The Union Labor Life Insurance Company (“Union Labor Life”) Is Committed to Providing Efficient and Effective Customer Service to Its Clients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Life Insurance
7LIFE INSURANCE People buy life insurance to protect their dependents INDIVIDUAL LIFE INSURANCE against financial hardship when the insured person, the Individual life is the most widely used form of life policyholder, dies. Many life insurance products also allow insurance protection, accounting for 58 percent of all life policyholders to accumulate savings that can be used in insurance in force in the United States at year-end 2017 a time of financial need. Most American families depend (Table 7.1). Typically purchased through life insurance on life insurance to provide this economic protection: 90 agents, this insurance is issued under individual policies million American families rely on life insurers’ products with face amounts as low as $1,000, although larger for financial and retirement security.* minimum amounts are more typical in today’s market. Americans purchased $3.1 trillion of new life insurance While individual life is principally used for family coverage in 2017, a 5.2 percent increase from 2016. By the protection, it also is widely used for business purposes. end of 2017, total life insurance coverage in the United A business may purchase life insurance to protect against States was $20.4 trillion, an increase of .5 percent from the economic loss that would result from the death of the 2016 (Table 7.1). owner or a key employee. Three types of life insurance policies predominate the Individual life insurance protection in the United States market. Individual insurance is underwritten separately totaled $12 trillion at the end of 2017 and has grown at for each individual who seeks insurance protection. -

Trade Union Benefits and Our Social Insurance Problems by Rainard B
14 TRADE UNION BENEFITS TRADE UNION BENEFITS AND OUR SOCIAL INSURANCE PROBLEMS BY RAINARD B. ROBBINS Trade unions have, for half a century, paid insurance benefits, quasi and pseudo insurance benefits, along with many other forms of allowances to which the term "insurance" is entirely foreign. An examination of the methods and experiences of trade unions will teach members of this body nothing in the way of actuarial theory. In fact, from the standpoint of an actuary the study of what trade unions have done is a good way of finding out what not to do. Nevertheless, this paper is written to review, very briefly, some of the characteristics of trade union benefit schemes, with the thought that we may learn something from these activities which will be of use in dealing with problems of importance to us as good citizens, if not as company actuaries. Trade union organizations are formed for the purpose of collec- tive bargaining in order to improve wages and working condi- tions. The basic units of union organizations are quite local and almost without exception a union is in existence for only a rela- tively short time before the members agree to unite in helping the less fortunate of their number by the payment of benefits in case of the occurrence of various contingencies, such as sick- ness, accident, death and old age. These are in addition to other benefits such as those paid in case of labor disturbances and unemployment. One of the mo~t common trade union benefits is the death benefit. Probably the simplest method of handling this benefit is to have either a tentative agreement or a hard and fast rule that each member shall pay a certain amount, say $1.00 when- ever a member dies, and that the total amount collected shall be paid to the beneficiary. -

A Brief History of Reinsurance by David M
Article from: Reinsurance News February 2009 – Issue 65 A BRIEF HISTORY OF REINSURANCE by David M. Holland, FSA, MAAA goods over a number of ships in order to reduce the risk from any one boat sinking.2 • In 1601, during the reign of Queen Elizabeth I, the English Parliament enacted “AN ACTE CONCERNINGE MATTERS OF ASSURANCES, AMONGSTE MARCHANTES,” which states: “… by meanes of whiche Policies of Assurance it comethe to passe, upon the losse or perishinge of any Shippe there followethe not the undoinge of any Man, but the losse lightethe rather easilie upon many, then heavilie upon fewe. …”3 • Edwin Kopf, FCAS, in his 1929 paper “Notes on Origin and Development of Reinsurance”4 translates from a German text by Ehrenberg as follows: einsurance is basically insurance for insur- ance companies. Park, writing in 1799, “Reinsurance achieves to the utmost more colorfully stated: extent the technical ideal of every branch R of insurance, which is actually to effect (1) “RE-ASSURANCE, as understood by the law of the atomization, (2) the distribution and England, may be said to be a contract, which the (3) the homogeneity of risk. Reinsurance first insurer enters into, in order to relieve himself is becoming more and more the essential from those risks which he has incautiously under- element of each of the related insurance taken, by throwing them upon other underwriters, branches. It spreads risks so widely and who are called re-assurers.”1 effectively that even the largest risk can be accommodated without unduly burden- 5 In order for commerce to flourish, there has to be a ing any individual.” way to deal with large financial risks. -

Insurance and the Legal Process
Insurance and the Legal Process Table of Contents Chapter 1: Philosophy of Law ................................................................................................................................. 1 Purpose of the Law .............................................................................................................................................. 1 The Legal System Develops ................................................................................................................................ 2 History of Law ...................................................................................................................................................... 7 Classes of Law .................................................................................................................................................. 13 Chapter 2: The U.S. Legal System ....................................................................................................................... 15 The Federal Court System ................................................................................................................................. 16 A Trip Through the Court System ...................................................................................................................... 19 Criminal Law ...................................................................................................................................................... 24 Insurance and Statutory Liability ...................................................................................................................... -

2019 Insurance Fact Book
2019 Insurance Fact Book TO THE READER Imagine a world without insurance. Some might say, “So what?” or “Yes to that!” when reading the sentence above. And that’s understandable, given that often the best experience one can have with insurance is not to receive the benefits of the product at all, after a disaster or other loss. And others—who already have some understanding or even appreciation for insurance—might say it provides protection against financial aspects of a premature death, injury, loss of property, loss of earning power, legal liability or other unexpected expenses. All that is true. We are the financial first responders. But there is so much more. Insurance drives economic growth. It provides stability against risks. It encourages resilience. Recent disasters have demonstrated the vital role the industry plays in recovery—and that without insurance, the impact on individuals, businesses and communities can be devastating. As insurers, we know that even with all that we protect now, the coverage gap is still too big. We want to close that gap. That desire is reflected in changes to this year’s Insurance Information Institute (I.I.I.)Insurance Fact Book. We have added new information on coastal storm surge risk and hail as well as reinsurance and the growing problem of marijuana and impaired driving. We have updated the section on litigiousness to include tort costs and compensation by state, and assignment of benefits litigation, a growing problem in Florida. As always, the book provides valuable information on: • World and U.S. catastrophes • Property/casualty and life/health insurance results and investments • Personal expenditures on auto and homeowners insurance • Major types of insurance losses, including vehicle accidents, homeowners claims, crime and workplace accidents • State auto insurance laws The I.I.I. -

Life Insurance Plan Bookletpdf
SUBJECT TO STATE FILING The Regents of the University of California Employee Term Life Coverage Basic, Core and Supplemental Plans Dependents Term Life Coverage Basic and Expanded Plans SUBJECT TO STATE FILING Disclosure Notice FOR ARKANSAS RESIDENTS Prudential’s Customer Service Office: The Prudential Insurance Company of America Prudential Group Life Claim Division P.O. Box 8517 Philadelphia, PA 19176 1-800-524-0542 If Prudential fails to provide you with reasonable and adequate service, you may contact: Arkansas Insurance Department Consumer Services Division 1200 West Third Street Little Rock, Arkansas 72201-1904 1-800-852-5494 FOR CALIFORNIA RESIDENTS Prudential’s Address: The Prudential Insurance Company of America 751 Broad Street Newark, New Jersey 07102 Customer Service Office: The Prudential Insurance Company of America Prudential Group Life Claim Division P.O. Box 8517 Philadelphia, Pennsylvania 19176 1-800-524-0542 Should you have a dispute concerning your coverage you should contact Prudential first. If the dispute is not resolved, you may contact the California Department of Insurance at the following address and phone number: California Department of Insurance Consumer Services Division 300 South Spring Street Los Angeles, California 90013 1-800-927-HELP http://www.insurance.ca.gov/01-consumers/ SUBJECT TO STATE FILING FOR FLORIDA RESIDENTS The benefits of the policy providing your coverage are governed by the law of a state other than Florida. FOR IDAHO RESIDENTS If you need the assistance of the governmental agency that -

Cross-Border Life Insurance: Differing Definitions in an Age of International Tax Reporting
Article from: Taxing Times May 2014 – Volume 10, Issue 2 CROSS-BORDER LIFE INSURANCE: DIFFERING DEFINITIONS IN AN AGE OF INTERNATIONAL TAX REPORTING By Philip Friedlan and John T. Adney This article was previously published in Insurance Planning insurers – a universal life insurance policy (the “Cdn UL and is being republished with the permission of Federated Policy”) and a ten-year level premium renewable term policy Press. that has no cash value (the “Cdn Term Policy”). Each of these policies is an “exempt policy”5 and is not registered as a de- ferred income plan. Since each policy is an exempt policy, INTRODUCTION income will only arise on the disposition of the interest in the We wrote several articles in 2004-2005 that dealt with the policy.6 In the second case, a U.S. citizen moves to Canada tax consequences relating to life insurance policies owned owning and being the life insured under a fixed, non-variable by individuals when they moved across the Canadian-U.S. UL policy (the “US UL Policy”) and a ten-year level premium border.1 Since that time and until recently, much of the cur- renewable term policy issued by a U.S. carrier (again, with no rent Canadian2 and the U.S.3 tax legislation as it relates to the cash value) (the “US Term Policy”). Neither policy is con- taxation of holders of life insurance policies has basically nected with a tax-qualified retirement plan. remained unchanged. CANADIAN TAX TREATMENT OF THE MOVE However, the 2013 Canadian Federal Budget proposed SOUTH changes in the rules applicable to leveraged insured annuity A Canadian resident is taxed on the person’s worldwide in- arrangements and so called 10/8 policies that are now law. -
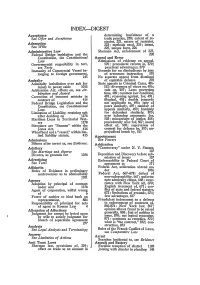
Index-Digest
INDEX-DIGEST Acceptance determining lawfulness of a See Offer and Acceptance trade practice, 220; extent of re- straint, 221, nature of restraint, Ademption 223; methods used, 224; intent, See Wills 225, unique facts, 226 Administrative Law Sherman Act, enforcement of 227, Federal Bridge legislation and the 230 Constitution, see Constitutional Appeal and Error Law Admissions of evidence on appeal, Governmental resposibility in tort, 570; procedural reform in, 570; see Torts practical advantages, 570 Immunity of Commercial Vessel be- Grounds for on disobedience by jury longing to foreign government, of erroneous instruction 570 145 No separate appeal from dismissal Amiralty of equitable defense 278 Admiralty jurisdiction over suit for State appeals in Criminal Cases, 486- injury to power cable 1015 512: divergence of views on, 486; Arbitration Act, effects on, see Ar- rule on, 487; Laws governing bitration and Award time, 489; common law condition, Correction of innocent mistake in 491; reasoning against, for, 491 ; contract of 414 illogical, 493; double jeopardy Federal Bridge Legislation and the not applicable to, 496; jury of Constitution, see Constitutional peers similarly, 497; number of Law. appeals similarly, 499; hardship Limitation of Liability, retaining suit for defendent similarly, 500; after deciding on 1176 over balancing arguments for, Maritime Liens in Territorial Wat- 503; miscarriage of justice, 508; ers 1178 procedurally wise for, 507; moral Stevedore are "Seamen" within the effect of, 508; supervision of Jones Act, 414 counsel for defense by, 510; un- Wharfboat not a "vessel," within lim- prejudiced bench by, 511 ited liability statute, 415 Appointment Admissions See Powers Silence after arrest as, see Evidence. -

Group Life Insurance: Its Legal Aspects
GROUP LIFE INSURANCE: ITS LEGAL ASPECTS FRANK W. HANBT* NATURE AND HISTORY Definitions of group insurance are usually nothing more than summaries of the common attributes of this device.' If one or more of the attributes usually present and included in the definitions were missing, still the device would be group insur- ance, just as a man with only one leg is still a man. Which of the usual attributes of group insurance are essential characteristics may be a matter of opinion; but it is suggested that any form of insurance which by a single policy gives insurance to individuals belonging to a definite group already in existence is group insurance. By far the most common type of group on which this form of insurance is in fact written is the group formed by the employees of a single employer. It is this fact which makes group insurance an important agency for the welfare of wage earners. Group insurance as above identified appeared in litigation as early as 1892. In the case of Enright v. Standard Life & Accident Insurance Company2 was involved an accident policy issued by the insurance company to a railroad, covering such of * LL.B., 1924, LL.M., 1929, A.B., 1929, University of Minnesota; S. J. D., 1931, Harvard University. General law practice, 1924-1929. Instructor in Law, University of Minnesota, 1929-1930; Fairchild Re- search Fellow, Harvard Law School, 1930-1931; Associate Professor of Law, University of North Carolina, 1931-; Associate Utilities Commissioner, North Carolina, 1934. Author of Control of Public Utilities in Minnesota (1932) 16 Minnesota Law Review, 457 (1932); Control of Electric Rates in North Carolina (1934) 12 North Carolina Law Review, 289; and other articles and comments. -

Consumer's Guide to Life Insurance
Consumer’s Guide to LIFE INSURANCE LOUISIANA DEPARTMENT OF INSURANCE Jim Donelon, Commissioner 1 A message from Commissioner of Insurance Jim Donelon Recent studies show that, while individuals may think they have adequate life insurance coverage, survivors often find that is not the case. Most people know they need some life insurance, they just don’t know how much or what kind. In this Consumer’s Guide, we offer advice to help you find a policy that meets your needs. Life insurance policies are based on some basic tenets that remain much the same year after year. Some time back, a National Association of Insurance Commissioners committee, chaired by Louisiana, put together the fundamentals set forth in this guide. We hope you find this guide useful in making informed decisions regarding life insurance. Louisiana Department of Insurance 2012 This public document is published at a total cost of $1,993.78. 5,000 copies of this public document were published in this fifth printing at a cost of $1,950. The total cost of all printings of this document including reprints is $8,201.16. This document was published by Moran Printing, 5425 Florida Blvd., Baton Rouge, LA 70806 to inform consumers about their life insurance options under authority of the Division of Administration. This material was printed in accordance with standards for printing by State Agencies established in R.S. 43:31. Printing of this material was purchased in accordance with the provisions of Title 43 of the Louisiana Revised Statutes. 2 Buying Life Insurance When you buy life insurance, you want coverage that fits your needs. -

Evolution of Life Insurance Industry Throughout the World
RECORD OF SOCIETY OF ACTUARIES 1990 VOL. 16 NO. 4A EVOLUTION OF LIFE INSURANCE INDUSTRY THROUGHOUT THE WORLD Moderator: ROBERT L. COLLETI" Panelists: NOEL J. ABKEMEIER EDWARD JOHN BONACH DEMOS K. PAPASAVVAS* Recorder: DAVID NOLIN COOK o What does the industry look like in various regions of the world: Western Europe, Eastern Europe, Far East and Latin America. o Why has the industry evolved so differently in different places? -- Regulation -- Taxation -- Political climate -- Demographics -- Culture o What is the prognosis? Will the life industry ever globalize? Where are the areas of greatest opportunity? MR. ROBERT L. COLLE'Iq': Our first panelist is Demos Papasawas. Demos was born in Cyprus in 1956. He went to the U.K. in 1974 to study at the London School of Economics. He graduated in 1977 and joined Mercantile & General Reinsurance Company (M&G) as an actuarial trainee. He planned to stay in the U.K. temporarily, but on receiving his Fellowship in the Institute, he decided to reside permanently in the U.K. During his time at the M&G, he gained experience in all types of individual and group life and health benefits, in both the U.K. and overseas. He had actuarial responsi- bility at M&G for U.K. clients outside the home countries, as well as for clients in Greece, Cyprus, and the Middle East. He is a partner in Bacon and Woodrow Consult- ing Actuaries. He is a member of their European team, specializing in Spain, Portugal, Greece, and Switzerland. Since joining Bacon and Woodrow, Demos has carried out a number of appraisals of European companies and has participated in the development of products and many other projects for companies on the continent. -

Colonial Term Life Insurance
Term Life Insurance How secure is your family’s future without you? The last thing you or your family should have to worry about is the financial cost of losing a loved one. Funeral expenses, medical bills and taxes are just the tip of the iceberg. How would they cover ongoing living expenses such as the mortgage, healthcare and utilities? Plan for the future with Colonial Life’s Term Life insurance. What are the advantages of Term Life Insurance? l Offers level death benefit. l Offers a lower cost option compared with cash value insurance. l Provides coverage for specified periods of time, which can be during high-need years. l Benefit is typically paid tax-free to your beneficiaries. What benefits and features are included? l Guaranteed premiums that do not increase during the term unless you receive an accelerated death benefit. l Guaranteed renewable to age 95 as long as premiums are paid when due. l Convertible to cash value insurance. l Portability allows you to take it with you if you change jobs or retire. l Includes an Accelerated Death Benefit. My Coverage Worksheet (For use with your Colonial Life Benefits Counselor) How much coverage do you need? You Spouse $_________________face amount $_________________face amount Select the term period: Select the term period: 10-year term period 10-year term period 20-year term period 20-year term period 30-year term period 30-year term period Select any optional riders: Spouse Term Life Rider $________________face amount for __________ year term period Children(s) Term Life Rider $________________face amount for __________ year term period Waiver of Premium Benefit Rider Accidental Death Benefit Rider Term Life 1000 Life Term How much will it cost? Your cost will vary based on the level of coverage you select.