Mooren's Ulcer: Diagnosis and Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Differentiate Red Eye Disorders
Introduction DIFFERENTIATE RED EYE DISORDERS • Needs immediate treatment • Needs treatment within a few days • Does not require treatment Introduction SUBJECTIVE EYE COMPLAINTS • Decreased vision • Pain • Redness Characterize the complaint through history and exam. Introduction TYPES OF RED EYE DISORDERS • Mechanical trauma • Chemical trauma • Inflammation/infection Introduction ETIOLOGIES OF RED EYE 1. Chemical injury 2. Angle-closure glaucoma 3. Ocular foreign body 4. Corneal abrasion 5. Uveitis 6. Conjunctivitis 7. Ocular surface disease 8. Subconjunctival hemorrhage Evaluation RED EYE: POSSIBLE CAUSES • Trauma • Chemicals • Infection • Allergy • Systemic conditions Evaluation RED EYE: CAUSE AND EFFECT Symptom Cause Itching Allergy Burning Lid disorders, dry eye Foreign body sensation Foreign body, corneal abrasion Localized lid tenderness Hordeolum, chalazion Evaluation RED EYE: CAUSE AND EFFECT (Continued) Symptom Cause Deep, intense pain Corneal abrasions, scleritis, iritis, acute glaucoma, sinusitis, etc. Photophobia Corneal abrasions, iritis, acute glaucoma Halo vision Corneal edema (acute glaucoma, uveitis) Evaluation Equipment needed to evaluate red eye Evaluation Refer red eye with vision loss to ophthalmologist for evaluation Evaluation RED EYE DISORDERS: AN ANATOMIC APPROACH • Face • Adnexa – Orbital area – Lids – Ocular movements • Globe – Conjunctiva, sclera – Anterior chamber (using slit lamp if possible) – Intraocular pressure Disorders of the Ocular Adnexa Disorders of the Ocular Adnexa Hordeolum Disorders of the Ocular -

Neurotrophic Keratopathy and Diabetes Mellitus a Lockwood Et Al 838
Eye (2006) 20, 837–839 & 2006 Nature Publishing Group All rights reserved 0950-222X/06 $30.00 www.nature.com/eye 1 1 2 Neurotrophic A Lockwood , M Hope-Ross and P Chell CASE SERIES keratopathy and diabetes mellitus Abstract no history of previous corneal trauma or herpes simplex infection. Ocular examination revealed Diabetes mellitus is frequently associated a best-corrected visual acuity of 6/12 in both with microvascular complications such as eyes. There was an epithelial irregularity retinopathy, nephropathy, and peripheral extending across the inferonasal quadrant of the neuropathy. Neurotrophic keratopathy occurs right cornea. A diagnosis of exposure in response to a neuropathy of the ophthalmic keratopathy was made. She was treated with division of the trigeminal nerve. Rarely has artificial tears and a month later the epithelium diabetic neurotrophic keratopathy been had healed. A year later, an epithelial defect in described. This paper discusses the the same area was seen at follow-up. Again she ophthalmic histories of three patients who was asymptomatic and the visual acuity was presented with diabetic neurotrophic unchanged. Decreased corneal sensation was keratopathy. In one patient the corneal noted using a cotton swab to touch the ulceration was the sole presenting feature of peripheral and central cornea. A diagnosis of his diabetes. We discuss the need for increased diabetic neurotrophic keratopathy was made. vigilance in the ophthalmic community for She was treated with ocular lubricants. After suspecting diabetes in patients with 6 months, the defect had increased in size to unexplained corneal epithelial disease. 5.5 mm. There was associated corneal Eye (2006) 20, 837–839. -
Corneal Ulcers in Cats
Corneal Ulcers in Cats 803-808-7387 www.gracepets.com The cornea is the clear, shiny membrane that makes up the surface of the eyeball. It is much like a clear window. To understand a corneal ulcer, you must first understand how the cornea is constructed. The cornea is comprised of three layers. The most superficial or outermost layer is the epithelium. This layer is comprised of many, very thin layers of cells, similar to an onion’s skin. Below the epithelium is the stroma and the deepest layer is Descemet's membrane. Because all of these layers are clear, it is not possible to see them without special stains and a microscope. Erosion through a few layers of the epithelium is called a corneal erosion or corneal abrasion. A corneal ulcer is an erosion through the entire epithelium and down into the stroma. If the erosion goes through the epithelium and stroma to the level of Descemet's membrane, a descemetocele exists. If Descemet's membrane ruptures, the liquid inside the eyeball leaks out and the eye collapses. What causes corneal ulcers? There are several causes for corneal ulcers in cats. The most common is trauma. An ulcer may result from blunt trauma, such as a cat rubbing its eye on a carpet, or due to a laceration, such as a cat-claw scratch. The second most common cause is chemical burn of the cornea. This may happen when irritating shampoo or dip gets in the eye. Less common causes of corneal ulcers include bacterial infections, viral infections, and other diseases. -

Corneal Cross-Linking in Infectious Keratitis David Tabibian1,5*, Cosimo Mazzotta2 and Farhad Hafezi1,3,4
Tabibian et al. Eye and Vision (2016) 3:11 DOI 10.1186/s40662-016-0042-x REVIEW Open Access PACK-CXL: Corneal cross-linking in infectious keratitis David Tabibian1,5*, Cosimo Mazzotta2 and Farhad Hafezi1,3,4 Abstract Background: Corneal cross-linking (CXL) using ultraviolet light-A (UV-A) and riboflavin is a technique developed in the 1990’s to treat corneal ectatic disorders such as keratoconus. It soon became the new gold standard in multiple countries around the world to halt the progression of this disorder, with good long-term outcomes in keratometry reading and visual acuity. The original Dresden treatment protocol was also later on used to stabilize iatrogenic corneal ectasia appearing after laser-assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). CXL efficiently strengthened the cornea but was also shown to kill most of the keratocytes within the corneal stroma, later on repopulated by those cells. Review: Ultraviolet-light has long been known for its microbicidal effect, and thus CXL postulated to be able to sterilize the cornea from infectious pathogens. This cytotoxic effect led to the first clinical trials using CXL to treat advanced infectious melting corneal keratitis. Patients treated with this technique showed, in the majority of cases, a stabilization of the melting process and were able to avoid emergent à chaud keratoplasty. Following those primary favorable results, CXL was used to treat beginning bacterial keratitis as a first-line treatment without any adjunctive antibiotics with positive results for most patients. In order to distinguish the use of CXL for infectious keratitis treatment from its use for corneal ectatic disorders, a new term was proposed at the 9th CXL congress in Dublin to rename its use in infections as photoactivated chromophore for infectious keratitis -corneal collagen cross-linking (PACK-CXL). -

Ocular Emergencies for the Primary Care Optometrist
Ocular Emergencies Ocular Emergencies for the Disclosure Statement Primary Care Optometrist . Honorarium, Speaker, Consultant, Research Grant: Aerie, Alcon, Allergan, B+L, Carl Zeiss, Glaukos, Heidelberg, Novartis, Topcon, Michael Chaglasian, OD, FAAO Associate Professor Illinois Eye Institute Illinois College of Optometry [email protected] What is a “True” Emergency? “True” Emergency . Pain (vs. discomfort) . History is key to differentiating emergency versus urgency . Current or potential for: Phone or in person Vision loss Proper triage is essential Structural damage After hours protocol Needs immediate (same day) attention Your office and your specialists Medico-legal implications History Emergency Exam Vision Recent ocular disease or One or both eyes? surgery . Acuity . External examination Visual field Other diseases . Visual fields . SLE Sudden or gradual cardiac, vascular, or . Pupils Blurred or lost? autoimmune . IOP Diplopia? viruses . Ocular Motility . Fundus exam Mono or Bino Medications or recent Pain changes to medications Redness Nausea/vomiting Onset Trauma Contact lenses M. Chaglasian, OD 1 Ocular Emergencies Emergency Kit “True” Emergency . Chemical Burns . Eye shield . pH paper Alkaline . Pressure patch . Bandage CL’s . Sterile eye wash . Diamox . Central Retinal Artery Occlusion . Alger brush . Topical drops . Forceps Antibiotics NSAID’s . Golf spud . Both have extremely high risk of severe and permanent Steroids vision loss which can be prevented via immediate Cycloplegics intervention and treatment Chemical Trauma Chemical Burns . Copious irrigation anesthetic . Acid exposure speculum Only penetrate through epithelium sterile saline v tap water car battery, vinegar, and some refrigerants . Contacts can be removed after irrigation . Sweep fornices – repeatedly . Alkaline exposure Penetrates tissues more easily and . Examination after irrigation and neutralization of pH have a prolonged effect . -

Management of Corneal Perforation Vishal Jhanji, MD,1,2,3 Alvin L
SURVEY OF OPHTHALMOLOGY VOLUME 56 NUMBER 6 NOVEMBER–DECEMBER 2011 MAJOR REVIEW Management of Corneal Perforation Vishal Jhanji, MD,1,2,3 Alvin L. Young, MMedSc (Hons), FRCSI,3 Jod S. Mehta, MD,4 Namrata Sharma, MD,5 Tushar Agarwal, MD,5 and Rasik B. Vajpayee, MS, FRCS (Edin), FRANZCO1,5,6 1Centre for Eye Research Australia, University of Melbourne, Australia; 2Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Hong Kong; 3Department of Ophthalmology and Visual Sciences, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong; 4Singapore National Eye Centre, Singapore; 5Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi, India; and 6Royal Victorian Eye and Ear Hospital, Melbourne, Australia Abstract. Corneal perforation may be associated with prolapse of ocular tissue and requires prompt diagnosis and treatment. Although infectious keratitis is an important cause, corneal xerosis and collagen vascular diseases should be considered in the differential diagnosis, especially in cases that do not respond to conventional medical therapy. Although medical therapy is a useful adjunct, a surgical approach is required for most corneal perforations. Depending on the size and location of the corneal perforation, treatment options include gluing, amniotic membrane transplantation, and corneal transplantation. (Surv Ophthalmol 56:522--538, 2011. Ó 2011 Elsevier Inc. All rights reserved.) Key words. corneal perforation diagnosis keratoplasty management patch graft therapeutic keratoplasty I. Introduction The selection of an appropriate treatment option is Corneal perforation is a cause of ocular morbidity mostly guided by size and location of the perfora- and profound visual loss.13,119 It is the end result of tion and the status of the underlying disease. -

Is Myopia Related to Intraocular Pressure
Br J Ophthalmol: first published as 10.1136/bjo.88.1.1-a on 23 December 2003. Downloaded from Creig Hoyt Editor IS MYOPIA RELATED TO empirical treatment of corneal ulcers—for example, aminoglycosides, cephalospor- ins, and fluoroquinones. Emergence of resistant strains is a major concern when INTRAOCULAR PRESSURE? antibiotics such as fluoroquinones are used as monotherapy. Bosscha and coworkers The precise aetiological factors respon- report the results of a retrospective study of 91 patients with bacterial ulcers treated sible for the development of myopia are with a topical combination of polymyxin B, neomycin, and gramicidin. In this study incompletely understood. Intraocular this combination was effective in the safe treatment of suspected corneal ulceration. pressure is one of several factors impli- Among 91 patients there were four perforations and one evisceration. cated in the pathogenesis of myopia. It See p 25 has been postulated that elevated intraocular pressure would create RISK FACTORS FOR ACUTE ENDOPHTHALMITIS scleral stress resulting in axial elonga- Acute infectious endophthalmitis remains a vision threatening complication of tion. Lee and coworkers report a study cataract. Although rare, it is a serious and dreaded complication. Wong and Chee of 636 Chinese children age 9–11 years report a retrospective case controlled study of 34 patients with acute endophthalmi- who underwent non-contact tonome- tis presenting within 6 weeks after cataract surgery. Three controls per case were try, cycloplegic autorefraction, and A- randomly selected from cataract surgery lists matched on the date of operation of scan biometry. There were no signifi- cases. This study suggests that the use of silicone intraocular lenses and/or rupture of cant intraocular pressure differences posterior capsule are risk factors for the development of acute endophthalmitis after between low or high myopes and cataract surgery. -

Treatment of Peripheral Corneal Ulcers by Limbal Conjunctivectomy
Brit. 7. Ophthal. (I 976) 6o, 713 Br J Ophthalmol: first published as 10.1136/bjo.60.10.713 on 1 October 1976. Downloaded from Treatment of peripheral corneal ulcers by limbal conjunctivectomy FRED M. WILSON II, MERRILL GRAYSON, AND FORREST D. ELLIS From the Department of Ophthalmology, Indiana University School of Medicine, Indianapolis, Indiana Peripheral corneal ulcers can still pose difficult appear within the ulcer about one week later, followed clinical problems despite therapeutic advances such in a few days by superficial vascularization. The ulcer as specific antimicrobial agents, collagenase inhibi- had healed and epithelialized three weeks after surgery tors, heparin, ocular lubricants, biological adhe- (Fig. ib) and L-cysteine and heparin drops were con- sives, and soft contact lenses. This paper reports tinued for three weeks after it had healed. The ulcer has the healing of several types of progressive marginal ulcers after the excision and recession of adjacent limbal conjunctiva (limbal conjunctivectomy), in some cases after other modes of treatment had been unsuccessful. copyright. Case reports CASE I, MOOREN )S ULCER A 54-year-old Black woman developed a severely painful, largely non-infiltrative ulcer of the nasal left cornea. The ulcer had an overhanging central edge and progressed circumferentially during a period of one year to involve nearly the entire comeal periphery http://bjo.bmj.com/ (Fig. ia). Progression occurred despite treatment at various times with acetylcysteine drops, L-cysteine drops, topical and subconjunctival heparin, artificial soft contact a short trial of tears, lens, topical cortico- (Ia.) steroids, and a trial without any treatment to minimize the possibility of overtreatment. -

Corneal Ulcer-Infiltrate Associated with Soft Contact Lens Use Following Penetrating Keratoplasty*
Cornea 3: 131-134,'1984 Corneal Ulcer-Infiltrate Associated with Soft Contact Lens Use following Penetrating Keratoplasty* S. Gregor) Smith, M.D. Richard L. Lindstrom, M.D. J. Daniel Nelson, M.D. Jack L. G7eiss, M.D. ' Donald J. Doughman, M.D. ABSTRACT INTRODUCTION A review of 100 patients who underwent penetrating keratoplasty revealed 47 who required therapeutic soft oft contact lenses have been used following contact lenses in the early postoperative period. Twelve penetrating keratoplasty for comfort, visual corneal ulcer-infiltrates, 11 of which were culture posi- S tive, occurred during soft contact lens wear (23% inci- acuity, the treatment and prevention of persistent dence of this complication in contact lens fitted eyes). epithelial defects, and to promote epithelialization I.. The most common offending organism was coagulase- of the graft. This has been reported to be relatively negative staphylococcus. The only statistically sig- safe, with few complications noted. It was our nificant risk factor for infection if a lens was used was clinical impression that our rate of complications the presence of a persistent epithelial defect (p = 0.03). was significant. For this reason a retrospective Factors which could not be statistically correlated with corneal ulcer-infiltrate included keratoconjunctivitis study was -undertaken to evaluate the incidence of sicca, the type of contact lens, the method of donor complications associated with therapeutic soft lens cornea preservation, lens hygiene, antibiotic and use following keratoplasty. steroid usage, the presence of blepharitis, preoperative bacterial keratitis, and the history of a previously failed penetrating keratoplasty. MATERIALS AND METHODS M7e performed a retrospective analysis of the records of 102 consecutive unselected patients who underwent penetrating keratoplasty at the Univer- sity of Minnesota from Februaq 1980 through April 1981. -

Case Report Comment
5. Dresner S, Codere F, Browstein S, Jouve P. Lacrimal drainage system inflammatory masses from retained silicone tubing. Am J Ophthalmol 1984;98:609. 6. McCormick SA, Lindberg JV. Pathology of nasolacrimal duct obstruction. In: Lindberg JV, editor. Lacrimal surgery. London: Churchill Livingstone, 1988:169. 7. Welham RAN, Henderson PH. Results of dacryocystorhinostomy: analysis of causes for failure. Trans Ophthalmol Soc UK 1973;93:601-9. 8. Allen KM, Berlin AI, Levine HL. Intranasal endoscopic analysis of dacryocystorhinostomy failure. Ophthalmic Plast Reconstr Surg 1988;4:143. 9. Welham RAN, Wule AE. Management of unsuccessful lacrimal surgery. Br J Ophthalmol 1987;4:152-7. 10. Walland MI, Rose GE. Factors affecting the success rate of open lacrimal surgery. Br J Ophthalmol 1994;78:888. Fig. 1. Clinical appearance of the left cornea on presentation, showing 11. Orcutt Je Hillel A, Weymuller EA Jr. Endoscopic repair of stromal infiltrate. failed dacryocystorhinostomy. Ophthalmic Plast Reconstr Surg 1990;6:197-202. fibrinous exudate. A left corneal ulcer measuring 3.5 mm L. Chang 4.0 mm was present, with stromal infiltrates temporally Wound Healing Research Unit in a semicircular configuration (Fig. 1). Corneal sensation Department of Pathology and Glaucoma Institute of Ophthalmology was present, and there was a marked degree of cells and London EC1V 9EL, UK flare but no hypopyon. Corneal scrapings were immediately obtained for culture and Gram stain, the N. Trendell-Smith Charing Cross Department of Histopathology latter showing scanty pus cells and Gram-negative rods. The Hammersmith Hospitals NHS Trust The patient was admitted and treated with topical London W6 8RF, UK cefuroxime 5% and gentamicin forte 1.5% half-hourly, J.M. -

Ocular Emergencies Brady Beale, VMD, DACVO (Ophthalmology) University of Pennsylvania School of Veterinary Medicine
Ocular Emergencies Brady Beale, VMD, DACVO (Ophthalmology) University of Pennsylvania School of Veterinary Medicine From acute loss of vision to sudden pain, redness, and clouding of the eye, patients present to the emergency room for a variety of underlying causes. Uncovering the diagnosis can be difficult, but a thorough history coupled with basic ophthalmic tests and equipment can facilitate reaching an accurate conclusion. Obtaining a relevant ocular history uncovers how rapidly the clinical signs appeared, whether vision differs depending on lighting conditions, and whether an owner is currently administering any medications that might alter the diagnostic test results. When possible, the exam should begin with eliciting a menace response, pupillary light reflexes (PLR), dazzle reflexes, and palpebral reflex followed by a Schirmer tear test, fluorescein stain and tonometry. Evaluation of the eye should include the lids, conjunctiva, cornea, anterior chamber and lens, using diffuse light or a slit lamp. In small animals, the fundic exam is preferably performed with an indirect light source and hand held lens. While the sudden red, cloudy, squinting eye could represent glaucoma, corneal ulcer, lens luxation or sudden keratoconjunctivitis sicca, performing the eye exam in a routine, systematic fashion will help reveal the underlying cause. GLAUCOMA Glaucoma describes an increase in intraocular pressure that leads to vision loss. The elevated pressure disturbs the axoplasmic flow in the optic nerve and damages the inner retinal layers (retinal ganglion cells and nerve fiber layers) as well as the outer retinal layers (outer nuclear layers and the rods and cones). This damage leads to loss of vision and pain with sustained high intraocular pressures. -
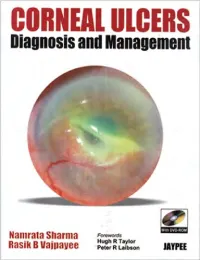
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233,