Noscapine Suppresses Angiotensin Converting Enzyme Inhibitors-Induced Cough
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Federal Controlled Substances Checklist
Federal Controlled Substances Checklist Introduction By Norton Tooby & Joseph Justin Rollin We have reprinted here an alphabetical list of all controlled substances forbidden under federal drug laws, taken from the official website of the U.S. Department of Justice, Drug Enforcement Administration, Office of Diversion Control, at http://www.justice.gov/dea/pubs/scheduling.html. No copyright is asserted to this information. This list changes frequently. The official list is contained at 21 CFR § 1308, as supplemented by final rules published in the Federal Register. The attached checklist of controlled substances has been compiled into one list, and placed in alphabetical order, for ease of reference. If a controlled substance is listed in the federal drug schedules, it triggers deportation, INA § 237(a)(2)(B)(i), 8 U.S.C. § 1227(a)(2)(B)(i), and inadmissibility. INA § 212(a)(2)(A)(i)(II), 8 U.S.C. § 1182(a)(2)(A)(i)II). In addition, there is an aggravated felony defined as illicit trafficking in a controlled substance. INA § 101(a)(43)(B), 8 U.S.C. § 1101(a)(43)(B). The same controlled substance lists apply to this ground of deportation as well. If a drug is not listed on the federal controlled substances schedules, it does not trigger removal under these grounds. In addition, because the government has the burden of proof in deportation removal proceedings by clear and convincing evidence, if the record of conviction is ambiguous as to whether the specific substance involved in the particular case was listed on the federal schedules, the government cannot obtain a deportation removal order on this ground. -

Recommended Methods for the Identification and Analysis of Fentanyl and Its Analogues in Biological Specimens
Recommended methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES Laboratory and Scientific Section UNITED NATIONS OFFICE ON DRUGS AND CRIME Vienna Recommended Methods for the Identification and Analysis of Fentanyl and its Analogues in Biological Specimens MANUAL FOR USE BY NATIONAL DRUG ANALYSIS LABORATORIES UNITED NATIONS Vienna, 2017 Note Operating and experimental conditions are reproduced from the original reference materials, including unpublished methods, validated and used in selected national laboratories as per the list of references. A number of alternative conditions and substitution of named commercial products may provide comparable results in many cases. However, any modification has to be validated before it is integrated into laboratory routines. ST/NAR/53 Original language: English © United Nations, November 2017. All rights reserved. The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the Secretariat of the United Nations concerning the legal status of any country, territory, city or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. Mention of names of firms and commercial products does not imply the endorse- ment of the United Nations. This publication has not been formally edited. Publishing production: English, Publishing and Library Section, United Nations Office at Vienna. Acknowledgements The Laboratory and Scientific Section of the UNODC (LSS, headed by Dr. Justice Tettey) wishes to express its appreciation and thanks to Dr. Barry Logan, Center for Forensic Science Research and Education, at the Fredric Rieders Family Founda- tion and NMS Labs, United States; Amanda L.A. -

Control Substance List
Drugs DrugID SubstanceName DEANumbScheNarco OtherNames 1 1-(1-Phenylcyclohexyl)pyrrolidine 7458 I N PCPy, PHP, rolicyclidine 2 1-(2-Phenylethyl)-4-phenyl-4-acetoxypiperidine 9663 I Y PEPAP, synthetic heroin 3 1-[1-(2-Thienyl)cyclohexyl]piperidine 7470 I N TCP, tenocyclidine 4 1-[1-(2-Thienyl)cyclohexyl]pyrrolidine 7473 I N TCPy 5 13Beta-ethyl-17beta-hydroxygon-4-en-3-one 4000 III N 6 17Alpha-methyl-3alpha,17beta-dihydroxy-5alpha-androstane 4000 III N 7 17Alpha-methyl-3beta,17beta-dihydroxy-5alpha-androstane 4000 III N 8 17Alpha-methyl-3beta,17beta-dihydroxyandrost-4-ene 4000 III N 9 17Alpha-methyl-4-hydroxynandrolone (17alpha-methyl-4-hyd 4000 III N 10 17Alpha-methyl-delta1-dihydrotestosterone (17beta-hydroxy- 4000 III N 17-Alpha-methyl-1-testosterone 11 19-Nor-4-androstenediol (3beta,17beta-dihydroxyestr-4-ene; 4000 III N 12 19-Nor-4-androstenedione (estr-4-en-3,17-dione) 4000 III N 13 19-Nor-5-androstenediol (3beta,17beta-dihydroxyestr-5-ene; 4000 III N 14 19-Nor-5-androstenedione (estr-5-en-3,17-dione) 4000 III N 15 1-Androstenediol (3beta,17beta-dihydroxy-5alpha-androst-1- 4000 III N 16 1-Androstenedione (5alpha-androst-1-en-3,17-dione) 4000 III N 17 1-Methyl-4-phenyl-4-propionoxypiperidine 9661 I Y MPPP, synthetic heroin 18 1-Phenylcyclohexylamine 7460 II N PCP precursor 19 1-Piperidinocyclohexanecarbonitrile 8603 II N PCC, PCP precursor 20 2,5-Dimethoxy-4-(n)-propylthiophenethylamine 7348 I N 2C-T-7 21 2,5-Dimethoxy-4-ethylamphetamine 7399 I N DOET 22 2,5-Dimethoxyamphetamine 7396 I N DMA, 2,5-DMA 23 3,4,5-Trimethoxyamphetamine -

Drugs of Abuseon September Archived 13-10048 No
U.S. DEPARTMENT OF JUSTICE DRUG ENFORCEMENT ADMINISTRATION WWW.DEA.GOV 9, 2014 on September archived 13-10048 No. v. Stewart, in U.S. cited Drugs of2011 Abuse EDITION A DEA RESOURCE GUIDE V. Narcotics WHAT ARE NARCOTICS? Also known as “opioids,” the term "narcotic" comes from the Greek word for “stupor” and originally referred to a variety of substances that dulled the senses and relieved pain. Though some people still refer to all drugs as “narcot- ics,” today “narcotic” refers to opium, opium derivatives, and their semi-synthetic substitutes. A more current term for these drugs, with less uncertainty regarding its meaning, is “opioid.” Examples include the illicit drug heroin and pharmaceutical drugs like OxyContin®, Vicodin®, codeine, morphine, methadone and fentanyl. WHAT IS THEIR ORIGIN? The poppy papaver somniferum is the source for all natural opioids, whereas synthetic opioids are made entirely in a lab and include meperidine, fentanyl, and methadone. Semi-synthetic opioids are synthesized from naturally occurring opium products, such as morphine and codeine, and include heroin, oxycodone, hydrocodone, and hydromorphone. Teens can obtain narcotics from friends, family members, medicine cabinets, pharmacies, nursing 2014 homes, hospitals, hospices, doctors, and the Internet. 9, on September archived 13-10048 No. v. Stewart, in U.S. cited What are common street names? Street names for various narcotics/opioids include: ➔ Hillbilly Heroin, Lean or Purple Drank, OC, Ox, Oxy, Oxycotton, Sippin Syrup What are their forms? Narcotics/opioids come in various forms including: ➔ T ablets, capsules, skin patches, powder, chunks in varying colors (from white to shades of brown and black), liquid form for oral use and injection, syrups, suppositories, lollipops How are they abused? ➔ Narcotics/opioids can be swallowed, smoked, sniffed, or injected. -
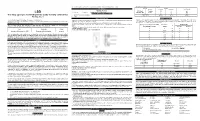
(LSD) Test Dip Card (Urine) • Specimen Collection Container % Agreement 98.8% 99
frozen and stored below -20°C. Frozen specimens should be thawed and mixed before testing. GC/MS. The following results were tabulated: Method GC/MS MATERIALS Total Results Results Positive Negative Materials Provided LSD Rapid Positive 79 1 80 LSD • Test device • Desiccants • Package insert • Urine cups Test Dip card Negative 1 99 100 Materials Required But Not Provided Total Results 80 100 180 One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) • Specimen collection container % Agreement 98.8% 99. % 98.9% • Timer Package Insert DIRECTIONS FOR USE Analytical Sensitivity This Instruction Sheet is for testing of Lysergic acid diethylamide. Allow the test device, and urine specimen to come to room temperature [15-30°C (59-86°F)] prior to testing. A drug-free urine pool was spiked with LSD at the following concentrations: 0 ng/mL, -50%cutoff, -25%cutoff, cutoff, A rapid, one step test for the qualitative detection of Lysergic acid diethylamide and its metabolites in human urine. 1) Remove the test device from the foil pouch. +25%cutoff and +50%cutoff. The result demonstrates >99% accuracy at 50% above and 50% below the cut-off For forensic use only. 2) Remove the cap from the test device. Label the device with patient or control identifications. concentration. The data are summarized below: INTENDED USE 3) Immerse the absorbent tip into the urine sample for 10-15 seconds. Urine sample should not touch the plastic Lysergic acid diethylamide (LSD) Percent of Visual Result The One Step Lysergic acid diethylamide (LSD) Test Dip card (Urine) is a lateral flow chromatographic device. -

Supplement 1: Additional Tables and Figures
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) BMJ Global Health Supplement 1: Additional tables and figures Box S1: Substances included and excluded from the International Narcotic Control Board (INCB) data on narcotic consumption, in alphabetical order. Opioids included in the opioid consumption calculation: 1. (+)-cis-3-methylfental 35. Bezitramide 2. 3-Acetylmorphine 36. Butyrfentanyl 3. 3-Methylfentanyl 37. Carfentanil 4. 3-Methylthiofentanyl 38. Carfentanyl 5. 3-Monoacetylmorphine 39. Clonitazene 6. 4-Fluoroisobutyrfentanyl 40. Codeine 7. 6-Acetylmorphine 41. Codeine-6GLUC 8. 6-Monoacetylmorphine 42. Codeine-6-glucuronide 9. Acetorphine 43. Codeine-Methyl 10. Acetyl-alpha-methylfentanyl 44. Codeine-N-oxide 11. Acetyldihydrocodeine 45. Codoxime 12. Acetylfentanyl 46. Conc. of poppy straw (C) ACA 13. Acetylmethadol 47. Conc. of poppy straw (C) AMA 14. Acetylmorphine 48. Conc. of poppy straw (C) AOA 15. Acrylfentanyl 49. Conc. of poppy straw (C) ATA 16. AH-7921 50. Conc. of poppy straw (C) GW 17. Alfentanil 51. Conc. of poppy straw (M) ACA 18. Allylprodine 52. Conc. of poppy straw (M) AMA 19. Alphacetylmethadol 53. Conc. of poppy straw (M) AOA 20. Alphameprodine 54. Conc. of poppy straw (M) ATA 21. Alphamethadol 55. Conc. of poppy straw (M) GW 22. alpha-Methylfentanyl 56. Conc. of poppy straw (N) GW 23. alpha-Methylthiofentanyl 57. Conc. of poppy straw (O) 24. Alphaprodine 58. Conc. of poppy straw (O) ACA 25. Anileridine 59. Conc. of poppy straw (O) AMA 26. Benzethidine 60. Conc. of poppy straw (O) AOA 27. -

Review Memorandum
510(k) SUBSTANTIAL EQUIVALENCE DETERMINATION DECISION SUMMARY ASSAY ONLY TEMPLATE A. 510(k) Number: k112395 B. Purpose for Submission: New device C. Measurand: Phencyclidine and Nortriptyline D. Type of Test: Qualitative immunochromatographic E. Applicant: Guangzhou Wondfo Biotech Co., Ltd. F. Proprietary and Established Names: Wondfo Phencyclidine Urine Test Wondfo Nortriptyline Urine Test G. Regulatory Information: Product Classification Regulation Section Panel Code LCM unclassified Enzyme Immunoassay 91, Toxicology Phencyclidine LFG II 21 CFR 862.3910 -Tricyclic 91, Toxicology antidepressant drug test system H. Intended Use: 1. Intended use(s): See indication for use below 1 2. Indication(s) for use: Wondfo Phencyclidine Urine Test Wondfo Phencyclidine Urine Test is an immunochromatographic assay for the qualitative determination of Phencyclidine in human urine at a cutoff concentration of 25 ng/mL. The test is available in a dip card format and a cup format. It is intended for prescription use and over the counter use. The test provides only preliminary test results. A more specific alternative chemical method must be used in order to obtain a confirmed analytical result. GC/MS is the preferred confirmatory method. Clinical consideration and professional judgment should be exercised with any drug of abuse test result, particularly when the preliminary result is positive. Wondfo Nortriptyline Urine Test Wondfo Nortriptyline Urine Test is an immunochromatographic assay for the qualitative determination of Nortriptyline (major metabolite of Tricyclic Antidepressants) in human urine at a cutoff concentration of 1000 ng/mL. The test is available in a dip card format and a cup format. It is intended for prescription use and over the counter use. -

BULLETIN on NARCOTICS, Volume LVII, Nos. 1 and 2, 2005
Drug profiling: a new scientific contribution to law enforcement operations in Viet Nam H. M. HUNG, N. D. TIEN and N. X. TRUONG* Institute of Forensic Sciences of Viet Nam, Hanoi, Viet Nam ABSTRACT Since 1995 heroin sample comparisons have been carried out in Viet Nam to establish links between wholesalers and retailers. To that end, the physical and chemical characteristics of samples are analysed: their colour, the packaging material, including fingerprints, diacetylmorphine (heroin) content and the composition of some main alkaloids. At the beginning of 2002, having acquired expertise on impurity profiling and with the support of new instruments, the Institute of Forensic Sciences of Viet Nam introduced the routine impurity profiling of seized heroin and methamphetamine and later undertook to explain that process to national law enforcement bodies. Since then, 375 heroin and 29 methamphetamine samples have been analysed for major and minor impurities. Substances detected in the analysis of illicit heroin include diacetylmorphine, morphine, codeine, O6-monoacetylmorphine and acetylcodeine as well as adulterants such as paracetamol and caffeine. Since methamphetamine impurity profiling began, 29 samples have so far been analysed, and some samples have been grouped through the application of cluster analysis. In the case of heroin, impurity profiling has established a link between two major trafficking groups suspected of obtaining heroin from the same source of production. Analysis has also revealed a link between one wholesaler and several retailers in one region. In addition, impurity profiling provides new information on the preparation and production of some methamphetamine and fake Ecstasy tablets. Keywords: forensic science; heroin; methamphetamine; gas chromatography (GC); gas chromatography/mass spectrometry (GC/MS); linking samples; methods of production *The authors would like to express their gratitude to K. -

Noscapine, a Non-Addictive Opioid and Microtubule-Inhibitor In
Neurochemical Research (2019) 44:1796–1806 https://doi.org/10.1007/s11064-019-02837-x REVIEW Noscapine, a Non‑addictive Opioid and Microtubule‑Inhibitor in Potential Treatment of Glioblastoma Meric A. Altinoz1,2 · Gulacti Topcu3 · Ahmet Hacimuftuoglu4 · Alp Ozpinar5 · Aysel Ozpinar1 · Emily Hacker5 · İlhan Elmaci6 Received: 5 April 2019 / Revised: 12 June 2019 / Accepted: 21 June 2019 / Published online: 10 July 2019 © Springer Science+Business Media, LLC, part of Springer Nature 2019 Abstract Noscapine is a phthalide isoquinoline alkaloid that easily traverses the blood brain barrier and has been used for years as an antitussive agent with high safety. Despite binding opioid receptors, noscapine lacks signifcant hypnotic and euphoric efects rendering it safe in terms of addictive potential. In 1954, Hans Lettré frst described noscapine as a mitotic poison. The drug was later tested for cancer treatment in the early 1960’s, yet no efect was observed likely as a result of its short biological half-life and limited water solubility. Since 1998, it has regained interest thanks to studies from Emory University, which showed its anticancer activity in animal models with negligible toxicity. In contrast to other microtubule-inhibitors, noscapine does not afect the total intracellular tubulin polymer mass. Instead, it forces the microtubules to spend an increased amount of time in a paused state leading to arrest in mitosis and subsequently inducing mitotic slippage/mitotic catastrophe/apop- tosis. In experimental models, noscapine does not induce peripheral neuropathy, which is common with other microtubule inhibitors. Noscapine also inhibits tumor growth and enhances cancer chemosensitivity via selective blockage of NF-κB, an important transcription factor in glioblastoma pathogenesis. -

Radiolabeling, Biodistribution and Gamma Scintigraphy of Noscapine
Priyadarshani et al. Journal of Ovarian Research 2010, 3:10 http://www.ovarianresearch.com/content/3/1/10 RESEARCH Open Access Radiolabeling,Research biodistribution and gamma scintigraphy of noscapine hydrochloride in normal and polycystic ovary induced rats Anjali Priyadarshani1, Krishna Chuttani2, Gaurav Mittal2 and Aseem Bhatnagar*2 Abstract Background: Noscapine, an alkaloid from Papaver somniferum, widely used as an antitussive, is being clinically studied in the treatment of polycystic ovary syndrome (PCOS) and a few other cancers primarily because of its anti- angiogenesis properties. With the advent of diverse application of noscapine, we sought to determine whether the radiolabeling method can be useful in studying uptake and kinetics of the molecule in-vivo. Specific objectives of this study were to radiolabel noscapine with Technetium-99m (Tc-99m), to determine its organ biodistribution in rat model and study its uptake kinetics in PCOS model. Methods: A method for radiolabeling noscapine with Tc-99m was standardized using stannous reduction method and its in vitro and in vivo stability parameters were studied. The radiopharmaceutical was also evaluated for blood kinetics and biodistribution profile. An animal model of PCOS was created by using antiprogesterone RU486 and uptake of 99mTc-noscapine in normal and PCOS ovaries was compared using gamma scintigraphy. Results: Noscapine hydrochloride was successfully radiolabeled with Tc-99m with high labeling efficiency and in vitro stability. Most of the blood clearance of the drug (80%) took place in first hour after intravascular injection with maximum accumulation being observed in liver, spleen, kidney followed by the ovary. At 4 hours post injection, radiolabeled complex accumulation doubled in PCOS ovaries in rats (0.9 ± 0.03% ID/whole organ) compared to normal cyclic rats (0.53 ± 0.01% ID/whole organ). -

Solution of the Multistep Pathway for Assembly of Corynanthean, Strychnos, Iboga, and Aspidosperma Monoterpenoid Indole Alkaloids from 19E-Geissoschizine
Solution of the multistep pathway for assembly of corynanthean, strychnos, iboga, and aspidosperma monoterpenoid indole alkaloids from 19E-geissoschizine Yang Qua, Michael E. A. M. Eassona,1, Razvan Simionescub, Josef Hajicekb,2, Antje M. K. Thamma,3, Vonny Salima,4, and Vincenzo De Lucaa,5 aDepartment of Biological Sciences, Brock University, St. Catharines, ON L2S 3A1, Canada; and bDepartment of Chemistry, Brock University, St. Catharines, ON L2S 3A1, Canada Edited by Jerrold Meinwald, Cornell University, Ithaca, NY, and approved February 11, 2018 (received for review November 16, 2017) Monoterpenoid indole alkaloids (MIAs) possess a diversity of for the formation of tabersonine or catharanthine from 19E- alkaloid skeletons whose biosynthesis is poorly understood. A geissoschizine. Gene discovery involved a combination of bio- bioinformatic search of candidate genes, combined with their informatics and virus-induced gene silencing (VIGS) to identify virus-induced gene silencing, targeted MIA profiling and in vitro/ candidate genes and functional expression of the selected genes in vivo pathway reconstitution identified and functionally charac- by in vitro/in vivo reconstitution of the pathway. A series of terized six genes as well as a seventh enzyme reaction required for highly unstable intermediates that rearrange to other important the conversion of 19E-geissoschizine to tabersonine and catharan- MIA precursors when not used by appropriate enzymes reveals thine. The involvement of pathway intermediates in the formation the plasticity of MIA formation and how this fundamental of four MIA skeletons is described, and the role of stemmadenine- property led to diverse MIA structures found in nature. O-acetylation in providing necessary reactive substrates for the formation of iboga and aspidosperma MIAs is described. -
Mephedrone Risk Assessment Report
TD-AK-11-001-EN-C Report on the risk assessment of mephedrone in the framework of the Council Decision on new psychoactive substances ISSN 1725–4485 About the EMCDDA The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) is one of the European Union’s decentralised agencies. Established in 1993 and based in Lisbon, it is the central source of comprehensive information on drugs and drug addiction in Europe. The EMCDDA collects, analyses and disseminates factual, objective, reliable and comparable information on drugs and drug addiction. In doing so, it provides its audiences with an evidence-based picture of the drug phenomenon EMCDDA at European level. The Centre’s publications are a prime source of information for RISK ASSESSMENTS a wide range of audiences including policymakers and their advisors, professionals and researchers working in the drugs field and, more broadly, the media and general public. EMCDDA risk assessments are publications examining the health and social risks of individual synthetic drugs on the basis of Report on the risk assessment of mephedrone research carried out by the agency and its partners. in the framework of the Council Decision on new psychoactive substances How to obtain EU publications Free publications: • via EU Bookshop (http://bookshop.europa.eu); • at the European Union’s representations or delegations. You can obtain their contact details on the Internet (http://ec.europa.eu) or by sending a fax to +352 2929-42758. Priced publications: • via EU Bookshop (http://bookshop.europa.eu). Priced subscriptions (e.g. annual series of the Official Journal of the European Union and reports of cases before the Court of Justice of the European Union): • via one of the sales agents of the Publications Office of the European Union (http://publications.europa.eu/others/agents/index_en.htm).