TRIM11 Locus Modifies PSP Phenotype
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Genome-Wide Analysis of 5-Hmc in the Peripheral Blood of Systemic Lupus Erythematosus Patients Using an Hmedip-Chip
INTERNATIONAL JOURNAL OF MOLECULAR MEDICINE 35: 1467-1479, 2015 Genome-wide analysis of 5-hmC in the peripheral blood of systemic lupus erythematosus patients using an hMeDIP-chip WEIGUO SUI1*, QIUPEI TAN1*, MING YANG1, QIANG YAN1, HUA LIN1, MINGLIN OU1, WEN XUE1, JIEJING CHEN1, TONGXIANG ZOU1, HUANYUN JING1, LI GUO1, CUIHUI CAO1, YUFENG SUN1, ZHENZHEN CUI1 and YONG DAI2 1Guangxi Key Laboratory of Metabolic Diseases Research, Central Laboratory of Guilin 181st Hospital, Guilin, Guangxi 541002; 2Clinical Medical Research Center, the Second Clinical Medical College of Jinan University (Shenzhen People's Hospital), Shenzhen, Guangdong 518020, P.R. China Received July 9, 2014; Accepted February 27, 2015 DOI: 10.3892/ijmm.2015.2149 Abstract. Systemic lupus erythematosus (SLE) is a chronic, Introduction potentially fatal systemic autoimmune disease characterized by the production of autoantibodies against a wide range Systemic lupus erythematosus (SLE) is a typical systemic auto- of self-antigens. To investigate the role of the 5-hmC DNA immune disease, involving diffuse connective tissues (1) and modification with regard to the onset of SLE, we compared is characterized by immune inflammation. SLE has a complex the levels 5-hmC between SLE patients and normal controls. pathogenesis (2), involving genetic, immunologic and envi- Whole blood was obtained from patients, and genomic DNA ronmental factors. Thus, it may result in damage to multiple was extracted. Using the hMeDIP-chip analysis and valida- tissues and organs, especially the kidneys (3). SLE arises from tion by quantitative RT-PCR (RT-qPCR), we identified the a combination of heritable and environmental influences. differentially hydroxymethylated regions that are associated Epigenetics, the study of changes in gene expression with SLE. -

The Emerging Relevance of AIM2 in Liver Disease
International Journal of Molecular Sciences Review The Emerging Relevance of AIM2 in Liver Disease Beatriz Lozano-Ruiz 1,2 and José M. González-Navajas 1,2,3,4,* 1 Alicante Institute for Health and Biomedical Research (ISABIAL), 03010 Alicante, Spain; [email protected] 2 Department of Pharmacology, Paediatrics and Organic Chemistry, University Miguel Hernández (UMH), 03550 San Juan, Alicante, Spain 3 Networked Biomedical Research Center for Hepatic and Digestive Diseases (CIBERehd), Institute of Health Carlos III, 28029 Madrid, Spain 4 Institute of Research, Development and Innovation in Healthcare Biotechnology in Elche (IDiBE), University Miguel Hernández, 03202 Elche, Alicante, Spain * Correspondence: [email protected]; Tel.: +34-(965)-913-928 Received: 16 August 2020; Accepted: 4 September 2020; Published: 7 September 2020 Abstract: Absent in melanoma 2 (AIM2) is a cytosolic receptor that recognizes double-stranded DNA (dsDNA) and triggers the activation of the inflammasome cascade. Activation of the inflammasome results in the maturation of inflammatory cytokines, such as interleukin (IL)-1 β and IL-18, and a form of cell death known as pyroptosis. Owing to the conserved nature of its ligand, AIM2 is important during immune recognition of multiple pathogens. Additionally, AIM2 is also capable of recognizing host DNA during cellular damage or stress, thereby contributing to sterile inflammatory diseases. Inflammation, either in response to pathogens or due to sterile cellular damage, is at the center of the most prevalent and life-threatening liver diseases. Therefore, during the last 15 years, the study of inflammasome activation in the liver has emerged as a new research area in hepatology. Here, we discuss the known functions of AIM2 in the pathogenesis of different hepatic diseases, including non-alcoholic fatty liver disease (NAFLD) and non-alcoholic steatohepatitis (NASH), hepatitis B, liver fibrosis, and hepatocellular carcinoma (HCC). -

A Computational Approach for Defining a Signature of Β-Cell Golgi Stress in Diabetes Mellitus
Page 1 of 781 Diabetes A Computational Approach for Defining a Signature of β-Cell Golgi Stress in Diabetes Mellitus Robert N. Bone1,6,7, Olufunmilola Oyebamiji2, Sayali Talware2, Sharmila Selvaraj2, Preethi Krishnan3,6, Farooq Syed1,6,7, Huanmei Wu2, Carmella Evans-Molina 1,3,4,5,6,7,8* Departments of 1Pediatrics, 3Medicine, 4Anatomy, Cell Biology & Physiology, 5Biochemistry & Molecular Biology, the 6Center for Diabetes & Metabolic Diseases, and the 7Herman B. Wells Center for Pediatric Research, Indiana University School of Medicine, Indianapolis, IN 46202; 2Department of BioHealth Informatics, Indiana University-Purdue University Indianapolis, Indianapolis, IN, 46202; 8Roudebush VA Medical Center, Indianapolis, IN 46202. *Corresponding Author(s): Carmella Evans-Molina, MD, PhD ([email protected]) Indiana University School of Medicine, 635 Barnhill Drive, MS 2031A, Indianapolis, IN 46202, Telephone: (317) 274-4145, Fax (317) 274-4107 Running Title: Golgi Stress Response in Diabetes Word Count: 4358 Number of Figures: 6 Keywords: Golgi apparatus stress, Islets, β cell, Type 1 diabetes, Type 2 diabetes 1 Diabetes Publish Ahead of Print, published online August 20, 2020 Diabetes Page 2 of 781 ABSTRACT The Golgi apparatus (GA) is an important site of insulin processing and granule maturation, but whether GA organelle dysfunction and GA stress are present in the diabetic β-cell has not been tested. We utilized an informatics-based approach to develop a transcriptional signature of β-cell GA stress using existing RNA sequencing and microarray datasets generated using human islets from donors with diabetes and islets where type 1(T1D) and type 2 diabetes (T2D) had been modeled ex vivo. To narrow our results to GA-specific genes, we applied a filter set of 1,030 genes accepted as GA associated. -

Proteomic Analysis Uncovers Measles Virus Protein C Interaction with P65
bioRxiv preprint doi: https://doi.org/10.1101/2020.05.08.084418; this version posted May 9, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder. All rights reserved. No reuse allowed without permission. Proteomic Analysis Uncovers Measles Virus Protein C Interaction with p65/iASPP/p53 Protein Complex Alice Meignié1,2*, Chantal Combredet1*, Marc Santolini 3,4, István A. Kovács4,5,6, Thibaut Douché7, Quentin Giai Gianetto 7,8, Hyeju Eun9, Mariette Matondo7, Yves Jacob10, Regis Grailhe9, Frédéric Tangy1**, and Anastassia V. Komarova1, 10** 1 Viral Genomics and Vaccination Unit, Department of Virology, Institut Pasteur, CNRS UMR-3569, 75015 Paris, France 2 Université Paris Diderot, Sorbonne Paris Cité, Paris, France 3 Center for Research and Interdisciplinarity (CRI), Université de Paris, INSERM U1284 4 Network Science Institute and Department of Physics, Northeastern University, Boston, MA 02115, USA 5 Department of Physics and Astronomy, Northwestern University, Evanston, IL 60208-3109, USA 6 Department of Network and Data Science, Central European University, Budapest, H-1051, Hungary 7 Proteomics platform, Mass Spectrometry for Biology Unit (MSBio), Institut Pasteur, CNRS USR 2000, Paris, France. 8 Bioinformatics and Biostatistics Hub, Computational Biology Department, Institut Pasteur, CNRS USR3756, Paris, France 9 Technology Development Platform, Institut Pasteur Korea, Seongnam-si, Republic of Korea 10 Laboratory of Molecular Genetics of RNA Viruses, Institut Pasteur, CNRS UMR-3569, -

For Reference Only
Datasheet Version: 1.0.0 Revision date: 05 Nov 2020 Histone H3R2me2a Antibody Catalogue No.:abx000029 Western blot analysis of extracts of various cell lines, using Asymmetric Dimethyl-Histone H3- R2 antibody (abx000029). Dot-blot analysis of various methylation peptides using Asymmetric Dimethyl-Histone H3-R2 antibody (abx000029). Immunofluorescence analysis of 293T cells using Asymmetric Dimethyl-Histone H3-R2 antibody (abx000029). Blue: DAPI for nuclear staining. Histone H3R2me2a Antibody is a Rabbit Polyclonal antibody against Histone H3R2me2a. Histones are basic nuclear proteins that are responsible for the nucleosome structure of the chromosomal fiber in eukaryotes. Nucleosomes consist of approximately 146 bp of DNA wrapped around a histone octamer composed of pairs of each of the four core histones (H2A, H2B, H3, and H4). The chromatin fiber is further compacted through the interaction of a linker histone, H1, with the DNA between the nucleosomes to form higher order chromatin structures. This gene is intronless and encodes a member of the histone H3 family. TranscriptsFor from this Reference gene lack polyA tails; instead, they contain a palindromic Only termination element. This gene is located separately from the other H3 genes that are in the histone gene cluster on chromosome 6p22-p21.3. Target: Histone H3R2me2a Clonality: Polyclonal Reactivity: Human, Mouse, Rat v1.0.0 Abbexa Ltd, Cambridge, UK · Phone: +44 1223 755950 · Fax: +44 1223 755951 1 Abbexa LLC, Houston, TX, USA · Phone: +1 832 327 7413 www.abbexa.com · Email: [email protected] Datasheet Version: 1.0.0 Revision date: 05 Nov 2020 Tested Applications: WB, IHC, IF/ICC, IP, ChIP Host: Rabbit Recommended dilutions: WB: 1/500 - 1/2000, IHC: 1/50 - 1/200, IF/ICC: 1/50 - 1/200, IP: 1/50 - 1/200, ChIP: 1/20 - 1/100, ChIPseq: 1/20 - 1/100. -
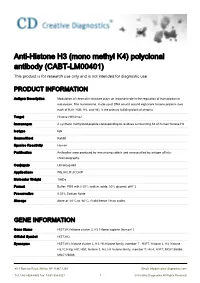
Anti-Histone H3 (Mono Methyl K4) Polyclonal Antibody (CABT-LM00401) This Product Is for Research Use Only and Is Not Intended for Diagnostic Use
Anti-Histone H3 (mono methyl K4) polyclonal antibody (CABT-LM00401) This product is for research use only and is not intended for diagnostic use. PRODUCT INFORMATION Antigen Description Modulation of chromatin structure plays an important role in the regulation of transcription in eukaryotes. The nucleosome, made up of DNA wound around eight core histone proteins (two each of H2A, H2B, H3, and H4), is the primary building block of chroma Target Histone H3K4me2 Immunogen A synthetic methylated peptide corresponding to residues surrounding K4 of human histone H3 Isotype IgG Source/Host Rabbit Species Reactivity Human Purification Antibodies were produced by immunizing rabbits and were purified by antigen affinity- chromatography. Conjugate Unconjugated Applications WB,IHC,IF,IP,ChIP Molecular Weight 15kDa Format Buffer: PBS with 0.02% sodium azide, 50% glycerol, pH7.3. Preservative 0.02% Sodium Azide Storage Store at -20°C or -80°C. Avoid freeze / thaw cycles. GENE INFORMATION Gene Name HIST3H3 histone cluster 3, H3 [ Homo sapiens (human) ] Official Symbol HIST3H3 Synonyms HIST3H3; histone cluster 3, H3; H3 histone family, member T , H3FT, histone 3, H3; histone H3.1t; H3/g; H3t; H3/t; histone 3, H3; H3 histone family, member T; H3.4; H3FT; MGC126886; MGC126888; 45-1 Ramsey Road, Shirley, NY 11967, USA Email: [email protected] Tel: 1-631-624-4882 Fax: 1-631-938-8221 1 © Creative Diagnostics All Rights Reserved Entrez Gene ID 8290 Protein Refseq NP_003484 UniProt ID Q16695 Chromosome Location 1q42 Pathway Alcoholism; Cell Cycle; Cellular Senescence; Cellular responses to stress; Chromosome Maintenance; DNA Damage/Telomere Stress Induced Senescence; EGFR1 Signaling Pathway; FSH signaling pathway; Meiosis; Meiotic Recombination; Meiotic Synapsis; Packaging O Function DNA binding; protein binding; protein heterodimerization activity References 1. -

The UBE2L3 Ubiquitin Conjugating Enzyme: Interplay with Inflammasome Signalling and Bacterial Ubiquitin Ligases
The UBE2L3 ubiquitin conjugating enzyme: interplay with inflammasome signalling and bacterial ubiquitin ligases Matthew James George Eldridge 2018 Imperial College London Department of Medicine Submitted to Imperial College London for the degree of Doctor of Philosophy 1 Abstract Inflammasome-controlled immune responses such as IL-1β release and pyroptosis play key roles in antimicrobial immunity and are heavily implicated in multiple hereditary autoimmune diseases. Despite extensive knowledge of the mechanisms regulating inflammasome activation, many downstream responses remain poorly understood or uncharacterised. The cysteine protease caspase-1 is the executor of inflammasome responses, therefore identifying and characterising its substrates is vital for better understanding of inflammasome-mediated effector mechanisms. Using unbiased proteomics, the Shenoy grouped identified the ubiquitin conjugating enzyme UBE2L3 as a target of caspase-1. In this work, I have confirmed UBE2L3 as an indirect target of caspase-1 and characterised its role in inflammasomes-mediated immune responses. I show that UBE2L3 functions in the negative regulation of cellular pro-IL-1 via the ubiquitin- proteasome system. Following inflammatory stimuli, UBE2L3 assists in the ubiquitylation and degradation of newly produced pro-IL-1. However, in response to caspase-1 activation, UBE2L3 is itself targeted for degradation by the proteasome in a caspase-1-dependent manner, thereby liberating an additional pool of IL-1 which may be processed and released. UBE2L3 therefore acts a molecular rheostat, conferring caspase-1 an additional level of control over this potent cytokine, ensuring that it is efficiently secreted only in appropriate circumstances. These findings on UBE2L3 have implications for IL-1- driven pathology in hereditary fever syndromes, and autoinflammatory conditions associated with UBE2L3 polymorphisms. -

The Conserved DNMT1-Dependent Methylation Regions in Human Cells
Freeman et al. Epigenetics & Chromatin (2020) 13:17 https://doi.org/10.1186/s13072-020-00338-8 Epigenetics & Chromatin RESEARCH Open Access The conserved DNMT1-dependent methylation regions in human cells are vulnerable to neurotoxicant rotenone exposure Dana M. Freeman1 , Dan Lou1, Yanqiang Li1, Suzanne N. Martos1 and Zhibin Wang1,2,3* Abstract Background: Allele-specifc DNA methylation (ASM) describes genomic loci that maintain CpG methylation at only one inherited allele rather than having coordinated methylation across both alleles. The most prominent of these regions are germline ASMs (gASMs) that control the expression of imprinted genes in a parent of origin-dependent manner and are associated with disease. However, our recent report reveals numerous ASMs at non-imprinted genes. These non-germline ASMs are dependent on DNA methyltransferase 1 (DNMT1) and strikingly show the feature of random, switchable monoallelic methylation patterns in the mouse genome. The signifcance of these ASMs to human health has not been explored. Due to their shared allelicity with gASMs, herein, we propose that non-tradi- tional ASMs are sensitive to exposures in association with human disease. Results: We frst explore their conservancy in the human genome. Our data show that our putative non-germline ASMs were in conserved regions of the human genome and located adjacent to genes vital for neuronal develop- ment and maturation. We next tested the hypothesized vulnerability of these regions by exposing human embryonic kidney cell HEK293 with the neurotoxicant rotenone for 24 h. Indeed,14 genes adjacent to our identifed regions were diferentially expressed from RNA-sequencing. We analyzed the base-resolution methylation patterns of the predicted non-germline ASMs at two neurological genes, HCN2 and NEFM, with potential to increase the risk of neurodegenera- tion. -

Role and Regulation of the P53-Homolog P73 in the Transformation of Normal Human Fibroblasts
Role and regulation of the p53-homolog p73 in the transformation of normal human fibroblasts Dissertation zur Erlangung des naturwissenschaftlichen Doktorgrades der Bayerischen Julius-Maximilians-Universität Würzburg vorgelegt von Lars Hofmann aus Aschaffenburg Würzburg 2007 Eingereicht am Mitglieder der Promotionskommission: Vorsitzender: Prof. Dr. Dr. Martin J. Müller Gutachter: Prof. Dr. Michael P. Schön Gutachter : Prof. Dr. Georg Krohne Tag des Promotionskolloquiums: Doktorurkunde ausgehändigt am Erklärung Hiermit erkläre ich, dass ich die vorliegende Arbeit selbständig angefertigt und keine anderen als die angegebenen Hilfsmittel und Quellen verwendet habe. Diese Arbeit wurde weder in gleicher noch in ähnlicher Form in einem anderen Prüfungsverfahren vorgelegt. Ich habe früher, außer den mit dem Zulassungsgesuch urkundlichen Graden, keine weiteren akademischen Grade erworben und zu erwerben gesucht. Würzburg, Lars Hofmann Content SUMMARY ................................................................................................................ IV ZUSAMMENFASSUNG ............................................................................................. V 1. INTRODUCTION ................................................................................................. 1 1.1. Molecular basics of cancer .......................................................................................... 1 1.2. Early research on tumorigenesis ................................................................................. 3 1.3. Developing -

A Mutation in Histone H2B Represents a New Class of Oncogenic Driver
Author Manuscript Published OnlineFirst on July 23, 2019; DOI: 10.1158/2159-8290.CD-19-0393 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. A Mutation in Histone H2B Represents A New Class Of Oncogenic Driver Richard L. Bennett1, Aditya Bele1, Eliza C. Small2, Christine M. Will2, Behnam Nabet3, Jon A. Oyer2, Xiaoxiao Huang1,9, Rajarshi P. Ghosh4, Adrian T. Grzybowski5, Tao Yu6, Qiao Zhang7, Alberto Riva8, Tanmay P. Lele7, George C. Schatz9, Neil L. Kelleher9 Alexander J. Ruthenburg5, Jan Liphardt4 and Jonathan D. Licht1 * 1 Division of Hematology/Oncology, University of Florida Health Cancer Center, Gainesville, FL 2 Division of Hematology/Oncology, Northwestern University 3 Department of Cancer Biology, Dana Farber Cancer Institute and Department of Biological Chemistry and Molecular Pharmacology, Harvard Medical School 4 Department of Bioengineering, Stanford University 5 Department of Molecular Genetics and Cell Biology, The University of Chicago 6 Department of Chemistry, Tennessee Technological University 7 Department of Chemical Engineering, University of Florida 8 Bioinformatics Core, Interdisciplinary Center for Biotechnology Research, University of Florida 9 Department of Chemistry, Northwestern University, Evanston IL 60208 Running title: Histone mutations in cancer *Corresponding Author: Jonathan D. Licht, MD The University of Florida Health Cancer Center Cancer and Genetics Research Complex, Suite 145 2033 Mowry Road Gainesville, FL 32610 352-273-8143 [email protected] Disclosures: The authors have no conflicts of interest to declare Downloaded from cancerdiscovery.aacrjournals.org on September 27, 2021. © 2019 American Association for Cancer Research. Author Manuscript Published OnlineFirst on July 23, 2019; DOI: 10.1158/2159-8290.CD-19-0393 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. -

A Mutation in Histone H2B Represents a New Class of Oncogenic Driver
Published OnlineFirst July 23, 2019; DOI: 10.1158/2159-8290.CD-19-0393 RESEARCH ARTICLE A Mutation in Histone H2B Represents a New Class of Oncogenic Driver Richard L. Bennett1, Aditya Bele1, Eliza C. Small2, Christine M. Will2, Behnam Nabet3, Jon A. Oyer2, Xiaoxiao Huang1,4, Rajarshi P. Ghosh5, Adrian T. Grzybowski6, Tao Yu7, Qiao Zhang8, Alberto Riva9, Tanmay P. Lele8, George C. Schatz4, Neil L. Kelleher4, Alexander J. Ruthenburg6, Jan Liphardt5, and Jonathan D. Licht1 Downloaded from cancerdiscovery.aacrjournals.org on September 30, 2021. © 2019 American Association for Cancer Research. Published OnlineFirst July 23, 2019; DOI: 10.1158/2159-8290.CD-19-0393 ABSTRACT By examination of the cancer genomics database, we identified a new set of mutations in core histones that frequently recur in cancer patient samples and are predicted to disrupt nucleosome stability. In support of this idea, we characterized a glutamate to lysine mutation of histone H2B at amino acid 76 (H2B-E76K), found particularly in bladder and head and neck cancers, that disrupts the interaction between H2B and H4. Although H2B-E76K forms dimers with H2A, it does not form stable histone octamers with H3 and H4 in vitro, and when recon- stituted with DNA forms unstable nucleosomes with increased sensitivity to nuclease. Expression of the equivalent H2B mutant in yeast restricted growth at high temperature and led to defective nucleosome-mediated gene repression. Significantly, H2B-E76K expression in the normal mammary epithelial cell line MCF10A increased cellular proliferation, cooperated with mutant PIK3CA to pro- mote colony formation, and caused a significant drift in gene expression and fundamental changes in chromatin accessibility, particularly at gene regulatory elements. -

Cytogenetic and Molecular Characterization of the Macro- And
University of Ulm Department of Human Genetics Prof. Dr. med. Walther Vogel Cytogenetic and Molecular Characterization of the Macro- and Micro-inversions, which Distinguish the Human and the Chimpanzee Karyotypes - from Speciation to Polymorphism Thesis Applying for the Degree of Doctor of Human Biology (Dr. hum. biol.) Faculty of Medicine University of Ulm Presented by Justyna Monika Szamalek from Wrze śnia in Poland 2006 Amtierender Dekan: Prof. Dr. Klaus-Michael Debatin 1. Berichterstatter: Prof. Dr. med. Horst Hameister 2. Berichterstatter: Prof. Dr. med. Konstanze Döhner Tag der Promotion: 28.07.2006 Content Content 1. Introduction ...................................................................................................................7 1.1. Primate phylogeny........................................................................................................7 1.2. Africa as the place of human origin and the living area of the present-day chimpanzee populations .................................................................9 1.3. Cytogenetic and molecular differences between human and chimpanzee genomes.............................................................................................10 1.4. Cytogenetic and molecular differences between common chimpanzee and bonobo genomes................................................................................17 1.5. Theory of speciation .....................................................................................................18 1.6. Theory of selection