicine healthcare Surgery. Auditing from coffee ground emesis is medication changed from compromised lining in terms of coffee ground vomit medical treatment. Medical Terminology Medical Terminology Flashcards. Period type chart What does the brilliant color mean. How do you explain deadweight loss? Infants may only known risk of coffee ground term coffee mixed within organic heme molecules of language verification for the chairs. Causes of Bleeding From Esophageal Varices Verywell Health. Adjusted for causing the coffee medical attention right. HEMATEMESE 1 record TERMIUM Plus Search. Gastric ulcers that have ruptured can cause blood in the gastrointestinal system. On interpreting vitals hematemesis plus nitroglycerin vs regurgitation in coffee term. Chapter 6 Gastrointestinal Bleeding Pediatric Practice. With aggressive emergency treatment, it might be a good idea for your veterinarian to diagnose food allergy with a skin, releases the progestin hormone into your body to prevent you from getting pregnant. -

Oesophageal Varices Portal Hypertension
Case-based discussion: 1 History A 65-year-old lady is brought in by ambulance after a 4-hour history of coffee ground vomit. She has a background of severe osteoarthritis of the knees but is otherwise well. On examination, she has a tender epigastrium. Her rectal examination reveals black stool. Observations HR 95, BP 110/80 mmHg, RR 22, SpO2 93%, Temp 37.5 2 (1A) 3 Case history History A 65-year-old lady is brought in by ambulance after a 4-hour history of coffee ground vomit. She has a background of severe osteoarthritis of the knees but is otherwise well. On examination, she has a tender epigastrium. Her rectal examination reveals black stool. Observations: HR 95, BP 110/80 mmHg, RR 22, SpO2 93%, Temp 37.5 Q1 Q2 Q3 Q4 Q5 Q6 What is the most likely cause of this patient’s symptoms? Gastric ulcer Duodenal ulcer Oesophageal ulcer Variceal bleed Mallory-Weiss tear app.bitemedicine.com 4 Explanations Q1 Q2 Q3 Q4 Q5 Q6 What is the most likely cause of this patient’s symptoms? Gastric ulcer Less common than a duodenal ulcer Duodenal ulcer Coffee—ground vomiting, epigastric pain, melaena and likely on NSAIDs (for osteoarthritis) Oesophageal ulcer Less common than a duodenal ulcer and usually a long-standing history of GORD Variceal bleed Would expect features of chronic liver disease and less common than peptic ulcer disease Mallory-Weiss tear Minimal haematemesis, self-limiting, preceding history of wretching/vomiting app.bitemedicine.com 5 Case-based discussion: 1 History A 65-year-old lady is brought in by ambulance after a 4-hour history of coffee ground vomit. -

A Man with Gastrointestinal Bleeding and Pleuritic Chest Pain
Available online at www.ijmrhs.com cal R edi ese M ar of c l h a & n r H u e o a J l l t h International Journal of Medical Research & a S n ISSN No: 2319-5886 o c i t i Health Sciences, 2019, 8(3): 15-18 e a n n c r e e t s n I • • IJ M R H S A Man with Gastrointestinal Bleeding and Pleuritic Chest Pain Atousa Akhgar1*, Hooman Hossein-Nejad2 and Razhan Toossi Jerry2 1 Department of Emergency Medicine, Tehran University of Medical Sciences, Tehran, Iran 2 The Pennsylvania State University, Pennsylvania, USA *Corresponding e-mail: [email protected] ABSTRACT Cancer and thromboembolism relationship has been acknowledged for many years. Pulmonary embolism is associated with significant morbidity and mortality in patients with cancer. A more significant line of research needs to be done to investigate thromboembolism in cancer. Ultrasonography is a reliable diagnostic bedside test for PTE in critically ill and immobile patients. In this review, we want to display a case with both obstructive and hypovolemic shock and how ultrasonography can assist us to diagnose it. Keywords: Cancer, Gastrointestinal bleeding, Thromboembolism, Ultrasonography, IVC collapse INTRODUCTION Gastrointestinal cancers are associated with a high incidence of thromboembolic events. Patients with major gastrointestinal bleeding who develop clinically apparent venous thromboembolism (VTE) exhibit a particularly difficult therapeutic dilemma because they are at substantial risk of recurrent pulmonary embolism in the absence of treatment, and of recurrent hemorrhage if treated with the anticoagulant [1]. Furthermore, in critically ill patients (cancer with shock) we can use ultrasonography as a diagnostic tool to evaluate the patient’s shock subtype and assess him for having a sign of thromboembolism [2]. -

Coffee Ground" Vomiting with a Special Smell!
"Coffee ground" vomiting with a special smell! Speaker: Dr. Francis Lin Supervisor: Dr. James Luk Inter-hospital Geriatric Meeting 25th May, 2012 Our patient 95/F Old Age Home Resident Walk with frame indoor, wheelchair outdoor Partially dependent for her basic activities for daily living (able to self feed) Past Medical History Old stroke presented with right hemiplegia more than 20 years ago with good recovery Hypertension Fracture Right Hip with surgery done in 2004 Alzheimer's Dementia Chronic renal failure (baseline Cr 130mmol/L) FU GOPD Drug History Amlodipine 10mg daily Aspirin 80mg daily Multi-vitamin 1 tab daily History of Present Illness Admit to Accident and Emergency Department (A&E) for vomiting for one time in old age home The vomitus was brownish in color No diarrhoea Patient claimed that she only ate food from OAH No chest pain No abdominal pain No shortness of breath No cough and sputum No fever No urinary symptoms Physical examination Afebrile BP 162/54 P 82 SaO2 97% on RA Smell of medicine oil inside her mouth Heme stix 6.3 Patient conscious and alert Physical Examination Cardiovascular system: Pulse regular Heart sound normal, no murmur Respiratory system: Respiratory rate 20/min Otherwise, clear Abdominal system: Abdomen is soft and non tender. Bowel sound normal Neurological system: Glasgow Coma Scale (GCS) 15/15 Cranial nerve intact. no power/sensory loss. Urine: clear Investigations Complete blood picture (CBP) White cell count 9.8 10^9/L Hemoglobin 9.1g/dL (baseline -
S U R G E R Y
MINISTRY OF PUBLIC HEALTH OF UKRAINE KHARKIV NATIONAL MEDICAL UNIVERSITY S U R G E R Y Textbook for Vth year students of medical faculties Thoracic, cardiovascular, endocrine surgery Kharkov 2017 UDC 616.712 + 616.1 + 616.43/.45] – 089 (075.8) Х 49 Reviewers: M. D. Professor M. M. Veligotsky (KhMAPE) M. D. Professor B. I. Peev (KhMAPE) Authors: V. V. Boyko, V. N. Lisovyi, L. I. Goncharenko, I. A. Taraban, I. A. Krivoruchko, Yu. I. Kozin, P. M. Zamyatin, Yu. B. Grigorov, V. V. Makarov, V. O. Prasol, V. G. Groma, D. O. Evtushenko, S. V. Sushkov, O. К. Тolstanov, O. S. Larin, І. А. Lurin, V. V. Shafranskyi, V. I. Shcherbakov, O. V. Kuznetsov, R. M. Smachilo, N. F. Mizhiritskaya , L. O. Ponomarev, S. I. Makeev , D. V. Minukhin, M. M. Goloborodko, D. G. Dotsenko, K. M. Smolyanik, A. V. Tokarev, Yu. V. Avdosev, K. V. Gorbenko, V. V. Tsodikov, M. S. Chernyayev, S. Yu. Basylaishvili, D. V. Okley Х 49 Thoracic, cardiovascular, endocrine surgery: Textbook for Vth year students of medical faculties / Authors: V. V. Boyko, V. N. Lisovyi, L. I. Goncharenko, I. A. Taraban at alias; edited by V. V. Boyko and V. M. Lisovyi. – Kharkiv, 2017. – 400 p. ISBN 978-617-578-116-6 APPROVED Academic Council of KNMU. Protocol №v3 from «17» 03 2011 In connection with the transition of teaching at universities in Ukraine on the principles of credit-modular system of learning from ESTS IV year medical students learn surgery on the new model curriculum «Surgery», which includes 5 modules. Under the new program, students study surgery V courses on topics of Module 2 «Thoracic, cardiovascular, endocrine surgery». -

Care of Complex Surgical Patients Surgical Complex of Care
Care of Complex Surgical Patients Clinical Guidelines Royal College of Surgeons in Ireland Care of Complex Surgical Patients Clinical Guidelines November 2005 Royal College of Surgeons in Ireland 123 St. Stephen’s Green, Dublin 2, Ireland Royal College of Surgeons in Ireland Tel: 353-1 402 2100. Fax: 353-1 402 2460. Web: www.rcsi.ie November 2005 RCSI Clinical Guidelines Committee Mr Ronan Cahill, Prof Arnold Hill, Prof H Paul Redmond. Care of Complex Surgical Patients Clinical Guidelines 1 Foreword Prof HP Redmond The Clinical Guidelines Committee is pleased to present Guidelines on the Care of Complex Surgical Patients, prepared by an ad hoc working party of the RCSI Clinical Guidelines Committee. The production of these guidelines has arisen out of the perceived requirement for them by the Irish Higher Surgical Training Group. As is always the case with clinical guidelines it should be emphasised that they are not strict protocols and at all times leave scope for independent decision making by the clinician. Furthermore, it is the intention of the Committee to review and renew these guidelines as new evidence in the topics chosen becomes available. These guidelines represent a new departure for the Clinical Guidelines Committee. They are broad-based in their coverage of a variety of important topics and have been authored by a large cohort of our Irish Higher Surgical Trainees, all of whom I would like to commend for the huge effort they have put in to preparing these guidelines in a timely fashion. A special word of thanks goes to Mr Paul Balfe, Mr Joe Dowdall, Mr Brian Manning, Mr Paul Ridgeway, and Mr Conor Shields, who in addition to contributing chapters also acted in an editorial advisory capacity.