Universidad Autónoma De Madrid
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Specimen Type, Collection Methods, and Diagnostic Assays Available For
Specimen type, collection methods, and diagnostic assays available for the detection of poxviruses from human specimens by the Poxvirus and Rabies Branch, Centers for Disease Control and Prevention1. Specimen Orthopoxvirus Parapoxvirus Yatapoxvirus Molluscipoxvirus Specimen type collection method PCR6 Culture EM8 IHC9,10 Serology11 PCR12 EM8 IHC9,10 PCR13 EM8 PCR EM8 Lesion material Fresh or frozen Swab 5 Lesion material [dry or in media ] [vesicle / pustule Formalin fixed skin, scab / crust, etc.] Paraffin block Fixed slide(s) Container Lesion fluid Swab [vesicle / pustule [dry or in media5] fluid, etc.] Touch prep slide Blood EDTA2 EDTA tube 7 Spun or aliquoted Serum before shipment Spun or aliquoted Plasma before shipment CSF3,4 Sterile 1. The detection of poxviruses by electron microscopy (EM) and immunohistochemical staining (IHC) is performed by the Infectious Disease Pathology Branch of the CDC. 2. EDTA — Ethylenediaminetetraacetic acid. 3. CSF — Cerebrospinal fluid. 4. In order to accurately interpret test results generated from CSF specimens, paired serum must also be submitted. 5. If media is used to store and transport specimens a minimal amount should be used to ensure as little dilution of DNA as possible. 6. Orthopoxvirus generic real-time polymerase chain reaction (PCR) assays will amplify DNA from numerous species of virus within the Orthopoxvirus genus. Species-specific real-time PCR assays are available for selective detection of DNA from variola virus, vaccinia virus, monkeypox virus, and cowpox virus. 7. Blood is not ideal for the detection of orthopoxviruses by PCR as the period of viremia has often passed before sampling occurs. 8. EM can reveal the presence of a poxvirus in clinical specimens or from virus culture, but this technique cannot differentiate between virus species within the same genus. -
Here, There, and Everywhere: the Wide Host Range and Geographic Distribution of Zoonotic Orthopoxviruses
viruses Review Here, There, and Everywhere: The Wide Host Range and Geographic Distribution of Zoonotic Orthopoxviruses Natalia Ingrid Oliveira Silva, Jaqueline Silva de Oliveira, Erna Geessien Kroon , Giliane de Souza Trindade and Betânia Paiva Drumond * Laboratório de Vírus, Departamento de Microbiologia, Instituto de Ciências Biológicas, Universidade Federal de Minas Gerais: Belo Horizonte, Minas Gerais 31270-901, Brazil; [email protected] (N.I.O.S.); [email protected] (J.S.d.O.); [email protected] (E.G.K.); [email protected] (G.d.S.T.) * Correspondence: [email protected] Abstract: The global emergence of zoonotic viruses, including poxviruses, poses one of the greatest threats to human and animal health. Forty years after the eradication of smallpox, emerging zoonotic orthopoxviruses, such as monkeypox, cowpox, and vaccinia viruses continue to infect humans as well as wild and domestic animals. Currently, the geographical distribution of poxviruses in a broad range of hosts worldwide raises concerns regarding the possibility of outbreaks or viral dissemination to new geographical regions. Here, we review the global host ranges and current epidemiological understanding of zoonotic orthopoxviruses while focusing on orthopoxviruses with epidemic potential, including monkeypox, cowpox, and vaccinia viruses. Keywords: Orthopoxvirus; Poxviridae; zoonosis; Monkeypox virus; Cowpox virus; Vaccinia virus; host range; wild and domestic animals; emergent viruses; outbreak Citation: Silva, N.I.O.; de Oliveira, J.S.; Kroon, E.G.; Trindade, G.d.S.; Drumond, B.P. Here, There, and Everywhere: The Wide Host Range 1. Poxvirus and Emerging Diseases and Geographic Distribution of Zoonotic diseases, defined as diseases or infections that are naturally transmissible Zoonotic Orthopoxviruses. Viruses from vertebrate animals to humans, represent a significant threat to global health [1]. -

Discovery of Antivirals Against Smallpox
Discovery of antivirals against smallpox Stephen C. Harrisona,b, Bruce Albertsc, Ellie Ehrenfeldd, Lynn Enquiste, Harvey Finebergf, Steven L. McKnightg, Bernard Mossh, Michael O’Donnelli, Hidde Ploeghj, Sandra L. Schmidk, K. Peter Walterl, and Julie Theriotm aHarvard Medical School, Howard Hughes Medical Institute, Seeley Mudd Building, Room 130, 250 Longwood Avenue, Boston, MA 02115; cNational Academy of Sciences, 2101 Constitution Avenue, NW, Washington, DC 20418; dLaboratory of Infectious Disease, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Building 50, Room 6120, 50 South Drive, Bethesda, MD 20892; ePrinceton University, 314 Schultz Laboratory, Washington Road, Princeton, NJ 08544; fInstitute of Medicine, 2101 Constitution Avenue, NW, Washington, DC 20418; gDepartment of Biochemistry, University of Texas Southwestern Medical Center, 5323 Harry Hines Boulevard, Dallas, TX 75390; hLaboratory of Viral Diseases, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Building 4, Room 229, 4 Center Drive, Bethesda, MD 20892; iLaboratory of DNA Replication, The Rockefeller University, Howard Hughes Medical Institute, 1230 York Avenue, New York, NY 10021; jDepartment of Pathology, Harvard Medical School, NRB, 77 Avenue Louis Pasteur, Boston, MA 02115; kDepartment of Cell Biology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, CA 92037; lDepartment of Biochemistry and Biophysics, University of California School of Medicine, Howard Hughes Medical Institute, Box 0448, HSE 1001, San Francisco, CA 94143; and mDepartment of Biochemistry, Stanford University School of Medicine, Stanford, CA 94305 Contributed by Stephen C. Harrison, May 21, 2004 mallpox, a devastating infectious Whatever the likelihood of covertly dopoxviruses has a restricted and spe- disease dreaded throughout much held variola virus stocks, an intentional cific host array (Table 2). -

BMBL) Quickly Became the Cornerstone of Biosafety Practice and Policy in the United States Upon First Publication in 1984
Biosafety in Microbiological and Biomedical Laboratories 5th Edition U.S. Department of Health and Human Services Public Health Service Centers for Disease Control and Prevention National Institutes of Health HHS Publication No. (CDC) 21-1112 Revised December 2009 Foreword Biosafety in Microbiological and Biomedical Laboratories (BMBL) quickly became the cornerstone of biosafety practice and policy in the United States upon first publication in 1984. Historically, the information in this publication has been advisory is nature even though legislation and regulation, in some circumstances, have overtaken it and made compliance with the guidance provided mandatory. We wish to emphasize that the 5th edition of the BMBL remains an advisory document recommending best practices for the safe conduct of work in biomedical and clinical laboratories from a biosafety perspective, and is not intended as a regulatory document though we recognize that it will be used that way by some. This edition of the BMBL includes additional sections, expanded sections on the principles and practices of biosafety and risk assessment; and revised agent summary statements and appendices. We worked to harmonize the recommendations included in this edition with guidance issued and regulations promulgated by other federal agencies. Wherever possible, we clarified both the language and intent of the information provided. The events of September 11, 2001, and the anthrax attacks in October of that year re-shaped and changed, forever, the way we manage and conduct work -

B Directive 2000/54/Ec of the European
02000L0054 — EN — 24.06.2020 — 002.001 — 1 This text is meant purely as a documentation tool and has no legal effect. The Union's institutions do not assume any liability for its contents. The authentic versions of the relevant acts, including their preambles, are those published in the Official Journal of the European Union and available in EUR-Lex. Those official texts are directly accessible through the links embedded in this document ►B DIRECTIVE 2000/54/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 18 September 2000 on the protection of workers from risks related to exposure to biological agents at work (seventh individual directive within the meaning of Article 16(1) of Directive 89/391/EEC) (OJ L 262, 17.10.2000, p. 21) Amended by: Official Journal No page date ►M1 Commission Directive (EU) 2019/1833 of 24 October 2019 L 279 54 31.10.2019 ►M2 Commission Directive (EU) 2020/739 of 3 June 2020 L 175 11 4.6.2020 02000L0054 — EN — 24.06.2020 — 002.001 — 2 ▼B DIRECTIVE 2000/54/EC OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 18 September 2000 on the protection of workers from risks related to exposure to biological agents at work (seventh individual directive within the meaning of Article 16(1) of Directive 89/391/EEC) CHAPTER I GENERAL PROVISIONS Article 1 Objective 1. This Directive has as its aim the protection of workers against risks to their health and safety, including the prevention of such risks, arising or likely to arise from exposure to biological agents at work. -

Report for the Hemodialysis Vascular Access: Standardized Fistula Rate
ESRD Quality Measure Development, Maintenance, and Support Contract Number HHSM-500-2013-13017I Report for the Hemodialysis Vascular Access: Standardized Fistula Rate (SFR) NQF #2977 Submitted to CMS by the University of Michigan Kidney Epidemiology and Cost Center June 21, 2017 Produced by UM-KECC Submitted: 6.21.2017 1 ESRD Quality Measure Development, Maintenance, and Support Contract Number HHSM-500-2013-13017I Table of Contents Introduction .................................................................................................................................................. 3 Methods ........................................................................................................................................................ 3 Overview ................................................................................................................................................... 3 Data Sources ............................................................................................................................................. 4 Outcome Definition .................................................................................................................................. 4 Denominator Definition ............................................................................................................................ 5 Risk Adjustment ........................................................................................................................................ 5 Choosing Adjustment Factors -

1 a Single Vertebrate DNA Virus Protein Disarms Invertebrate
A single vertebrate DNA virus protein disarms invertebrate immunity to RNA virus infection Don B. Gammon1, Sophie Duraffour2, Daniel K. Rozelle3, Heidi Hehnly4, Rita Sharma1,9, Michael E. Sparks5, Cara C. West6, Ying Chen1, James J. Moresco7, Graciela Andrei2, John H. Connor3, Darryl Conte Jr1., Dawn E. Gundersen-Rindal5, William L. Marshall6,8#, John R. Yates III7, Neal Silverman6 and Craig C. Mello1,9,*. 1University of Massachusetts Medical School, RNA Therapeutics Institute, Worcester, MA, USA. 2Rega Institute for Medical Research, Leuven, Belgium. 3Boston University, Department of Microbiology, Boston, MA, USA. 4University of Massachusetts Medical School, Program in Molecular Medicine, Worcester, MA, USA. 5United States Department of Agriculture, Agricultural Research Service, Beltsville, MD, USA. 6University of Massachusetts Medical School, Department of Medicine, Worcester, MA, USA. 7The Scripps Research Institute, Department of Chemical Physiology, La Jolla, CA, USA. 8Merck Research Laboratories, Boston, MA, USA. #Current Address. 9Howard Hughes Medical Institute, University of Massachusetts Medical School, Worcester, MA, USA. *Corresponding author: Please address all correspondence to Dr. Craig Mello at the University of Massachusetts Medical School. Email: [email protected]. Telephone: 508-856-1602. 1 1 Abstract 2 Virus-host interactions drive a remarkable diversity of immune responses and 3 countermeasures. We found that two RNA viruses with broad host ranges, vesicular 4 stomatitis virus (VSV) and Sindbis virus (SINV), are completely restricted in their 5 replication after entry into Lepidopteran cells. This restriction is overcome when cells 6 are co-infected with vaccinia virus (VACV), a vertebrate DNA virus. Using RNAi 7 screening, we show that Lepidopteran RNAi, Nuclear Factor-κB, and ubiquitin- 8 proteasome pathways restrict RNA virus infection. -

A Single Vertebrate DNA Virus Protein Disarms Invertebrate Immunity To
RESEARCH ARTICLE elifesciences.org A single vertebrate DNA virus protein disarms invertebrate immunity to RNA virus infection Don B Gammon1, Sophie Duraffour2, Daniel K Rozelle3, Heidi Hehnly4, Rita Sharma1,5, Michael E Sparks6†, Cara C West7, Ying Chen1, James J Moresco8, Graciela Andrei2, John H Connor3, Darryl Conte Jr.1, Dawn E Gundersen-Rindal6, William L Marshall7‡, John R Yates8, Neal Silverman7, Craig C Mello1,5* 1RNA Therapeutics Institute, University of Massachusetts Medical School, Worcester, United States; 2Rega Institute for Medical Research, KU Leuven, Leuven, Belgium; 3Department of Microbiology, Boston University, Boston, United States; 4Program in Molecular Medicine, University of Massachusetts Medical School, Worcester, United States; 5Howard Hughes Medical Institute, University of Massachusetts Medical School, Worcester, United States; 6Agricultural Research Service, United States Department of Agriculture, Beltsville, United States; 7Department of Medicine, University of Massachusetts Medical School, Worcester, United States; 8Department of Chemical Physiology, The Scripps Research Institute, La Jolla, United States *For correspondence: craig. [email protected] Abstract Virus-host interactions drive a remarkable diversity of immune responses and Present address: †Multidrug- countermeasures. We found that two RNA viruses with broad host ranges, vesicular stomatitis resistant Organism Repository virus (VSV) and Sindbis virus (SINV), are completely restricted in their replication after entry into and Surveillance Network, Walter Lepidopteran cells. This restriction is overcome when cells are co-infected with vaccinia virus Reed Army Institute of Research, (VACV), a vertebrate DNA virus. Using RNAi screening, we show that Lepidopteran RNAi, Nuclear Silver Spring, United States; Factor-κB, and ubiquitin-proteasome pathways restrict RNA virus infection. Surprisingly, a highly ‡Merck Research Laboratories, conserved, uncharacterized VACV protein, A51R, can partially overcome this virus restriction. -
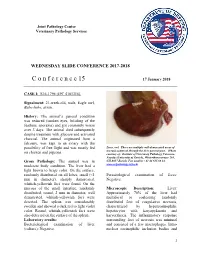
C O N F E R E N C E 15 17 January 2018
Joint Pathology Center Veterinary Pathology Services WEDNESDAY SLIDE CONFERENCE 2017-2018 C o n f e r e n c e 15 17 January 2018 CASE I: S16-1796 (JPC 4101316). Signalment: 21-week-old, male, Eagle owl, Bubo bubo, avian. History: The animal’s general condition was reduced (sunken eyes, bristling of the feathers, anorexia) and got constantly worse over 3 days. The animal died subsequently despite treatment with glucose and activated charcoal. The animal originated from a falconry, was kept in an aviary with the possibility of free flight and was mostly fed Liver, owl. There are multiple well-demarcated areas of necrosis scattered through the liver parenchyma. (Photo on chicken and pigeons. courtesy of: Institute of Veterinary Pathology Vetsuisse- Faculty (University of Zurich), Winterthurerstrasse 268, Gross Pathology: The animal was in CH-8057 Zurich, Fax number +41 44 635 89 34, moderate body condition. The liver had a www.vetpathology.uzh.ch) light brown to beige color. On the surface, randomly distributed on all lobes, small (<1 Parasitological examination of feces: mm in diameter), sharply demarcated, Negative. whitish-yellowish foci were found. On the mucosa of the small intestine, randomly Microscopic Description: Liver: distributed, round, 2 mm in diameter, well Approximately 70% of the liver had demarcated, whitish-yellowish foci were multifocal to coalescing randomly detected. The spleen was considerably distributed foci of coagulative necrosis, swollen and showed a dark red to light violet characterized by hypereosinophilic color. Round, whitish-yellowish foci were hepatocytes with karyopyknosis and also detected on the surface of the spleen. karyorrhexis. The inflammatory response Laboratory results: surrounding foci of necrosis was minimal Bacteriological examination of liver and consisted of a few macrophages. -

The Genome Sequence of Yaba-Like Disease Virus, a Yatapoxvirus
Virology 281, 170–192 (2001) doi:10.1006/viro.2000.0761, available online at http://www.idealibrary.com on View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector The Genome Sequence of Yaba-like Disease Virus, a Yatapoxvirus Han-Joo Lee,*,1 Karim Essani,† and Geoffrey L. Smith*,2 *Sir William Dunn School of Pathology, University of Oxford, South Parks Road, Oxford OX1 3RE, United Kingdom; and †Department of Biological Sciences, Western Michigan University, Michigan 49008 Received July 18, 2000; returned to author for revision August 18, 2000; accepted November 28, 2000 The genome sequence of Yaba-like disease virus (YLDV), an unclassified member of the yatapoxvirus genus, has been determined. Excluding the terminal hairpin loops, the YLDV genome is 144,575 bp in length and contains inverted terminal repeats (ITRs) of 1883 bp. Within 20 nucleotides of the termini, there is a sequence that is conserved in other poxviruses and is required for the resolution of concatemeric replicative DNA intermediates. The nucleotide composition of the genome is 73% AϩT, but the ITRs are only 63% AϩT. The genome contains 151 tightly packed open reading frames (ORFs) that either are Ն180 nucleotides in length or are conserved in other poxviruses. ORFs within 23 kb of each end are transcribed toward the termini, whereas ORFs within the central region of the genome are encoded on either DNA strand. In the central region ORFs have a conserved position, orientation, and sequence compared with vaccinia virus ORFs and encode many enzymes, transcription factors, or structural proteins. -

Supporting Information
Supporting Information Wu et al. 10.1073/pnas.0905115106 20 15 10 5 0 10 15 20 25 30 35 40 Fig. S1. HGT cutoff and tree topology. Robinson-Foulds (RF) distance [Robinson DF, Foulds LR (1981) Math Biosci 53:131–147] between viral proteome trees with different horizontal gene transfer (HGT) cutoffs h at feature length 8. Tree distances are between h and h-1. The tree topology remains stable for h in the range 13–31. We use h ϭ 20 in this work. Wu et al. www.pnas.org/cgi/content/short/0905115106 1of6 20 18 16 14 12 10 8 6 0.0/0.5 0.5/0.7 0.7/0.9 0.9/1.1 1.1/1.3 1.3/1.5 Fig. S2. Low complexity features and tree topology. Robinson-Foulds (RF) distance between viral proteome trees with different low-complexity cutoffs K2 for feature length 8 and HGT cutoff 20. The tree topology changes least for K2 ϭ 0.9, 1.1 and 1.3. We choose K2 ϭ 1.1 for this study. Wu et al. www.pnas.org/cgi/content/short/0905115106 2of6 Table S1. Distribution of the 164 inter-viral-family HGT instances bro hr RR2 RR1 IL-10 Ubi TS Photol. Total Baculo 45 1 10 9 11 1 77 Asco 11 7 1 19 Nudi 1 1 1 3 SGHV 1 1 2 Nima 1 1 2 Herpes 48 12 Pox 18 8 2 3 1 3 35 Irido 1 1 2 4 Phyco 2 3 2 1 8 Allo 1 1 2 Total 56 8 35 24 6 17 14 4 164 The HGT cutoff is 20 8-mers. -

Varicella- Zoster Virus
Laboratory Diagnosis of Viral Skin Infections M Parsania, Ph.D. Tehran Medical Sciences Branch, Islamic Azad University important viral agents causing skin and mucus membranes Infections in human ¾ viruses cause maculopapular rashes rubella virus HiBHuman parvovirus B19 Measles virus Enteroviruses Human herpes viruses types 6 and 7 ¾ viruses cause vesicular skin rashes Herpes simplex virus Varicella-zoster virus Enteroviruses Pox viruses ¾ viruses cause wart-like lesions on the skin and mucus membranes Human Papilloma viruses Molluscum contagiosum virus Diseases of the Skin Caused by Herpesviruses The Relationships between the Human Herpesviruses HSV Viral Structure • Composed of a dsDNA (152kbp) nucleoprotein core • Core is surrounded by an icosahedral protein capsid • 100nm Capsid is enclosed in an outer envelope consisting of at least 8 glycoproteins. • Envelope spikes ~8 nm long • The virus requires a moist environment for survival. Subfamily Genus Common Name Alp ha herpesv ir inae Simp lexv irus HiliHerpes simplex virus - 1 (HSV-1) Herpes simplex virus - 2 (HSV-2) Varicellovirus Varicella-zoster virus (VZV) Betaherpesvirinae Cytomegalovirus Cytomegalovirus (CMV) Roseolovirus Human herpesvirus 6 (HHV-6) Human herpesvirus 7 (HHV-7) Gammaherpesvirinae Lymphocryptovirus Epstein-Barr virus (EBV) Rhadinovirus Human herpesvirus 8 (HHV-8) Cold sores are contagious sores caused by HSV‐1. • After primary infection, the viruses become latent in sensory ganglia. • Recurrence of cold sores occurs when viruses are reactivated and move to the epithelium.