Comparison of Effectiveness of Cefovecin, Doxycycline, And
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antibiotic Use Guidelines for Companion Animal Practice (2Nd Edition) Iii
ii Antibiotic Use Guidelines for Companion Animal Practice (2nd edition) iii Antibiotic Use Guidelines for Companion Animal Practice, 2nd edition Publisher: Companion Animal Group, Danish Veterinary Association, Peter Bangs Vej 30, 2000 Frederiksberg Authors of the guidelines: Lisbeth Rem Jessen (University of Copenhagen) Peter Damborg (University of Copenhagen) Anette Spohr (Evidensia Faxe Animal Hospital) Sandra Goericke-Pesch (University of Veterinary Medicine, Hannover) Rebecca Langhorn (University of Copenhagen) Geoffrey Houser (University of Copenhagen) Jakob Willesen (University of Copenhagen) Mette Schjærff (University of Copenhagen) Thomas Eriksen (University of Copenhagen) Tina Møller Sørensen (University of Copenhagen) Vibeke Frøkjær Jensen (DTU-VET) Flemming Obling (Greve) Luca Guardabassi (University of Copenhagen) Reproduction of extracts from these guidelines is only permitted in accordance with the agreement between the Ministry of Education and Copy-Dan. Danish copyright law restricts all other use without written permission of the publisher. Exception is granted for short excerpts for review purposes. iv Foreword The first edition of the Antibiotic Use Guidelines for Companion Animal Practice was published in autumn of 2012. The aim of the guidelines was to prevent increased antibiotic resistance. A questionnaire circulated to Danish veterinarians in 2015 (Jessen et al., DVT 10, 2016) indicated that the guidelines were well received, and particularly that active users had followed the recommendations. Despite a positive reception and the results of this survey, the actual quantity of antibiotics used is probably a better indicator of the effect of the first guidelines. Chapter two of these updated guidelines therefore details the pattern of developments in antibiotic use, as reported in DANMAP 2016 (www.danmap.org). -

Convenia, INN-Cefovecin Sodium
EMA/215997/2006 EMEA/V/C/000098 EPAR summary for the public CONVENIA cefovecin This document is a summary of the European Public Assessment Report. Its purpose is to explain how the assessment done by the Committee for Medicinal Products for Veterinary Use (CVMP) on the basis of the documentation provided, led to the recommendations on the conditions of use. This document cannot replace a face-to-face discussion with your veterinarian. If you need more information about your animal’s medical condition or treatment, contact your veterinarian. If you want more information on the basis of the CVMP recommendations, read the Scientific Discussion (also part of the EPAR). What is Convenia? Convenia contains cefovecin, an antibiotic which is given by injection (under the skin). It is used for dogs and cats. There are two vials in each pack of Convenia, one vial containing a powder, and one vial containing the diluent. The powder is dissolved in the diluent before use to make up a solution for injection. What is Convenia used for? Convenia is used to treat infections caused by certain specific bacteria (see the SPC for further details). It is generally given as a single injection, and the effect of the injection lasts for up to 14 days. Depending on the infection concerned, the injection can be repeated if necessary (up to three times). Convenia is used in dogs to treat skin and soft tissue infections; these are infections on the skin and in the layers just below the skin, such as wounds, abscesses and pyoderma (a skin infection with a rash and pustules). -

AMEG Categorisation of Antibiotics
12 December 2019 EMA/CVMP/CHMP/682198/2017 Committee for Medicinal Products for Veterinary use (CVMP) Committee for Medicinal Products for Human Use (CHMP) Categorisation of antibiotics in the European Union Answer to the request from the European Commission for updating the scientific advice on the impact on public health and animal health of the use of antibiotics in animals Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 29 October 2018 Adopted by the CVMP for release for consultation 24 January 2019 Adopted by the CHMP for release for consultation 31 January 2019 Start of public consultation 5 February 2019 End of consultation (deadline for comments) 30 April 2019 Agreed by the Antimicrobial Advice ad hoc Expert Group (AMEG) 19 November 2019 Adopted by the CVMP 5 December 2019 Adopted by the CHMP 12 December 2019 Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 An agency of the European Union © European Medicines Agency, 2020. Reproduction is authorised provided the source is acknowledged. Categorisation of antibiotics in the European Union Table of Contents 1. Summary assessment and recommendations .......................................... 3 2. Introduction ............................................................................................ 7 2.1. Background ........................................................................................................ -
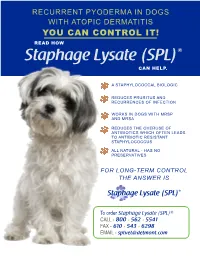
Staphylococcus Aureus Phage Lysate (SPL) Use for Control of Recurrent Eczematizing Pyoderma of Dogs with Atopic Dermatitis 2011 – by Dr
RECURRENT PYODERMA IN DOGS WITH ATOPIC DERMATITIS YOU CAN CONTROL IT! READ HOW Staphage Lysate (SPL)® CAN HELP. A STAPHYLOCOCCAL BIOLOGIC REDUCES PRURITUS AND RECURRENCES OF INFECTION WORKS IN DOGS WITH MRSP AND MRSA REDUCES THE OVERUSE OF ANTIBIOTICS WHICH OFTEN LEADS TO ANTIBIOTIC RESISTANT STAPHYLOCOCCUS ALL NATURAL - HAS NO PRESERVATIVES FOR LONG-TERM CONTROL THE ANSWER IS Staphage Lysate (SPL)® To order Staphage Lysate (SPL)® CALL - 800 .562 .5541 FAX - 610 .543 .6298 EMAIL - [email protected] Abstract from Masters Thesis - Staphylococcus Aureus Phage Lysate (SPL) use for control of recurrent eczematizing pyoderma of dogs with atopic dermatitis 2011 – By Dr. Suzana Evelyn Bahr Solomon – Pontifica Universidade Católica do Paraná, São José dos Pinhais, Paraná, Brazil Recurrent staphylococcal infections are The aim of this study was to evaluate whether frequent in dogs with atopic dermatitis. the use of Staphylococcus aureus Phage Several factors such as decrease of epidermal Lysate (Staphage Lysate (SPL)®), a bacterin barrier function, decrease in production of obtained from S. aureus used in vaccine antimicrobial peptides and increased protocol, can minimize the symptoms colonization and adherence of bacteria to of recurrent pyoderma and increase the keratinocytes seem to combine to make interval between episodes in atopic dogs. bacterial pyoderma refractory to treatment. Twelve dogs with a history of recurrent Systemic antibiotic therapy in the short-term is bacterial pyoderma received SPL® at effective for the treatment of episodes and with increasing intervals for twenty three weeks. pulse therapy, might contribute to long-term An efficacy rate of 83.33% for the control control. However, in addition to undesirable of pruritus and regression of lesions was side-effects, microbial resistance has become observed. -

(Cefovecin Sodium) Lowered Albumin Values Due to Interference with Certain Testing Methods
Positive direct Coombs’ test results and false positive reactions for glucose in the urine have been reported during treatment with some cephalosporin antimicrobials. Cephalosporin antimicrobials may also cause falsely elevated urine protein determinations. Some antimicrobials, including cephalosporins, can cause (cefovecin sodium) lowered albumin values due to interference with certain testing methods. Occasionally, cephalosporins and NSAIDs have been associated with myelotoxicity, thereby creating a 4 Antimicrobial for Subcutaneous Injection in Dogs and Cats Only toxic neutropenia . Other hematological reactions seen with cephalosporins include neutropenia, anemia, hypoprothrombinemia, thrombocytopenia, prolonged prothrombin time (PT) and partial thromboplastin time CAUTION: Federal (USA) law restricts this drug to use by or on the order of a licensed veterinarian. (PTT), platelet dysfunction and transient increases in serum aminotransferases. DESCRIPTION: Cefovecin sodium is a semi-synthetic broad-spectrum antibacterial agent from the ADVERSE REACTIONS: cephalosporin class of chemotherapeutic agents. Cefovecin is the non-proprietary designation for (6R,7R)-7- Dogs [[(2Z)-(2-amino-4-thiazolyl)(methoxyimino)acetyl]amino]-8-oxo-3-[(2S)-tetrahydro-2-furanyl]-5-thia-1- A total of 320 dogs, ranging in age from 8 weeks to 19 years, were included in a field study safety analysis. azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid, monosodium salt. Adverse reactions reported in dogs treated with CONVENIA and the active control are summarized in Table -

Higher Prevalence of Extended-Spectrum Cephalosporin
antibiotics Article Higher Prevalence of Extended-Spectrum Cephalosporin-Resistant Enterobacterales in Dogs Attended for Enteric Viruses in Brazil Before and After Treatment with Cephalosporins Marília Salgado-Caxito 1,2,* , Andrea I. Moreno-Switt 2,3, Antonio Carlos Paes 1, Carlos Shiva 4 , Jose M. Munita 2,5 , Lina Rivas 2,5 and Julio A. Benavides 2,6,7,* 1 Department of Animal Production and Preventive Veterinary Medicine, School of Veterinary Medicine and Animal Science, Sao Paulo State University, Botucatu 18618000, Brazil; [email protected] 2 Millennium Initiative for Collaborative Research on Bacterial Resistance (MICROB-R), Santiago 7550000, Chile; [email protected] (A.I.M.-S.); [email protected] (J.M.M.); [email protected] (L.R.) 3 Escuela de Medicina Veterinaria, Pontificia Universidad Católica de Chile, Santiago 8940000, Chile 4 Faculty of Veterinary Medicine and Zootechnics, Universidad Cayetano Heredia of Peru, Lima 15102, Peru; [email protected] 5 Genomics and Resistant Microbes Group, Facultad de Medicina Clinica Alemana, Universidad del Desarrollo, Santiago 7550000, Chile 6 Departamento de Ecología y Biodiversidad, Facultad de Ciencias de la Vida, Universidad Andrés Bello, Santiago 8320000, Chile 7 Centro de Investigación para la Sustentabilidad, Facultad de Ciencias de la Vida, Universidad Andrés Bello, Santiago 8320000, Chile Citation: Salgado-Caxito, M.l.; * Correspondence: [email protected] (M.S.-C.); [email protected] (J.A.B.) Moreno-Switt, A.I; Paes, A.C.; Shiva, C.; Munita, J.M; Rivas, L.; Abstract: The extensive use of antibiotics is a leading cause for the emergence and spread of antimicro- Benavides, J.A Higher Prevalence of Extended-Spectrum Cephalosporin- bial resistance (AMR) among dogs. -

Treating Pyoderma Is NOT What It Used to Be Vetgirl Final
Helpful Q:A from the VETgirl-Zoetis webinar “Treating pyoderma is NOT what it used to be” with Dr. Valerie A. Fadok, DVM, PhD, Diplomate, ACVD (All answers are provided by the speaker). Cytology: A few of our participants made the comment that they use pipettes to put their stain on the slides. They have no dunking and they only require one set of stains this way. Sounds good! Some hospitals’ cytology fees are per site. If all lesions are visibly similar and one cytology is performed, will it be accurate? This is a tough question. In general, if all lesions are epidermal collarettes and you find some good cocci in one, the probability is high that the lesions are quite similar. In atopic dogs, though, they may have yeast around their muzzle, on their feet, and up under the claw along with a classic pyoderma on the body. The patient will need to be treated for both, so at least 2 cytologies would needed here. At our practice, we charged the same fee for up to 3 cytologies. Pyoderma How contagious is S. schleiferi from animals to people? We don’t really know, to tell you the truth. Please see this blog written by Dr. Scott Weese at U. Guelph. It is superb. Here is a hyperlink. https:// www.wormsandgermsblog.com/2011/12/articles/animals/dogs/staph-schleiferi-in- dogs/ What dosage of cephalosporin do I recommend? When I use cefovecin (Convenia®), I use the label dose, which is 8 mg/kg. When I use cefpodoxime (Simplicef®) I use 5-10 mg/kg every 24 hrs. -

Chronic Upper Respiratory Tract Disease in A
RED LIGHT, GREEN LIGHT PEER REVIEWED Margie Scherk, DVM, DABVP (Feline) catsINK Chronic Upper Respiratory Vancouver, British Columbia, Canada Tract Disease in a Cat SAM, AN 11-YEAR-OLD, NEUTERED PERSIAN CAT, has an 8-year history of recur- ring and progressively worsening chronic upper respiratory disease. He is presented because of loud breathing and head shaking while sneezing nonproductively over the past 3 days. The patient is reportedly withdrawn and less interested in eating but is still drinking. The patient has received amoxicillin previously (most recently, 5 weeks ago); he also receives glucosamine with chondroitin sulfate for arthritis. His weight is stable and BCS is 4/9. No oral lesions are seen. TPR is normal, but tracheal- auscultated sounds are harsh. CBC reveals stress lymphopenia and mild monocyto- sis. Serum chemistry values are within normal reference intervals, and urinalysis is unremarkable. RED = do not use YELLOW = use with caution, GREEN = safe & effective moderately effective Amoxicillin–clavulanic acid RED YELLOW GREEN Azithromycin RED YELLOW GREEN Pradofloxacin Which of the RED YELLOW GREEN Doxycycline monohydrate/hyclate following RED YELLOW GREEN Cefovecin drugs would be RED YELLOW GREEN Famciclovir appropriate in RED YELLOW GREEN the management Zidovudine RED YELLOW GREEN of this patient? Mirtazapine RED YELLOW GREEN Based on the information Cyproheptadine provided, how would you RED YELLOW GREEN Meloxicam grade the following drugs RED YELLOW GREEN and why? Prednisolone RED YELLOW GREEN L-Lysine RED YELLOW GREEN Turn the page and Probiotics compare your results h RED YELLOW GREEN BCS = body condition score, CBC = complete blood count, TPR = temperature, pulse, respiration Plumb’s Therapeutics Brief January 2016 23 RED LIGHT, GREEN LIGHT PEER REVIEWED Did you answer? Amoxicillin–clavulanic acid | CORRECT RESPONSE The following represents Amoxicillin–clavulanic acid, a β-lactam antibiotic, is used for elimination of infection and clinical signs associated with Chlamydophila spp. -

Concept Paper
Concept Paper: Potential Approach for Ranking of Antimicrobial Drugs According to Their Importance in Human Medicine: A Risk Management Tool for Antimicrobial New Animal Drugs Introduction This concept paper discusses a potential approach to considering the human medical importance of antimicrobial drugs when assessing and managing antimicrobial resistance risks associated with the use of antimicrobial drugs in animals. In 2003, FDA established a list ranking antimicrobial drugs according to their relative importance in human medicine primarily for the purpose of supporting a qualitative risk assessment process outlined in agency guidance. It was envisioned by the Agency at the time the current medical importance rankings list was published that it would periodically reassess the rankings to align with contemporary science and current human clinical practices. To that end, this paper describes a potential revised process for ranking antimicrobial drugs according to their relative importance in human medicine, potential revised criteria to determine the medical importance rankings, and the list of antimicrobial drug medical importance rankings that would result if those criteria were to be used. Disclaimer: This concept paper is for discussion purposes only. The intent of this concept paper is to obtain public comment and early input on a potential approach to consider the human medical importance of antimicrobial drugs when assessing and managing antimicrobial resistance risks associated with the use of antimicrobial drugs in animals. This concept paper does not contain recommendations and does not constitute draft or final guidance by the Food and Drug Administration. It should not be used for any purpose other than to facilitate public comment. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0150995 A1 Taft, III Et Al
US 2015O150995A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0150995 A1 Taft, III et al. (43) Pub. Date: Jun. 4, 2015 (54) CONJUGATED ANTI-MICROBIAL Publication Classification COMPOUNDS AND CONUGATED ANT-CANCER COMPOUNDS AND USES (51) Int. Cl. THEREOF A647/48 (2006.01) A63/546 (2006.01) (71) Applicant: PONO CORPORATION, Honolulu, HI A633/38 (2006.01) (US) (52) U.S. Cl. CPC ........... A61K47/480.15 (2013.01); A61K33/38 (72) Inventors: Karl Milton Taft, III, Honolulu, HI (2013.01); A61 K3I/546 (2013.01) (US); Jarred Roy Engelking, Honolulu, HI (US) (57) ABSTRACT (73) Assignee: PONO CORPORATION, Honolulu, HI Disclosed herein are synthesis methods for generation of (US) conjugated anti-microbial compounds and conjugated anti cancer compounds. Several embodiments, related to the uses (21) Appl.ppl. NNo.: 14/418,9079 of Such compoundsp in the treatment of infections, in particu lar those caused by drug-resistant bacteria. Some embodi (22) PCT Filed: Aug. 9, 2013 ments relate to targeting cancer based on the metabolic sig (86). PCT No.: PCT/US2O13/O54391 nature of tumor cells. S371 (c)(1), (2) Date: Jan. 30, 2015 NH Related U.S. Application Data O Ag" (60) Provisional application No. 61/742,443, filed on Aug. B-Lactam Silver Ion 9, 2012, provisional application No. 61/742,444, filed on Aug. 9, 2012. O O O O O O HSONaNO -pE (CHO)2SO2 OEt Br2 OEt 2W4 OH NOMe 1 2 3 Q Q H.N.S NH, NHT chicci -VV653C(CH) NaOH Bra-oe 2 2 S1N (C6H5)3C- SNN a NOMe MeO -co. -

Antibiotic Classes
Penicillins Aminoglycosides Generic Brand Name Generic Brand Name Amoxicillin Amoxil, Polymox, Trimox, Wymox Amikacin Amikin Ampicillin Omnipen, Polycillin, Polycillin-N, Gentamicin Garamycin, G-Mycin, Jenamicin Principen, Totacillin, Unasyn Kanamycin Kantrex Bacampicillin Spectrobid Neomycin Mycifradin, Myciguent Carbenicillin Geocillin, Geopen Netilmicin Netromycin Cloxacillin Cloxapen Paromomycin Dicloxacillin Dynapen, Dycill, Pathocil Streptomycin Flucloxacillin Flopen, Floxapen, Staphcillin Tobramycin Nebcin Mezlocillin Mezlin Nafcillin Nafcil, Nallpen, Unipen Quinolones Oxacillin Bactocill, Prostaphlin Generic Brand Name Penicillin G Bicillin L-A, First Generation Crysticillin 300 A.S., Pentids, Flumequine Flubactin Permapen, Pfizerpen, Pfizerpen- Nalidixic acid NegGam, Wintomylon AS, Wycillin Oxolinic acid Uroxin Penicillin V Beepen-VK, Betapen-VK, Piromidic acid Panacid Ledercillin VK, V-Cillin K Pipemidic acid Dolcol Piperacillin Pipracil, Zosyn Rosoxacin Eradacil Pivampicillin Second Generation Pivmecillinam Ciprofloxacin Cipro, Cipro XR, Ciprobay, Ciproxin Ticarcillin Ticar Enoxacin Enroxil, Penetrex Lomefloxacin Maxaquin Monobactams Nadifloxacin Acuatim, Nadoxin, Nadixa Generic Brand Name Norfloxacin Lexinor, Noroxin, Quinabic, Aztreonam Azactam, Cayston Janacin Ofloxacin Floxin, Oxaldin, Tarivid Carbapenems Pefloxacin Peflacine Generic Brand Name Rufloxacin Uroflox Imipenem, Primaxin Third Generation Imipenem/cilastatin Balofloxacin Baloxin Doripenem Doribax Gatifloxacin Tequin, Zymar Meropenem Merrem Grepafloxacin Raxar Ertapenem -
Methicillin-Resistant Staphylococci in Animals: Veterinary and Public Health Implications
Final Program and Abstracts Final Program 3rd ASM-ESCMID Conference on Methicillin-resistant Staphylococci in Animals: Veterinary and Public Health Implications November 4 – 7, 2013 Copenhagen, Denmark © 2013 American Society for Microbiology 1752 N Street, N.W. Washington, DC 20036-2904 Phone: 202-737-3600 World Wide Web: www.asm.org All Rights Reserved Printed in the United States of America Table of Contents ASM Conferences Information ...................................... 2 Conference Organization ............................................... 3 Acknowledgments .......................................................... 3 General Information ....................................................... 4 Travel Grants .................................................................. 6 Scientific Program .......................................................... 7 Abstracts for Speakers ................................................. 13 Abstracts for Posters .................................................... 38 Index .......................................................................... 112 3rd ASM-ESCMID Conference on Methicillin-resistant Staphylococci in Animals 1 ASM Conferences Committee William E. Goldman, Chair Lora Hooper University of North Carolina, Chapel Hill University of Texas Southwestern Medical Center Sean Whelan, Vice Chair Harvard Medical School Gary Procop Cleveland Clinic Victor DiRita University of Michigan Curtis Suttle University of British Columbia Joanna Goldberg Emory University ASM Conferences Mission