Weekly Data Report - August 11, 2021 Table of Contents Background
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2016 Recognition Targets for Hospitals
Patient Safety Reporting Program 2016 Recognition Targets for Hospitals March 2016 Recognition targets provide attainable goals for healthcare facilities participating in the Patient Safety Reporting Program (PSRP). Targets can also help facilities incrementally and effectively build adverse event review and reporting into their culture of safety. On a statewide level, targets ensure OPSC receives enough adverse event reports to build a strong database of prevention strategies so that all Oregon healthcare facilities can learn from one another. Targets are effective as of January 1, 2016. Although a participant may meet or exceed targets at any time throughout the year, the facility should continue to report adverse events according to reporting program guidelines. Healthcare facilities that meet targets are recognized annually for their transparency efforts and commitment to patient safety. For more information, visit oregonpatientsafety.org. Meet Targets Exceed Targets Quantity The number of reports submitted by a participating Submit at least the Submit at least the facility minimum quantity minimum quantity target for target for Goal: Help ensure PSRP obtains enough reports to your facility your facility build a strong database for learning. (see page 2) (see page 2) Acceptable Quality The report identifies contributing factors, root Submit at least 2 Submit 75% of causes, and system-level action plans reports that are reports with acceptable quality acceptable quality Goal: Provide enough information so that your experience can help others learn and improve. See the Guide to Quality Reporting Timeliness The amount of time that passes between discovery Submit 50% of reports of an adverse event and when a report is submitted within 45 days of to PSRP event discovery Goal: Respond immediately after an adverse event to collect full and reliable information, reduce delays, and develop strong solutions. -

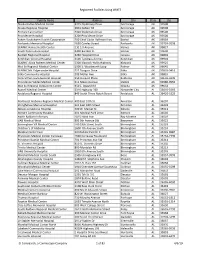
Impact of Policies on Rural Communities Oregon
Impact of Policies on Rural Communities Oregon Sequestration2 Bad Debt Reimbursement Cut3 2% Inpatient and Outpatient Medicare Revenue Cut 35% Medicare Bad Debt Reimburesment Cut Provider Operating Annual Potential Job Potential GDP Annual Potential Job Potential GDP Provider Name/Number 1 Type Margin 1 Revenue Lost 1 Loss 4 Loss 5 Revenue Lost Loss 4 Loss 5 Bay Area Hospital (380090) RPPS 5.1% $1,402,674 21 $2,694,287 $335,951 5 $645,302 Blue Mountain Hospital (381305) CAH 12.4% $103,038 2 $230,097 $22,265 0 $49,721 CHI St. Anthony Hospital (381319) CAH 14.1% $295,649 4 $570,912 $62,980 1 $121,616 Columbia Memorial Hospital (381320) CAH 13.3% $536,031 9 $1,188,408 $312,917 5 $693,753 Coquille Valley Hospital (381312) CAH -1.0% $221,858 3 $409,956 $18,291 0 $33,799 Curry General Hospital (381322) CAH -0.2% $285,231 5 $630,182 $100,353 2 $221,718 Good Shepherd Health Care System (381325) CAH 4.5% $425,575 7 $923,659 $62,123 1 $134,829 Grande Ronde Hospital (381321) CAH 3.6% $445,021 7 $879,693 $167,414 3 $330,936 Harney District Hospital (381307) CAH -1.8% $103,560 2 $240,129 $17,862 0 $41,417 Lake District Hospital (381309) CAH 0.3% $120,338 3 $338,664 $11,533 0 $32,456 Lower Umpqua Hospital District (381311) CAH -5.8% $121,920 2 $285,842 $68,875 1 $161,478 Mercy Medical Center (380027) RPPS 16.5% $1,187,722 20 $2,610,228 $101,817 2 $223,760 Mid-Columbia Medical Center (380001) RPPS 3.2% $477,045 9 $1,109,291 $139,303 3 $323,927 PeaceHealth Cottage Grove Community Medical Center CAH 19.4% $237,056 4 $483,247 $87,272 1 $177,907 (381301) 1 CMS Healthcare Cost Report Information System (HCRIS) Q1 2020. -

Beacon Name Changing to Affinity
September 30, 2016 Dear Provider, A few months ago we sent you some information and an attestation of acknowledgement that the Beacon network name will be changing to the Affinity network for the 2017 plan year. With 2017 open enrollment beginning in November, we want to make sure you are aware of changes to Moda’s Beacon Network, which is available to individuals purchasing health coverage directly from Moda or through the federal marketplace exchange. For plans effective January 1, 2017, the Beacon Network name in your area will change to the Affinity Network. The Beacon Network will continue to serve members in select Western Oregon counties. The Affinity Network will be available to individual members residing in the following counties: Baker Morrow Gilliam Sherman Grant Umatilla Harney Union Lake Wallowa Malheur Wheeler Affinity is designed to ensure members find the care they need, when they need it, Affinity helps members looking for customized care that fits their individual lifestyle and budget, and find the care they need, when they need it. With Affinity, members have access to a large selection of providers including Blue Mountain Hospital District, Good Shepherd, Grande Ronde Hospital, Harney District Hospital, Lake District Hospital, Pioneer Memorial Hospital (Heppner), St. Alphonsus Baker City, St. Alphonsus Ontario, and Wallowa Memorial Hospital. Although the Affinity name is new, we don’t expect any changes to your current workflow. Reimbursement, referrals to in-network providers, prior authorizations and processes will be the same. Individuals choosing plans supported by the Affinity network will be asked to select a primary care physician (PCP) to coordinate care. -

Umatilla &Morrow
Safe Kids Oregon 2012 State Report Dear Child Safety Advocates, Injury prevention efforts continue to make a difference to Oregon’s children. Between 2005-2007 and 2009-2011 deaths to children ages 0 – 14 from unintentional injuries decreased by 18.9% (from 148 to 120) and hospitalizations decreased by 17.3% (from 3,539 to 3,214). The important injury prevention messages and events hosted by Safe Kids Coalitions and partners throughout communities in 2012 continue to help families make safe INSIDE THIS REPORT: choices. This report details the extensive work of Safe Kids Oregon and the eight coalitions and three chapters in Introduction 1-3 Oregon. Please take a moment to read about our efforts. Prevention Activity Statewide 4-6 2012 was a year of transition for Safe Kids Oregon. I wish Motor Vehicle Occupant Safety to thank Adrienne Greene for her support as she moved Pedestrian Safety into her role as CDC Grant Manager and Tam Peterson for Bicycle and Wheeled Sports Safety her valuable training in website maintenance and Suffocation Prevention and Safe newsletter design. Additionally, the Safe Kids Oregon Sleep Advisory Board has been very active and involved in Fire and Burn Prevention providing guidance to Safe Kids Oregon. Fall Prevention Water Safety Sports Safety Ruth Harshfield Safe Kids Oregon Director Chapters & Coalitions 7 - 18 Safe Kids Oregon Safe Kids Central Oregon Safe Kids Columbia County Safe Kid Columbia Gorge Safe Kids Harney County Safe Kids Malheur County A MESSAGE FROM Safe Kids Portland Metro Safe Kids Rogue Valley KAREN GUNSON, MD ~ Safe Kids Umatilla/Morrow Counties HONORARY CHAIR Safe Kids Union County Safe Kids Washington County The work of Safe Kids Oregon continues to be important. -

157 Entities in LIVE Status EHR/PDMP
Oregon PDMP Integration initiative Implementation Report Updated 9/30/20 189 Entities In LIVE Status Total EDIE/PDMP Prescribers 741 Total EHR/PDMP Prescribers 20111 Overall Total 20852 32 Entities In LIVE Status EDIE/PDMP # Facility Parent/Host Facility Name Prescribers Type Integration Type Adventist Medical Center 26 IH Cerner Asante Ashland Community Hospital 10 IH Epic Asante Rogue Regional Medical Center 41 IH Epic Asante Three Rivers Medical Center 19 IH Epic CHI St. Anthony Hospital 19 IH Meditech Coquille Valley Hospital District 12 IH Cerner Grande Ronde Hospital 8 IH Epic KP Sunnyside Medical Center 36 IH Epic KP Westside Medical Center 36 IH Epic Lake Health District Hospital 5 IH T-System Legacy Emanuel 25 IH Epic Legacy Good Samaritan 30 IH Epic Legacy Meridian Park 18 IH Epic Legacy Mount Hood 28 IH Epic Legacy Silverton Medical Center 15 IH Epic Oregon Health and Science University 70 IH Epic Peacehealth Peace Harbor 7 IH Epic Peacehealth Riverbend (2 Locations Riverbend & University District) 22 IH Epic Peacehealth University District 22 IH Epic Providence Hood River Memorial Hospital 10 IH Epic Providence Medford Medical Center 19 IH Epic Providence Milwaukie Hospital 13 IH Epic # Facility Parent/Host Facility Name Prescribers Type Integration Type Providence Newberg Hospital 26 IH Epic Providence Portland Medical Center 43 IH Epic Providence Seaside Hospital 7 IH Epic Providence St Vincent Medical Center 47 IH Epic Providence Willamette Falls Medical Center 12 IH Epic Salem Hospital 42 IH Epic Sky Lakes Medical Center -

Hospital Presumptive Medical -- Authorized Sites 1-Nov-14
Hospital Presumptive Medical -- Authorized Sites 1-Nov-14 Hospital Identification Number Contact Email Phone Adventist Medical Center Portland 1801887658 Donna Krenzler [email protected] 503.251.6153 Asante Tonya Richner [email protected] 541-789-5208 Asante Ashland Community Hospital 1386644029; 136114 Asante Three Rivers Medical Center 1801891809; 022560 Asante Rogue Regional Medical Center 1770587107; 162008 Blue Mountain Hospital District 1356414395 Barb Oliver [email protected] 541-575-4153 Good Shepherd Medical Center 1295789667 Jonathan Edwards [email protected] 541-667-3438 Grande Ronde Hospital 1407446195; 067801 KARLI WRIGHT [email protected] 541-963-1555 Kaiser Permanente Northwest 1124182902 Melissa Inskeep [email protected] 503 813 4111 Lake Health District 1376698522 Brian McCarthy [email protected] 541-947-7290 Legacy System Terrie Handy [email protected] Melody Jackson [email protected] Kim Carter [email protected] Legacy Emanuel 1831112358 Legacy Good Samaritan 1780608216 Legacy Meridian Park 1184647620 Legacy Mt. Hood 1255354700 Legacy Randall Children's Hospital at Legacy Emanuel 1831112358 Legacy Salmon Creek 1700809829 Lower Umpqua Hospital 1003874819; 000054; 286986 Mark Sayler [email protected] 541-271-2171 x395 Mercy Medical Center 1477590198 John Kasberger Kasberger [email protected] Luke Martin [email protected] 303-513-2502 Laurie Jones [email protected] 541-677-2461 OHSU Hospital 1609824010 Kippi Coffey [email protected] 503-494-6664 PeaceHealth -
ROR) + Library Partnership
WLA/OLA 2019 – Charting the Unknown Together Healthcare Providers & Libraries Collaborating to Support Families How to start a Reach Out and Read (ROR) + Library Partnership Step 1: Check with your librarians, early learning staff, and Youth Services/Community Managers to see if relationships already exist. Talk internally to see what type/level of partnership might make sense. Step 2: Find out if a ROR clinic exists near you! Washington https://reachoutandreadwa.org/ - 206.524.3579 - [email protected] Oregon: http://reachoutandread.org/oregon/ - 503-830-0510 - [email protected] Find a program near you: http://www.reachoutandread.org/resource-center/find-a-program/ For large scale partnerships, identify the best person at your library to reach out to the ROR director for your state. For local, clinic-to-branch level connections, ROR staff can help with making an initial introduction. In some cases, there may be value in setting up an in-person meeting with ROR, the clinic, and the library. In others, an email introduction may be ideal. Step 3: Get to know your clinic! Set up a phone or in-person meeting. Here are some questions you might ask: I am interested in knowing more about the communities you serve at your clinic. Do you serve low income families or families from specific cultural groups? What languages are spoken as a first language by your clients? What community resources do you frequently refer families to? Do you have any questions for me about what resources are available at the library? WLA/OLA -

Oregon's Rural Landscape
Oregon’s Rural Landscape Oregon’s 32 small and rural hospitals provide essential health care services to more than one million Oregonians. These hospitals are the cornerstones within the communities they serve. For most communities, they are the largest employer, offering family-wage jobs. What is the Critical Access Hospital Program? (Medicare Reimbursement) Twenty-five of Oregon’s 32 rural hospitals are Critical Access Hospitals (CAH), which is a federal program designed to improve rural health care access and reduce hospital closures. For its Medicare patients, CAHs receive cost- based reimbursement. As the name implies, cost-based reimbursement pays hospitals to cover the maximum allowable cost assumed by the hospital. Oregon’s rural hospitals have long depended on cost-based reimbursement from Medicaid and Medicare to remain viable. Prior to the CAH program and cost-based reimbursement, several rural hospitals around the country shut their doors as a result of poor reimbursement levels. What are A & B Designations? (Medicaid Reimbursement) Oregon’s rural hospitals also have a state designation based on their size and location. Similar to Medicare for CAHs, the state designation of Type A or B provides Medicaid reimbursement up to 100% of cost. These rural designations significantly improve the bottom line for many fragile community hospitals. Many rural hospitals lack the operating margins needed to access capital funding to replace or update facilities and purchase necessary health information technology or upgrades. Along with tackling financial challenges, small and rural hospitals must sustain a highly trained work force, including medical providers. Even with strong recruitment efforts, rural hospitals have difficulty attracting and retaining skilled workers. -
November 19, 2018
Q3 2018 HOSPITAL UTILIZATION AND FINANCIAL ANALYSIS November 19, 2018 4000 Kruse Way Place • Suite 100 • Lake Oswego, OR 97035 • Tel: (503) 479-6034 • www.apprisehealthinsights.com APPRISE HEALTH INSIGHTS IS A SUBSIDIARY OF THE OREGON ASSOCIATION OF HOSPITALS AND HEALTH SYSTEMS © 2018 Apprise Health Insights Q3 2018 HOSPITAL UTILIZATION AND FINANCIAL ANALYSIS ABOUT THIS REPORT This report aims to provide a quarterly analysis of the utilization and financial data submitted by Oregon’s hospitals to the DATABANK program. DATABANK is a state-mandated monthly hospital data program administered by Apprise Health Insights in collaboration with the Office for Oregon Health Policy and Research (OHPR). Please note that all DATABANK data are self-reported by the hospital and represent a twelve-month calendar year. Accuracy is the responsibility of the reporting hospitals. Because this report’s objective is to provide a complex dive into the data, the graphs and methods may change between reports. This forces only the most compelling stories to be exhibited. The determination of which graphs and stories to focus on is evaluated by hospital finance and data experts at Apprise. Note: Kaiser Sunnyside and Kaiser Westside hospitals are excluded from this analysis due to the lack of financial data available in DATABANK. LAYOUT INFORMATION Aggregate vs Median This report uses two statistics to report statewide hospital data: median and aggregate. Aggregate numbers sum up the entire amount for all hospitals into one number, where median only takes the number from the middle of the pack. Aggregate is useful when looking at the industry as a whole, such as the percent of Medicaid charges or the total number of patients visiting Emergency Departments in the state. -
View List of Registered Health Care Facilities Using WMTS
Registered Facilities Using WMTS Facility Name Address City State Zip Alaska Native Medical Center 4315 Diplomacy Drive Anchorage AK 99508 Alaska Regional Hospital 2801 DeBarr Rd Anchorage AK 99508 Primary Care Center 4320 Diplomacy Drive Anchorage AK 99508 Providence Hospital 3200 Providence Drive Anchorage AK 99508 Yukon-Kuskokwim Health Corporation 700 Chief Eddie Hoffman Hwy Bethel AK 99559 Fairbanks Memorial Hospital 1650 Cowles Street Fairbanks AK 99701-5998 SEARHC Haines Health Center 131 1st Avenue Haines AK 99827 South Peninsula Hospital 4300 Bartlett St. Homer AK 99603 Bartlett Regional Hospital 3260 Hospital Drive Juneau AK 99801 Ketchikan General Hospital 3100 Tongrass Avenue Ketchikan AK 99901 SEARHC-Alicia Roberts Medical Center 7300 Klawock-Hollis Highway Klawock AK 99925 Mat-Su Regional Medical Center 2500 S. Woodworth Loop Palmer AK 99645 SEARHC Mt. Edgecumbe Hospital 222 Tongass Drive Sitka AK 99835-9416 Sitka Community Hospital 209 Moller Ave Sitka AK 99835 Central Peninsula General Hospital 250 Hospital Place Soldotna AK 99669-6999 Providence Valdez Medical Center 911 Meals Avenue Valdez AK 99686-0550 Mat-Su Regional Outpatient Center 950 E. Bogard Rd Wasilla AK 99654 Russell Medical Center 3316 Highway 280 Alexander City AL 35010-3369 Andalusia Regional Hospital 849 South Three Notch Street Andalusia AL 36420-5325 Northeast Alabama Regional Medical Center 400 East 10th St. Anniston AL 36207 Stringfellow Memorial Hospital 301 East 18th Street Anniston AL 36201 Athens Limestone Hospital 700 W. Market St Athens AL 35611 -

Oregon Tech – Oregon Health and Science University Medical Laboratory Science Clinical Affiliates
Oregon Tech – Oregon Health and Science University Medical Laboratory Science Clinical Affiliates Adventist Hospital, Portland, OR Adventist Hospital, Tillamook, OR Adventist Hospital, Walla Wall, WA Asante, Grants Pass, OR Bay Area Hospital, Coos Bay, OR Bonner General Hospital, Sand Point , ID Clinical Lab of Hawaii, Aeia Oahu Columbia Memorial Hospital, Astoria, OR Corvallis Clinic, Corvallis, OR Good Samaritan Medical Center, LaFayette, CO Grande Ronde Hospital, La Grande, OR Kaiser Foundation Hospitals, Portland, Oregon Kootenai Health, Coeur d’Alene, ID Legacy Health, Portland, OR Mercy Medical Health Center, Roseburg, OR Mid-Columbia Medical Center, The Dalles, OR Northern Nevada Medical Center, Sparks, NV Oregon Health & Science University, Portland, OR Peace Health Laboratories, Springfield, OR Pease Health laboratories, Vancouver, WA Providence St. Vincent’s MC, Portland, OR Providence Medford Medical Center, Medford, Oregon Providence Milwaukie Hospital, Milwaukie, Oregon Providence Regional Lab Services Core, Portland, Oregon Providence Willamette Falls MC, Oregon City, Oregon Providence Portland Medical Center, Portland, Oregon Providence Seaside Hospital, Seaside, Oregon Providence Lab at the Oregon Clinic, Portland, Oregon Renown Regional Medical Center, Reno, NV Rogue Valley Medical Center, Medford, OR Salem Clinic, Salem, OR Salem Hospital, Salem, Oregon Samaritan Health Services, Inc., Corvallis, OR Santiam Memorial Hospital, Stayton, OR Silverton Hospital, Silverton, OR Sky Lakes Medical Center, Klamath Falls, OR St. Alphonsus Regional Medical Center, Boise, ID St. Alphonsus, Baker City, OR St. Alphonsus, Ontario, OR St Charles Medical Center, Bend, OR St Charles Medical Center, Madras, OR St Mary’s Regional Medical Center, Reno, NV Three Rivers Community Hospital, Grants Pass, OR Veterans Healthcare System, Roseburg, OR Veterans Medical Center, Portland, OR Veterans Medical Center, Boise, ID Vancouver Clinic, Vancouver, WA Willamette Valley Medical Center, McMinnville, OR . -

OHA Hospital Types
Hospital Types Oregon Health Authority categorizes hospitals based on their size, distance from another hospital, and reimbursement level. The OHA Hospital Reporting Program primarily uses three type designations: DRG, Type A, and Type B. All of the 60 acute care inpatient hospitals fall into one (and only one) of these three categories. However, there are several other state and federal designations that can impact a hospital’s financial and utilization measures. The following table provides details and definitions for all such hospital categories, as well as counts for the number of each type of hospital in Oregon. These counts are not cumulative, as some hospitals may be categorized in multiple ways. The next page contains a complete list of Oregon’s 60 acute care inpatient hospitals by category. Designation Number Description DRG hospitals are typically large urban hospitals that receive standard DRG 27 Medicare Diagnostic Related Group (DRG) based reimbursement. Type A hospitals are small hospitals (with 50 or fewer beds) that are located Type A 12 more than 30 miles from another hospital. Type B hospitals are small hospitals (with 50 or fewer beds) that are located Type B 21 within 30 miles of another hospital. Type C hospitals are rural hospitals with more than 50 beds that are not a Type C 2 referral center. These hospitals are also uniformly DRG hospitals. OregonDesignations Health district hospitals are hospitals under the control of a formal health district. In most cases the controlling entity is the local county government. Being a part of a health district allows these hospitals access to additional Health District 12 funds from tax sources to contribute to operations.