Corneal Ulcer-Infiltrate Associated with Soft Contact Lens Use Following Penetrating Keratoplasty*
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Neurotrophic Keratopathy and Diabetes Mellitus a Lockwood Et Al 838
Eye (2006) 20, 837–839 & 2006 Nature Publishing Group All rights reserved 0950-222X/06 $30.00 www.nature.com/eye 1 1 2 Neurotrophic A Lockwood , M Hope-Ross and P Chell CASE SERIES keratopathy and diabetes mellitus Abstract no history of previous corneal trauma or herpes simplex infection. Ocular examination revealed Diabetes mellitus is frequently associated a best-corrected visual acuity of 6/12 in both with microvascular complications such as eyes. There was an epithelial irregularity retinopathy, nephropathy, and peripheral extending across the inferonasal quadrant of the neuropathy. Neurotrophic keratopathy occurs right cornea. A diagnosis of exposure in response to a neuropathy of the ophthalmic keratopathy was made. She was treated with division of the trigeminal nerve. Rarely has artificial tears and a month later the epithelium diabetic neurotrophic keratopathy been had healed. A year later, an epithelial defect in described. This paper discusses the the same area was seen at follow-up. Again she ophthalmic histories of three patients who was asymptomatic and the visual acuity was presented with diabetic neurotrophic unchanged. Decreased corneal sensation was keratopathy. In one patient the corneal noted using a cotton swab to touch the ulceration was the sole presenting feature of peripheral and central cornea. A diagnosis of his diabetes. We discuss the need for increased diabetic neurotrophic keratopathy was made. vigilance in the ophthalmic community for She was treated with ocular lubricants. After suspecting diabetes in patients with 6 months, the defect had increased in size to unexplained corneal epithelial disease. 5.5 mm. There was associated corneal Eye (2006) 20, 837–839. -
Iol Calculations for Patients with Keratoconus
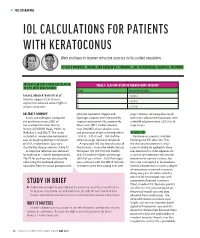
s THE LITERATURE IOL CALCULATIONS FOR PATIENTS WITH KERATOCONUS Work continues to improve refractive accuracy in this patient population. BY ALICE ROTHWELL, MBCHB, AND ANDREW M.J. TURNBULL, BM, PGCERTMEDED, PGDIPCRS, FRCOPHTH INTRAOCULAR LENS POWER CALCULATION TABLE 1. CLASSIFICATION OF KERATOCONUS SEVERITY IN EYES WITH KERATOCONUS Stage Keratometry Reading Savini G, Abbate R, Hoffer KJ, et al1 1 ≤ 48.00 D Industry support: K.J.H. licenses 2 > 48.00 D registered trademark name Hoffer to various companies 3 > 53.00 D ABSTRACT SUMMARY spherical equivalent. Myopic and stage 1 disease. Accuracy decreased Savini and colleagues compared hyperopic surprises were indicated by with more advanced keratoconus, with the prediction errors (PEs) of negative and positive PEs, respectively. a MedAE of greater than 2.50 D in all five standard formulas: Barrett Mean error (ME), median absolute stage 3 eyes. Universal II (BUII), Haigis, Hoffer Q, error (MedAE), mean absolute error, Holladay 1, and SRK/T. The study and percentage of eyes achieving within DISCUSSION included 41 consecutive keratoconic ±0.50 D, ±0.75 D, and ±1.00 D of the Keratoconus presents multiple eyes undergoing phacoemulsification refractive target were also calculated. challenges to IOL selection. First, and IOL implantation. Eyes were A hyperopic ME was found across all the standard keratometric index classified by disease severity (Table 1). five formulas. Across the whole dataset, cannot reliably be applied to these A subjective refraction was obtained the lowest ME (0.91 D) and MedAE eyes because this index depends on for each eye at 1 month postoperatively. (0.62 D) and the highest percentage a normal ratio between the anterior The PE for each eye was calculated by (36%) of eyes within ±0.50 D of target and posterior corneal surfaces, but subtracting the predicted spherical were achieved with the SRK/T formula. -

Analysis of Human Corneal Igg by Isoelectric Focusing
Investigative Ophthalmology & Visual Science, Vol. 29, No. 10, October 1988 Copyright © Association for Research in Vision and Ophthalmology Analysis of Human Corneal IgG by Isoelectric Focusing J. Clifford Woldrep,* Robin L. Noe,f and R. Doyle Stulringf Parameters which regulate the localization and retention of IgG within the corneal stroma are complex and poorly understood. Although multiple factors are involved, electrostatic interactions between IgG and anionic corneal tissue components, ie, proteoglycans (PG) and glycosaminoglycans (GAG) may regulate the distribution of antibodies within the corneal stroma. Isoelectric focusing (IEF) and blotting analysis of IgG revealed a restricted pi profile for both central and peripheral regions of the normal cornea. Similar analysis of pathological corneas from keratoplasty specimens in Fuchs' dys- trophy and keratoconus reveal a variable IEF profile. In the majority of keratoplasty specimens from patients with corneal edema or graft rejection, there was generally little or no IgG detectable. These results suggest that in edematous corneas where there is altered PG/GAG in the stroma and modified fluid dynamics, there is a concomitant loss of IgG. These findings may have implications for immuno- logic surveillance and protection of the avascular cornea. Invest Ophthalmol Vis Sci 29:1538-1543, 1988 The humoral immune system plays an important the soluble plasma proteins through ionic interac- role in mediating immunologic surveillance and pro- tions. The PGs and GAGs have long been known to -
Management Modalities for Keratoconus an Overview of Noninterventional and Interventional Treatments
REFRACTIVE SURGERY FEATURE STORY EXCLUSIVE ONLINE CONTENT AVAILABLE Management Modalities for Keratoconus An overview of noninterventional and interventional treatments. BY MAZEN M. SINJAB, MD, PHD anagement of keratoconus has advanced TAKE-HOME MESSAGE during the past few years, and surgeons can • When evaluating patients with keratoconus, ask now choose among numerous traditional and them to stop using RGP contact lenses at least 2 modern treatments. Traditional modalities weeks before evaluation to achieve correct Msuch as spectacle correction, contact lenses, penetrating measurement of the corneal shape. keratoplasty (PKP), and conductive keratoplasty (CK) • Interventional management modalities include CK, are still effective; however, demand for the last two has PKP, DALK, ICRSs, CXL, phakic IOLs, or some decreased with the advent of modern alternatives, specifi- combination of these treatments. cally intrastromal corneal ring segments (ICRSs) and cor- • Making the right management decision depends neal collagen crosslinking (CXL). Caution should be used on the patient’s corneal transparency and stress when considering these newer treatment modalities, and lines, age, progression, contact lens tolerance, surgeons should be aware of their indications, contraindi- refractive error, UCVA and BCVA, K-max, corneal cations, conditions, and complications before proceeding thickness, and sex. with treatment. Keratoconus treatments can be divided into two cate- Some patients achieve good vision correction and comfort gories, interventional and noninterventional. In this article, with this strategy. particular attention is given to ICRSs and CXL, as they are Advances in lens designs and materials have increased the the most popular emerging interventional management proportion of keratoconus patients who can be fitted with modalities for keratoconus. -
Corneal Ulcers in Cats
Corneal Ulcers in Cats 803-808-7387 www.gracepets.com The cornea is the clear, shiny membrane that makes up the surface of the eyeball. It is much like a clear window. To understand a corneal ulcer, you must first understand how the cornea is constructed. The cornea is comprised of three layers. The most superficial or outermost layer is the epithelium. This layer is comprised of many, very thin layers of cells, similar to an onion’s skin. Below the epithelium is the stroma and the deepest layer is Descemet's membrane. Because all of these layers are clear, it is not possible to see them without special stains and a microscope. Erosion through a few layers of the epithelium is called a corneal erosion or corneal abrasion. A corneal ulcer is an erosion through the entire epithelium and down into the stroma. If the erosion goes through the epithelium and stroma to the level of Descemet's membrane, a descemetocele exists. If Descemet's membrane ruptures, the liquid inside the eyeball leaks out and the eye collapses. What causes corneal ulcers? There are several causes for corneal ulcers in cats. The most common is trauma. An ulcer may result from blunt trauma, such as a cat rubbing its eye on a carpet, or due to a laceration, such as a cat-claw scratch. The second most common cause is chemical burn of the cornea. This may happen when irritating shampoo or dip gets in the eye. Less common causes of corneal ulcers include bacterial infections, viral infections, and other diseases. -

Scleral Lenses and Eye Health
Scleral Lenses and Eye Health Anatomy and Function of the Human Eye How Scleral Lenses Interact with the Ocular Surface Just as the skin protects the human body, the ocular surface protects the human Scleral lenses are large-diameter lenses designed to vault the cornea and rest on the conjunctival tissue sitting on eye. The ocular surface is made up of the cornea, the conjunctiva, the tear film, top of the sclera. The space between the back surface of the lens and the cornea acts as a fluid reservoir. Scleral and the glands that produce tears, oils, and mucus in the tear film. lenses can range in size from 13mm to 19mm, although larger diameter lenses may be designed for patients with more severe eye conditions. Due to their size, scleral lenses consist SCLERA: The sclera is the white outer wall of the eye. It is SCLERAL LENS made of collagen fibers that are arranged for strength rather of at least two zones: than transmission of light. OPTIC ZONE The optic zone vaults over the cornea CORNEA: The cornea is the front center portion of the outer Cross section of FLUID RESERVOIR wall of the eye. It is made of collagen fibers that are arranged in the eye shows The haptic zone rests on the conjunctiva such a way so that the cornea is clear. The cornea bends light the cornea, overlying the sclera as it enters the eye so that the light is focused on the retina. conjunctiva, and sclera as CORNEA The cornea has a protective surface layer called the epithelium. -

Association Between Visual Field Damage and Corneal Structural
www.nature.com/scientificreports OPEN Association between visual feld damage and corneal structural parameters Alexandru Lavric1*, Valentin Popa1, Hidenori Takahashi2, Rossen M. Hazarbassanov3 & Siamak Yousef4,5 The main goal of this study is to identify the association between corneal shape, elevation, and thickness parameters and visual feld damage using machine learning. A total of 676 eyes from 568 patients from the Jichi Medical University in Japan were included in this study. Corneal topography, pachymetry, and elevation images were obtained using anterior segment optical coherence tomography (OCT) and visual feld tests were collected using standard automated perimetry with 24-2 Swedish Interactive Threshold Algorithm. The association between corneal structural parameters and visual feld damage was investigated using machine learning and evaluated through tenfold cross-validation of the area under the receiver operating characteristic curves (AUC). The average mean deviation was − 8.0 dB and the average central corneal thickness (CCT) was 513.1 µm. Using ensemble machine learning bagged trees classifers, we detected visual feld abnormality from corneal parameters with an AUC of 0.83. Using a tree-based machine learning classifer, we detected four visual feld severity levels from corneal parameters with an AUC of 0.74. Although CCT and corneal hysteresis have long been accepted as predictors of glaucoma development and future visual feld loss, corneal shape and elevation parameters may also predict glaucoma-induced visual functional loss. While intraocular pressure (IOP), age, disc hemorrhage, and optic cup characteristics have been long identifed as classic risk factors for development of primary open-angle glaucoma (POAG)1,2, the Ocular Hypertension Treatment Study (OHTS) suggested central corneal thickness (CCT) as a new risk factor for development of POAG3. -

Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation
10.5005/jp-journals-10025-1024 JaimeCASE Levy REPORT et al Treatment of Stable Keratoconus by Cataract Surgery with Toric IOL Implantation Jaime Levy, Anry Pitchkhadze, Tova Lifshitz ABSTRACT implantation in the right eye. On presentation, uncorrected We present the case of a 73-year-old patient who underwent visual acuity (UCVA) was 6/60 OU. Refraction was –0.75 successful phacoemulsification and toric intraocular lens (IOL) –5.0 × 65° OD and –3.25 –4.0 × 98° OS. Nuclear sclerosis implantation to correct high stable astigmatism due to and posterior subcapsular cataract +2 was observed in the keratoconus and cataract. Preoperative refraction was –3.25 – left eye. The posterior segments were unremarkable. 4.0 × 98°. A toric IOL (Acrysof SN60T6) with a spherical power of 16.5 D and a cylinder power of 3.75 D at the IOL plane and Corneal topography performed with Orbscan (Bausch 2.57 D at the corneal plane was implanted and aligned at an and Lomb, Rochester, NY) showed central thinning of 457 axis of 0°. Uncorrected visual acuity improved from 6/60 to microns and positive islands of elevation typical for 6/10. Postoperative best corrected visual acuity was 6/6, 6 months after the operation. In conclusion, phacoemulsification keratoconus in the right eye (Fig. 1). In the left eye a less with toric IOL implantation can be performed in eyes with pronounced inferior cone was observed (Fig. 2), without keratoconus and cataract. any area of significant thinning near the limbus typical for Keywords: Intraocular lens, Toric IOL, Keratoconus, Cataract pellucid marginal degeneration.2 Keratometry (K)-values surgery. -

Distribution of Anterior and Posterior Corneal Astigmatism in Eyes with Keratoconus
Distribution of Anterior and Posterior Corneal Astigmatism in Eyes With Keratoconus MOHAMMAD NADERAN, MOHAMMAD TAHER RAJABI, AND PARVIZ ZARRINBAKHSH PURPOSE: To investigate the magnitude, with-the-rule ERATOCONUS (KC) IS A PROGRESSIVE, USUALLY (WTR) or against-the-rule (ATR) orientation, and vec- bilateral ectatic corneal disorder, characterized by 1,2 tor components (Jackson astigmatic vectors [J0 and J45] K corneal thinning and protrusion. KC starts at and blurring strength) of the anterior and posterior puberty and progresses to the third or fourth decade of corneal astigmatism (ACA and PCA) in patients with life, causing myopia and astigmatism, which results in keratoconus (KC) in a retrospective study, and to try to severe vision distortion and sometimes even blindness.1 find suitable cutoff points for ACA and PCA in an Astigmatism is a refractive error that is mostly caused by attempt to discriminate KC from normal corneas. toricity of the anterior corneal surface leading to visually DESIGN: Retrospective age- and sex-matched case- significant optical aberration. Both the anterior and poste- control study. rior corneal surfaces contribute to the total corneal METHODS: Using the Pentacam images, the aforemen- astigmatism. Recently, the direct and quantitative mea- tioned parameters were compared between 1273 patients surement of the posterior corneal measurements in a with KC and 1035 normal participants. clinical setting has been possible with new imaging tech- RESULTS: The mean magnitude of the ACA and PCA nologies such as slit-scanning, Scheimpflug, or optical was 4.49 ± 2.16 diopter (D) and 0.90 ± 0.43 D, respec- coherence devices.3,4 tively. The dominant astigmatism orientation of the Assessment of the corneal astigmatism plays an impor- ACA was ATR in KC patients and WTR in normal par- tant role in vision correction procedures such as rigid gas- ticipants (P < .001), while for the PCA it was WTR in permeable lens prescription or intraocular lens (IOL) im- KC patients and ATR in normal participants (P < .001). -

Corneal Cross-Linking in Infectious Keratitis David Tabibian1,5*, Cosimo Mazzotta2 and Farhad Hafezi1,3,4
Tabibian et al. Eye and Vision (2016) 3:11 DOI 10.1186/s40662-016-0042-x REVIEW Open Access PACK-CXL: Corneal cross-linking in infectious keratitis David Tabibian1,5*, Cosimo Mazzotta2 and Farhad Hafezi1,3,4 Abstract Background: Corneal cross-linking (CXL) using ultraviolet light-A (UV-A) and riboflavin is a technique developed in the 1990’s to treat corneal ectatic disorders such as keratoconus. It soon became the new gold standard in multiple countries around the world to halt the progression of this disorder, with good long-term outcomes in keratometry reading and visual acuity. The original Dresden treatment protocol was also later on used to stabilize iatrogenic corneal ectasia appearing after laser-assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). CXL efficiently strengthened the cornea but was also shown to kill most of the keratocytes within the corneal stroma, later on repopulated by those cells. Review: Ultraviolet-light has long been known for its microbicidal effect, and thus CXL postulated to be able to sterilize the cornea from infectious pathogens. This cytotoxic effect led to the first clinical trials using CXL to treat advanced infectious melting corneal keratitis. Patients treated with this technique showed, in the majority of cases, a stabilization of the melting process and were able to avoid emergent à chaud keratoplasty. Following those primary favorable results, CXL was used to treat beginning bacterial keratitis as a first-line treatment without any adjunctive antibiotics with positive results for most patients. In order to distinguish the use of CXL for infectious keratitis treatment from its use for corneal ectatic disorders, a new term was proposed at the 9th CXL congress in Dublin to rename its use in infections as photoactivated chromophore for infectious keratitis -corneal collagen cross-linking (PACK-CXL). -

Ocular Emergencies for the Primary Care Optometrist
Ocular Emergencies Ocular Emergencies for the Disclosure Statement Primary Care Optometrist . Honorarium, Speaker, Consultant, Research Grant: Aerie, Alcon, Allergan, B+L, Carl Zeiss, Glaukos, Heidelberg, Novartis, Topcon, Michael Chaglasian, OD, FAAO Associate Professor Illinois Eye Institute Illinois College of Optometry [email protected] What is a “True” Emergency? “True” Emergency . Pain (vs. discomfort) . History is key to differentiating emergency versus urgency . Current or potential for: Phone or in person Vision loss Proper triage is essential Structural damage After hours protocol Needs immediate (same day) attention Your office and your specialists Medico-legal implications History Emergency Exam Vision Recent ocular disease or One or both eyes? surgery . Acuity . External examination Visual field Other diseases . Visual fields . SLE Sudden or gradual cardiac, vascular, or . Pupils Blurred or lost? autoimmune . IOP Diplopia? viruses . Ocular Motility . Fundus exam Mono or Bino Medications or recent Pain changes to medications Redness Nausea/vomiting Onset Trauma Contact lenses M. Chaglasian, OD 1 Ocular Emergencies Emergency Kit “True” Emergency . Chemical Burns . Eye shield . pH paper Alkaline . Pressure patch . Bandage CL’s . Sterile eye wash . Diamox . Central Retinal Artery Occlusion . Alger brush . Topical drops . Forceps Antibiotics NSAID’s . Golf spud . Both have extremely high risk of severe and permanent Steroids vision loss which can be prevented via immediate Cycloplegics intervention and treatment Chemical Trauma Chemical Burns . Copious irrigation anesthetic . Acid exposure speculum Only penetrate through epithelium sterile saline v tap water car battery, vinegar, and some refrigerants . Contacts can be removed after irrigation . Sweep fornices – repeatedly . Alkaline exposure Penetrates tissues more easily and . Examination after irrigation and neutralization of pH have a prolonged effect .