Therapeutic Class Overview Erythropoiesis-Stimulating Agents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Specialty Drug List 10-22-12 Final
Iowa Medicaid Specialty Drug List Effective 10/22/2012 “Specialty” drugs include biological drugs, blood-derived products, complex molecules, and select oral, injectable, and infused medications identified by the Department and reimbursed at AWP-17% plus the dispensing fee. Specialty pricing will be applied to both the brand and generic drug products. NOTE: See the PDL at www.iowamedicaidpdl.com for specific PA criteria for the following drugs. BRAND NAME GENERIC NAME AGENTS FOR GAUCHER DISEASE ELELYSO taliglucerase alfa VPRIV velaglucerase alfa ALS RILUTEK riluzole ALCOHOL DEPENDENCE VIVITROL naltrexone AMINOGLYCOSIDES TOBI tobramycin ANTI-ASTHMATICS ALPHA PROTEINASE INHIBITORS ARALAST proteinase inhibitor ARALAST NP proteinase inhibitor PROLASTIN, C proteinase inhibitor ZEMAIRA alpha-1 proteinase inhibitor ANTIASTHMATIC - BETA - ADRENERGICS BRETHINE INJECTION turbutaline sulfate ANTIASTHMATIC - HYDRO-LYTIC ENZYMES KALYDECO ivacaftor ANTIBIOTICS - MISC. CAYSTON aztreonam lysine for inhal soln ANTI-CATAPLECTIC AGENTS XYREM sodium oxybate oral solution ANTICOAGULANTS ARIXTRA fondaparinux sodium FRAGMIN dalteparin sodium INNOHEP tinzaparin sodium LOVENOX enoxaparin sodium ANTICONVULSANTS SABRIL vigabatrin ANTIDOTES FERRIPROX deferiprone ANTIDOTES - CHELATING AGENTS CHEMET succimer EXJADE deferasirox tab for oral susp Page 1 of 10 ANTIEMETIC - TETRAHYDROCANNABINOL (THC) DERIVATIVES MARINOL dronabinol ANTIFUNGALS - ASSORTED AMBISOME amphotericin B Liposome IV for suspension ANCOBON flucytosine CANCIDAS caspofungin acetate for IV solution -

Myelodysplastic Syndromes
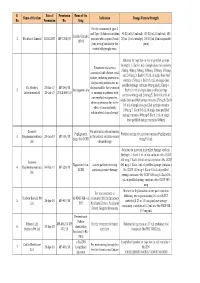
MYELODYSPLASTIC SYNDROMES TREATMENT REGIMENS (Part 1 of 3) Clinical Trials: The National Comprehensive Cancer Network recommends cancer patient participation in clinical trials as the gold standard for treatment. Cancer therapy selection, dosing, administration, and the management of related adverse events can be a complex process that should be handled by an experienced healthcare team. Clinicians must choose and verify treatment options based on the individual patient; drug dose modifications and supportive care interventions should be administered accordingly. The cancer treatment regimens below may include both U.S. Food and Drug Administration-approved and unapproved indications/regimens. These regimens are only provided to supplement the latest treatment strategies. These Guidelines are a work in progress that may be refined as often as new significant data becomes available. The NCCN Guidelines® are a consensus statement of its authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult any NCCN Guidelines® is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient’s care or treatment. The NCCN makes no warranties of any kind whatsoever regarding their content, use, or application and disclaims any responsibility for their application or use in any way. First-Line Treatment1 Note: All recommendations are Category 2A unless otherwise indicated. Relatively Lower-Risk Patientsa,b Symptomatic Anemia With del(5q) ± One Other Cytogenetic Abnormality (except those involving chromosome 7) REGIMEN DOSING Lenalidomide2-5,c Days 1–21: Lenalidomide 10mg orally once daily. Repeat cycle every 28 days (or 28 days monthly). Assess response 2–4 months after initiation of treatment. -

Specialty Drug Benefit Document
Louisiana Healthcare Connections Specialty Drug Benefit ouisiana Healthcare Connections provides coverage of a number of specialty drugs. All specialty drugs, such as biopharmaceuticals and injectables, require a prior authorization (PA) to be approved for L payment by Louisiana Healthcare Connections. PA requirements are programmed specific to the drug. Since the list of specialty drugs changes over time due to new drug arrivals and other market conditions, it is important to contact Provider Services at 1-866-595-8133 or check the Louisiana Healthcare Connections website at www.LouisianaHealthConnect.com for updates to this benefit. Requests for specialty drugs can be submitted to Louisiana Healthcare Connections by filling out the Medication Prior Authorization Form that is available on the Louisiana Healthcare Connections website at www.LouisianaHealthConnect.com and faxing the request as instructed on the form. Louisiana Healthcare Connections members can receive the specialty drugs they require at any outpatient pharmacy enrolled in our pharmacy network that can supply specialty drugs. Providers that wish to have drugs distributed by a SPECIALTY PHARMACY should FAX the request to 1-866-399-0929 for review. If a provider wishes to dispense a specialty drug from OFFICE STOCK, the provider should FAX the request to Louisiana Healthcare Connections at 1-877-401-8172 for review. BRAND NAME INGREDIENTS SPECIAL INSTRUCTIONS ACTEMRA TOCILIZUMAB ACTHAR HP CORTICOTROPIN ACTIMMUNE INTERFERON GAMMA-1B ADAGEN PEGADEMASE BOVINE Limited Distribution -

MSM Chapter 1200 3/1/21
MEDICAID SERVICES MANUAL TRANSMITTAL LETTER February 23, 2021 TO: CUSTODIANS OF MEDICAID SERVICES MANUAL FROM: JESSICA KEMMERER, HIPAA PRIVACY AND CIVIL RIGHTS OFFICER /Jessica Kemmerer/ BACKGROUND AND EXPLANATION The DHCFP is proposing revisions to Medicaid Services Manual (MSM), Chapter 1200 – Prescribed Drugs, Appendix A, to reflect recommendations approved on October 22, 2020, by the Drug Use Review (DUR) Board. The proposed changes include the addition of new prior authorization criteria for Doxepine Topical, the addition of new prior authorization criteria for Zeposia® (ozanimod), addition of new prior authorization for Evenity® (romosozumab-aqqg), Prolia® (denosumab), Forteo® (teriparatide) and Tymlos® (abaloparatide) within a new combined osteoporosis agents section, and addition of new prior authorization criteria for Orilissa® (elagolix) and Oriahnn® (elagolix, estradiol, and norethindrone) within a new Gonadorpin Hormone Receptor (GnRH) Antagonist and Combinations section. Additionally, the DHCFP is proposing revisions to the existing prior authorization criteria for psychotropic medications for children and adolescents, and revision to the existing clinical criteria for Epidiolex® (cannabidiol). Throughout the chapter, grammar, punctuation and capitalization changes were made, duplications removed, acronyms used and standardized, and language reworded for clarity. Renumbering and re- arranging of sections was necessary. These changes are effective March 1, 2021. MATERIAL TRANSMITTED MATERIAL SUPERSEDED MTL N/A MTL N/A MSM Ch 1200 – Prescribed Drugs MSM Ch 1200 – Prescribed Drugs Background and Explanation of Policy Changes, Manual Section Section Title Clarifications and Updates Appendix A Psychotropic Added new policy language criteria on which specific Section N Medications for drug classes may bypass polypharmacy clinical criteria. Children and Adolescents Appendix A Reserved for Future Created a new section titled “Doxepin Topical.” Added Section W Use new prior authorization criteria for doxepin topical. -

OMONTYS® Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION ---------------------DOSAGE FORMS AND STRENGTHS---------------------- These highlights do not include all the information needed to use Dosage Form Strengths OMONTYS® safely and effectively. See full prescribing information for OMONTYS. Single use vials 2 mg/0.5 mL, 3 mg/0.5 mL, (preservative-free) 4 mg/0.5 mL, 5 mg/0.5 mL, and OMONTYS® (peginesatide) Injection, 6 mg/0.5 mL for intravenous or subcutaneous use Single use pre-filled syringes 1 mg/0.5 mL, 2 mg/0.5 mL, Initial U.S. Approval: 2012 (preservative-free) 3 mg/0.5 mL, 4 mg/0.5 mL, 5 mg/0.5 mL, and 6 mg/0.5 mL WARNING: ESAs INCREASE THE RISK OF DEATH, MYOCARDIAL Multiple use vials 10 mg/mL and 20 mg/2 mL INFARCTION, STROKE, VENOUS THROMBOEMBOLISM, (with preservative) THROMBOSIS OF VASCULAR ACCESS AND TUMOR PROGRESSION OR RECURRENCE -------------------------------CONTRAINDICATIONS------------------------------ See full prescribing information for complete boxed warning. Uncontrolled hypertension (4). Chronic Kidney Disease: In controlled trials, patients experienced greater risks for -----------------------WARNINGS AND PRECAUTIONS------------------------ death, serious adverse cardiovascular reactions, and stroke Increased Mortality, Myocardial Infarction, Stroke, and when administered erythropoiesis-stimulating agents (ESAs) Thromboembolism: Using ESAs to target a hemoglobin level of to target a hemoglobin level of greater than 11 g/dL (5.1). greater than 11 g/dL increases the risk of serious adverse No trial has identified a hemoglobin target level, ESA dose, or cardiovascular reactions and has not been shown to provide dosing strategy that does not increase these risks (5.1). additional benefits (5.1). -
Final List of R-DNA Based Drugs Approved in the Country.Xlsx
S. Date of Permission Name of the Name of the firm Indication Dosage Form & Strength No. Permission No. Drug For the treatment of type -I and Type -II diabetes mellitus 40 IU/ml (10 ml vial), 100 IU/ml (10 ml vial), 100 Insulin Glargine 1 Wockhardt Limited 22.02.2007 MF-7206/07 patients who required basal IU/ml (3 ml cartridge), 100 IU/ml (3 ml disposable 100 IU (long acting) insulin for the pens) control of hyperglycemia. Solution for injection in vial or prefilled syringe Strength: 1. Each 1 mL of single dose vial contains Treatment of anaemia 25mcg, 40mcg, 60mcg, 100mcg, 200mcg, 300mcg associated with chronic renal and 500mcg 2. Each 0.75 mL of single dose vial failure, including patients on contains 150mcg 3. Each 0.3 mL of single dose dialysis and patients not on prefilled syringe contains 60mcg and 150mcg 4. Dr. Reddy's 23-Mar-10 MF-246/10 dialysis and for the treatment 2 Darbepoetin alfa Each 0.4 mL of single dose prefilled syringe Laboratories Ltd. 20-Jul-10 BULK-668/10 of anaemia in patients with contains 40mcg and 200mcg 5. Each 0.42 mL of non-myeloid malignancies, single dose prefilled syringe contains 25mcg 6. Each where anaemia is due to the 0.5 mL of single dose prefilled syringe contains effect of concomitantly 100mcg 7. Each 0.6 mL of single dose prefilled administered chemotherapy syringe contains 300mcg 8. Each 1 mL of single dose prefilled syringe contains 500mcg Gennova For prevention of neutropenia Pegfilgrastim Prefilled syringe for injection contains Pegfilgrastim 3 Biopharmaceuticals 29-Jan-10 MF-104/10 in the patient receiving cancer (peg-r-hu-GCSF) 6 mg/0.6 mL Ltd. -

Overview of Antibody Drug Delivery
pharmaceutics Review Overview of Antibody Drug Delivery Sahar Awwad 1,2,* ID and Ukrit Angkawinitwong 1 1 UCL School of Pharmacy, London WC1N 1AX, UK; [email protected] 2 National Institute for Health Research (NIHR) Biomedical Research Centre at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology, London EC1 V9EL, UK * Correspondence: [email protected]; Tel.: +44-207-753-5802 Received: 27 March 2018; Accepted: 29 June 2018; Published: 4 July 2018 Abstract: Monoclonal antibodies (mAbs) are one of the most important classes of therapeutic proteins, which are used to treat a wide number of diseases (e.g., oncology, inflammation and autoimmune diseases). Monoclonal antibody technologies are continuing to evolve to develop medicines with increasingly improved safety profiles, with the identification of new drug targets being one key barrier for new antibody development. There are many opportunities for developing antibody formulations for better patient compliance, cost savings and lifecycle management, e.g., subcutaneous formulations. However, mAb-based medicines also have limitations that impact their clinical use; the most prominent challenges are their short pharmacokinetic properties and stability issues during manufacturing, transport and storage that can lead to aggregation and protein denaturation. The development of long acting protein formulations must maintain protein stability and be able to deliver a large enough dose over a prolonged period. Many strategies are being pursued to improve the formulation and dosage forms of antibodies to improve efficacy and to increase the range of applications for the clinical use of mAbs. Keywords: antibodies; protein; pharmacokinetics; drug delivery; stability 1. -
Presentation Title
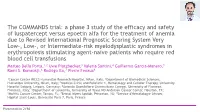
The COMMANDS trial: a phase 3 study of the efficacy and safety of luspatercept versus epoetin alfa for the treatment of anemia due to Revised International Prognostic Scoring System Very Low-, Low-, or Intermediate-risk myelodysplastic syndromes in erythropoiesis stimulating agent-naive patients who require red blood cell transfusions Matteo Della Porta,1,2 Uwe Platzbecker,3 Valeria Santini,4 Guillermo Garcia-Manero,5 Rami S. Komrokji,6 Rodrigo Ito,7 Pierre Fenaux8 1Cancer Center IRCCS Humanitas Research Hospital, Milan, Italy; 2Department of Biomedical Sciences, Humanitas University, Milan, Italy; 3Medical Clinic and Policlinic 1, Hematology and Cellular Therapy, University Hospital Leipzig, Leipzig, Germany; 4Azienda Ospedaliero-Universitaria Careggi, University of Florence, Florence, Italy; 5Department of Leukemia, University of Texas MD Anderson Cancer Center, Houston, TX; 6Moffitt Cancer Center, Tampa, FL; 7Bristol Myers Squibb, Princeton, NJ; 8Service d'Hématologie Séniors, Hôpital Saint-Louis, Université Paris 7, Paris, France Presentation 2198 Presenting author disclosures M.D.P.: no conflicts of interest to disclose. 2 Introduction and objectives Introduction • Studies of epoetin alfa and darbepoetin alfa have demonstrated efficacy among patients with LR-MDS, but the patient population in which a clinically significant effect is observed may be limited1,2 • Luspatercept, a first-in-class erythroid maturation agent with a mechanism of action distinct from ESAs,3 is approved by the US FDA for the treatment of anemia failing an -

Peginesatide for Anaemia in Chronic Kidney Disease – First and Second Line
Peginesatide for anaemia in chronic kidney disease – first and second line June 2012 This technology summary is based on information available at the time of research and a limited literature search. It is not intended to be a definitive statement on the safety, efficacy or effectiveness of the health technology covered and should not be used for commercial purposes. The NIHR Horizon Scanning Centre Research Programme is part of the National Institute for Health Research www.nhsc-healthhorizons.org.uk June 2012 Peginesatide for anaemia in chronic kidney disease – first and second line Target group • Symptomatic anaemia: patients on dialysis with chronic kidney disease (CKD) – first and second line. Background Human erythropoietin (EPO) is a protein produced by the kidneys that stimulates the production of red blood cells. Because the kidney is the sole source of EPO synthesis in adults, the reduction in kidney mass that occurs in progressive CKD often causes impairment of EPO production, resulting in anaemia. Technology description Peginesatide (AF-37702) is a synthetic peptide mimetic of EPO that binds directly to the erythropoietin receptor on red blood cell precursors to stimulate red cell formation. Peginesatide is intended as a substitute for currently available erythropoiesis stimulating agents (ESAs) in the treatment of anaemia in CKD dialysis patients. It is administered intravenously (IV) or subcutaneously (SC) at 0.04 mg/kg once monthly. After the initial dose, doses may be titrated to achieve a haemoglobin (Hb) level in the range of 10 to 12g/dL. Peginesatide is also in phase II clinical trials for pure red cell aplasia. -

Pipelinetr Ends
June 2011 PIPELINE TRxENDS PIPELINE TR ENDS is produced by the x 1-3 Promising New Agents 5 Industry Trends University of Massachusetts Medical School’s 4 Projected Generic Entry 5 Additional Promising Clinical Pharmacy Services division and 4 Investigational Indications New Agents distributed to our clients twice yearly. 4 FDA Updates In This Issue Promising New Promising New Agents Agents Aflibercept Drug Name: Aclidinium bromide Drug Name: Aflibercept BLA submitted Manufacturer: Almirall, Forest Manufacturer: Regeneron, Bayer for wet age- Phase III Indication: COPD BLA Indication: Wet AMD related macular Formulation: Dry powder inhaler Formulation: Intravitreal injection degeneration Dimethyl fumarate Aclidinium bromide, a long-acting, inhaled Aflibercept is under FDA review for the treatment NDA submission anticholinergic bronchodilator, is an antagonist at of the neovascular form of age-related macular planned for the M2 and M3 muscarinic receptors. It is being degeneration (wet AMD). By inhibiting vascular relapsing-remitting multiple sclerosis studied for the treatment of chronic obstructive endothelial and placental growth factors, aflibercept pulmonary disease (COPD). may reduce the abnormal growth of blood vessels Projected Three Phase III, randomized, double-blind trials that damage the retina through blood and fluid leaks. Generic Entry compared aclidinium bromide 200 μg and 400 μg In two double-blind, non-inferiority, Phase III ® Nasacort AQ twice daily to placebo in patients with moderate to studies, VIEW 1 (N=1,217) and VIEW 2 (N=1,240), Levaquin® severe COPD. In each study, the primary endpoint patients with wet AMD were randomized to Uroxatral® Anzemet® was the change in morning trough forced expiratory intravitreal aflibercept 0.5 mg monthly, 2 mg monthly, Zyprexa® volume in one second (FEV1), from baseline to week or 2 mg every two months following three monthly Zyprexa® Zydis® 12. -

Management of Anemia on Hemodialysis
Chapter 17 Management of Anemia on Hemodialysis Konstantinos Pantelias and Eirini Grapsa Additional information is available at the end of the chapter http://dx.doi.org/10.5772/ 52399 1. Introduction The definition of anemia is controversial. The WHO defines anemia as hemoglobin (Hb)<13 g/dL for men and <12 g/dL for women [1]. The National Kidney Foundation's Kidney Dis‐ ease Outcomes Quality Initiative, which is the criteria used for Medicare reimbursement, de‐ fines anemia in adult men and postmenopausal women as Hb<12 g/dL, or <11 g/dL in a premenopausal woman [2]. Anemia represents a significant problem to deal with in patients with chronic kidney disease (CKD) on hemodialysis (HD). Renal anemia is typically an iso‐ lated normochromic, normocytic anemia with no leukopenia or thrombocytopenia [3]. This is a frequent complication and contributes considerably to reduced quality of life (QoL) [4-6] of patients with CKD. It has also been associated with a number of adverse clinical out‐ comes, increased morbidity and mortality [5, 7-13]. In general, there is a progressive increase in the incidence and severity of anemia with declining renal function. The reported preva‐ lence of anemia by CKD stage varies significantly and depends, to a large extent, on the def‐ inition of anemia and whether study participants selected from the general population, are at a high risk for CKD. Data from the National Health and Nutrition Examination Survey (NHANES) showed that the distribution of Hb levels starts to fall at an estimated glomeru‐ lar filtration rate (eGFR) of less than 75 ml/min per 1.73 m2 in men and 45 ml/min per 1.73 m2 in women [14]. -

WHO Drug Information Vol
WHO Drug Information Vol. 26, No. 4, 2012 WHO Drug Information Contents International Regulatory Regulatory Action and News Harmonization New task force for antibacterial International Conference of Drug drug development 383 Regulatory Authorities 339 NIBSC: new MHRA centre 383 Quality of medicines in a globalized New Pakistan drug regulatory world: focus on active pharma- authority 384 ceutical ingredients. Pre-ICDRA EU clinical trial regulation: public meeting 352 consultation 384 Pegloticase approved for chronic tophaceous gout 385 WHO Programme on Tofacitinib: approved for rheumatoid International Drug Monitoring arthritis 385 Global challenges in medicines Rivaroxaban: extended indication safety 362 approved for blood clotting 385 Omacetaxine mepesuccinate: Safety and Efficacy Issues approved for chronic myelo- Dalfampridine: risk of seizure 371 genous leukaemia 386 Sildenafil: not for pulmonary hyper- Perampanel: approved for partial tension in children 371 onset seizures 386 Interaction: proton pump inhibitors Regorafenib: approved for colorectal and methotrexate 371 cancer 386 Fingolimod: cardiovascular Teriflunomide: approved for multiple monitoring 372 sclerosis 387 Pramipexole: risk of heart failure 372 Ocriplasmin: approved for vitreo- Lyme disease test kits: limitations 373 macular adhesion 387 Anti-androgens: hepatotoxicity 374 Florbetapir 18F: approved for Agomelatine: hepatotoxicity and neuritic plaque density imaging 387 liver failure 375 Insulin degludec: approved for Hypotonic saline in children: fatal diabetes mellitus