Layout Maureen V2.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Transcription of Historical Ciphers and Keys: Guidelines
cl.lingfil.uu.se/decode Beáta Megyesi [email protected] February 10, 2020 Transcription of Historical Ciphers and Keys: Guidelines Content 1 Introduction 3 2 Transcription of Ciphertext 3 2.1 Metadata 3 2.2 Content 4 2.2.1 Line breaks, spaces, punctuation and diacritical marks 4 2.2.2 Catchwords 7 2.2.3 Notes in margins 8 2.3 Transcription of ciphertext, cleartext and plaintext 10 2.4 Upload of transcriptions into the DECODE database 12 3 Transcription of Keys 12 3.1 Original keys 14 3.1.1 Metadata 14 3.1.2 Transcription of codes 14 3.1.3 Upload of transcribed original keys into the DECODE database 17 3.2 Reconstructed keys 17 3.2.1 Metadata 17 3.2.2 Transcription of codes 18 3.2.3 Upload of transcribed recovered keys into the DECODE database 18 4 Transcription of Cleartexts 18 4.1 Metadata 18 4.2 Transcription of cleartext 19 4.3 Upload of cleartext transcriptions into the DECODE database 19 5. Summary 20 Acknowledgements 20 References 20 Appendix: Transcription of Special Symbols 21 Greek letters 21 Roman numerals 22 Zodiac signs 23 Alchemical signs 24 Other signs 25 2 1 Introduction The document describes guidelines for the transcription of encrypted sources and related documents, being it ciphertext, original or recovered keys, and cleartext. Usually, the first step in attacking a cipher is the conversion of the image into a machine- readable format, represented as text. There are many different ways of transcribing a manuscript. Therefore, we developed guidelines so that the transcriptions available in the DECODE database1 (Megyesi et al., 2019) have a common format. -

04132-N2740-Phonetic.Pdf
ISO/IEC JTC1/SC2/WG2/N2740 ISO/IEC JTC 1/SC 2/WG 2 PROPOSAL SUMMARY FORM TO ACCOMPANY SUBMISSIONS FOR ADDITIONS TO THE REPERTOIRE OF ISO/IEC 106461 Please fill all the sections A, B and C below. Please read Principles and Procedures Document (P & P) from http://www.dkuug.dk/JTC1/SC2/WG2/docs/principles.html for guidelines and details before filling this form. Please ensure you are using the latest Form from http://www.dkuug.dk/JTC1/SC2/WG2/docs/summaryform.html. See also http://www.dkuug.dk/JTC1/SC2/WG2/docs/roadmaps.html for latest Roadmaps. A. Administrative 1. Title: Proposal to add additional phonetic characters to the UCS 2. Requester's name: INCITS/L2, UTC, SIL International 3. Requester type (Member body/Liaison/Individual contribution): member body (L2), liaison (UTC), expert (SIL) 4. Submission date: 2004-4-19 5. Requester's reference (if applicable): L2/04-044, L2/04-045, L2/04-046, L2/04-047 6. Choose one of the following: This is a complete proposal: yes or, More information will be provided later: B. Technical – General 1. Choose one of the following: a. This proposal is for a new script (set of characters): No Proposed name of script: b. The proposal is for addition of character(s) to an existing block: Yes (partially) Name of the existing block: Eight characters are to be allocated to two existing blocks: Latin Extended-B and Phonetic Extensions. One character is to be allocated to a block approved by WG2 for addition in Amendment 1: Combining Diacritical Marks Supplement. -

LATEX Quick Reference
LATEX quick reference Mark Gates November 19, 2012 This guide is available from http://web.eecs.utk.edu/∼mgates3/ Copyright ©2007{2011 by Mark Gates. You may freely copy and modify this document under the Creative Commons Attribution-ShareAlike license. When distributing modified versions, please include your Latex file. Purpose. This document was initially made as a quick reference to all the commands that I typically use, organized so I can understand it, with examples and without clutter. It also includes many shortcuts that I have defined in my mgates.sty file. It is not intended to be exhaustive, nor overly descriptive. Most of the general LATEXcommands can be found in the Not So Short Introduction to LATEX 2" [4]; most of the math in the Short Math Guide to LATEX [2]; most of the bibliography information in the BibTeX tutorial [3] and the natbib documentation [1]. I also wrote a separate Latex fonts guide. 1 Contents 1 Commands3 1.1 Document structure................................3 1.2 Page format....................................4 1.3 Chapters and Sections..............................5 1.4 Fonts........................................6 1.5 Reserved characters................................7 1.6 Special characters.................................7 1.7 Accented characters................................8 1.8 Special spaces...................................8 1.9 Special phrases..................................8 1.10 Line and page breaks...............................9 1.11 References, citations, footnotes......................... 10 1.12 Hyperlinks..................................... 10 2 Environments 11 2.1 Text alignment.................................. 11 2.2 Boxes....................................... 11 2.3 Block quotes.................................... 12 2.4 Verse........................................ 12 2.5 Verbatim...................................... 12 2.6 Lists........................................ 13 2.7 Tables (tabular).................................. 13 2.8 Figures and Tables............................... -

Flat Cylinders EZH/DZF/DZH
Data sheet Flat cylinders EZH/DZF/DZH Technical data TOC Bookmark Materials Flat cylinders EZH/DZF/DZH Dimensions Product range overview Ordering data Flat cylinder EZH Accessories Peripherals overview Foot mounting Type codes Flange mounting Data sheet Swivel mounting Technical data Clevis foot Materials Rod eye Dimensions Rod clevis Ordering data Coupling piece Flat cylinder DZF Self-aligning rod coupler Peripherals overview Adapter Type codes Proximity switch Data sheet Mounting kit for proximity switch Technical data Connecting cable Materials Slot cover Dimensions One-way flow control valve Ordering data Accessories Foot mounting Flange mounting Swivel flange Clevis foot Rod eye Rod clevis Self-aligning rod coupler Coupling piece Adapter Flat cylinder DZH Peripherals overview Type codes Product range overview Flat cylinders EZH/DZF/DZH Product range overview Function Design Type Piston @ Stroke [mm] [mm] Single-acting EZH EZH 1.5x6.5 10 Piston rod at one end 2.5x9 10, 20 5x20 25, 50 10x40 40 Double-acting DZF DZF 12, 18, 25 10, 25, 40, 50, 80, 100, 125, 160, 200 1 ... 200 Piston rod at one end 32, 40, 50, 63 10, 25, 40, 50, 80, 100, 125, 160, 200, 250, 320 1 ... 320 DZF-...-S2 12, 18, 25 – 1 ... 200 Through piston rod 32, 40, 50, 63 – 1 ... 320 DZF-...-S20 12, 18, 25 – 1 ... 200 Through, hollow 32, 40, 50, 63 – 1 ... 320 piston rod Double-acting DZH DZH 16 25, 40, 50, 80, 100, 125, 160, 200 1 ... 200 Piston rod at one end 20 25, 40, 50, 80, 100, 125, 160, 200, 250, 320 1 .. -

Iso/Iec Jtc 1/Sc 2 N 3730 Date: 2004-05-10
SC2/WG2 N2757R ISO/IEC JTC 1/SC 2 N 3730 DATE: 2004-05-10 ISO/IEC JTC 1/SC 2 Coded Character Sets Secretariat: Japan (JISC) DOC. TYPE Summary of Voting/Table of Replies Summary of Voting on SC 2 N 3714 : Combined PDAM Registration and Consideration Ballot: ISO/IEC 10646: 2003/Amd 1, Information technology -- Universal Multiple-Octet TITLE Coded Character Set (UCS) -- AMENDMENT 1: Glagolitic, Coptic, Georgian and other characters SOURCE SC 2 Secretariat PROJECT JTC1.02.10646.00.01 PDAM Registration: Approved. PDAM Consideration: This voting summary is forwarded STATUS to WG 2. WG 2 is requested to prepare a disposition of comments report, revised text and a recommendation for further processing. ACTION ID FYI DUE DATE DISTRIBUTION P, O and L Members of ISO/IEC JTC 1/SC 2 ; ISO/IEC JTC 1 Secretariat; ISO/IEC ITTF ACCESS LEVEL Def ISSUE NO. 188 NAME 02n3730.pdf FILE SIZE (KB) 7560 PAGES 102 Secretariat ISO/IEC JTC 1/SC 2 - IPSJ/ITSCJ *(Information Processing Society of Japan/Information Technology Standards Commission of Japan) Room 308-3, Kikai-Shinko-Kaikan Bldg., 3-5-8, Shiba-Koen, Minato-ku, Tokyo 105-0011 Japan *Standard Organization Accredited by JISC Telephone: +81-3-3431-2808; Facsimile: +81-3-3431-6493; E-mail: [email protected] Summary of Voting on ISO/IEC JTC 1/SC 2 N 3714 : Combined PDAM Registration and Consideration Ballot: ISO/IEC 10646: 2003/Amd 1, Information technology -- Universal Multiple-Octet Coded Character Set (UCS) -- AMENDMENT 1: Glagolitic, Coptic, Georgian and other characters Q1 : PDAM Registration Q2 : -

The Brill Typeface User Guide & Complete List of Characters
The Brill Typeface User Guide & Complete List of Characters Version 2.06, October 31, 2014 Pim Rietbroek Preamble Few typefaces – if any – allow the user to access every Latin character, every IPA character, every diacritic, and to have these combine in a typographically satisfactory manner, in a range of styles (roman, italic, and more); even fewer add full support for Greek, both modern and ancient, with specialised characters that papyrologists and epigraphers need; not to mention coverage of the Slavic languages in the Cyrillic range. The Brill typeface aims to do just that, and to be a tool for all scholars in the humanities; for Brill’s authors and editors; for Brill’s staff and service providers; and finally, for anyone in need of this tool, as long as it is not used for any commercial gain.* There are several fonts in different styles, each of which has the same set of characters as all the others. The Unicode Standard is rigorously adhered to: there is no dependence on the Private Use Area (PUA), as it happens frequently in other fonts with regard to characters carrying rare diacritics or combinations of diacritics. Instead, all alphabetic characters can carry any diacritic or combination of diacritics, even stacked, with automatic correct positioning. This is made possible by the inclusion of all of Unicode’s combining characters and by the application of extensive OpenType Glyph Positioning programming. Credits The Brill fonts are an original design by John Hudson of Tiro Typeworks. Alice Savoie contributed to Brill bold and bold italic. The black-letter (‘Fraktur’) range of characters was made by Karsten Lücke. -

Lgrs) for the Second Level Publication Date: 5 November 2020 Prepared By: Pitinan Kooarmornpatana
Reference Label Generation Rulesets (LGRs) for the Second Level Publication Date: 5 November 2020 Prepared By: Pitinan Kooarmornpatana Public Comment Proceeding Important Information Links Open Date: 24 August 2020 Close Date: 15 October 2020 Announcement Staff Report 5 November 2020 Public Comment Proceeding View Comments Submitted Due Date: Staff Contact: Pitinan Kooarmornpatana Email: [email protected] Section I: General Overview and Next Steps To improve the transparency and consistency of the Internationalized Domain Name (IDN) table review process to facilitate the registry operations of new gTLDs, ICANN has developed additional reference IDN Tables in machine-readable format, called reference Label Generation Rulesets (LGRs) for the second level. The reference IDN tables are based on the Guidelines for Developing Reference Label Generation Rules (LGRs), which were finalized after community review. These reference LGRs will be used in reviewing IDN tables submitted by the gTLD registries, e.g. through the Registry Service Evaluation Policy (RSEP) process. Section II: Contributors At the time this report was prepared, a total of twelve (12) community submissions had been posted to the forum. The contributors, both individuals and organizations/groups, are listed below in chronological order by posting date with initials noted. To the extent that quotations are used in the foregoing narrative (Section III), such citations will reference the contributor’s initials. Organizations and Groups: Name Submitted by Initials Chinese Generation -

Times and Helvetica Fonts Under Development
ΩTimes and ΩHelvetica Fonts Under Development: Step One Yannis Haralambous, John Plaice To cite this version: Yannis Haralambous, John Plaice. ΩTimes and ΩHelvetica Fonts Under Development: Step One. Tugboat, TeX Users Group, 1996, Proceedings of the 1996 Annual Meeting, 17 (2), pp.126-146. hal- 02101600 HAL Id: hal-02101600 https://hal.archives-ouvertes.fr/hal-02101600 Submitted on 25 Apr 2019 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. ΩTimes and ΩHelvetica Fonts Under Development: Step One Yannis Haralambous Atelier Fluxus Virus, 187, rue Nationale, F-59800 Lille, France [email protected] John Plaice D´epartement d’informatique, Universit´e Laval, Ste-Foy (Qu´ebec) Canada G1K 7P4 [email protected] TheTruthIsOutThere and publishers request that their texts be typeset —ChrisCARTER, The X-Files (1993) in Times; Helvetica (especially the bold series) is often used as a titling font. Like Computer Modern, Times is a very neutral font that can be used in a Introduction wide range of documents, ranging from poetry to ΩTimes and ΩHelvetica will be public domain technical documentation.. virtual Times- and Helvetica-like fonts based upon It would surely be more fun to prepare a real PostScript fonts, which we call “Glyph Con- Bembo- or Stempel Garamond-like font for the serifs tainers”. -

Proposal for "Swedish International" Keyboard
ISO/IEC JTC 1/SC 35 N 0748 DATE: 2005-01-31 ISO/IEC JTC 1/SC 35 User Interfaces Secretariat: Association Française de Normalisation (AFNOR) TITLE: Proposal for "Swedish International" keyboard SOURCE: Karl Ivar Larsson, Swedish Expert STATUS: FYI DATE: 2005-01-31 DISTRIBUTION: P and O members of JTC1/SC35 MEDIUM: E NO. OF PAGES: 8 Secretariat ISO/IEC JTC 1/SC 35 – Nathalie Cappel-Souquet – 11 Avenue Francis de Pressensé 93571 St Denis La Plaine Cedex France Telephone: + 33 1 41 62 82 55; Facsimile: + 33 1 49 17 91 29 e-mail: [email protected] LWP Consulting R 04/0-3 Notes: 1. This document was handed out in the SC35 Stockholm meeting 2004-11-24. 2. The proposal contained in the document relates to Swedish standardization, and at present not to any SC35 activities. Contents 1 Scope ...................................................................................................................................................................3 2 Characters added ...............................................................................................................................................3 2.1 Diacritical marks.................................................................................................................................................3 2.2 Special-shape letters..........................................................................................................................................3 2.3 Other characters.................................................................................................................................................3 -
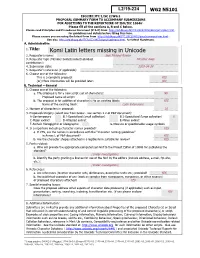
Komi Latin Letters Missing in Unicode 2
WG2 N5101 ISO/IEC JTC 1/SC 2/WG 2 PROPOSAL SUMMARY FORM TO ACCOMPANY SUBMISSIONS 1 FOR ADDITIONS TO THE REPERTOIRE OF ISO/IEC 10646TP PT Please fill all the sections A, B and C below. Please read Principles and Procedures Document (P & P) from HTU http://std.dkuug.dk/JTC1/SC2/WG2/docs/principles.html UTH for guidelines and details before filling this form. Please ensure you are using the latest Form from HTU http://std.dkuug.dk/JTC1/SC2/WG2/docs/summaryform.htmlUTH. See also HTU http://std.dkuug.dk/JTC1/SC2/WG2/docs/roadmaps.html UTH for latest Roadmaps. A. AdministratiVe 1. Title: Komi Latin letters missing in Unicode 2. Requester's name: Jack Michael Rueter 3. Requester type (Member body/Liaison/Individual Member body contribution): 4. Submission date: 2019-04-24 5. Requester's reference (if applicable): 6. Choose one of the following: This is a complete proposal: YES (or) More information will be provided later: NO B. Technical – General 1. Choose one of the following: a. This proposal is for a new script (set of characters): NO Proposed name of script: b. The proposal is for addition of character(s) to an existing block: YES Name of the existing block: Latin Extensions 2. Number of characters in proposal: 16 3. Proposed category (select one from below - see section 2.2 of P&P document): A-Contemporary B.1-Specialized (small collection) B.2-Specialized (large collection) X C-Major extinct D-Attested extinct E-Minor extinct F-Archaic Hieroglyphic or Ideographic G-Obscure or questionable usage symbols 4. -

The TLG Beta Code Manual
® The TLG Beta Code Manual Table of Contents Introduction ......................................................................................................................................................................2 Notes ............................................................................................................................................................................3 Beta Escape Codes .......................................................................................................................................................4 1. Alphabets and Basic Punctuation ................................................................................................................................5 1.1. Greek .....................................................................................................................................................................5 1.2. Combining Diacritics ............................................................................................................................................6 1.3 Basic Punctuation ..................................................................................................................................................6 1.2. Latin ......................................................................................................................................................................7 1.3. Coptic ...................................................................................................................................................................8 -

05.31.2017 Disbursements.XLSX
RECS found:4,803; RUN time: 22.81 sec Layout: /DEFAULT COLLIER COUNTY BOARD OF COUNTY COMMISSIONERS Company: = 1000 DISBURSEMENTS REPORT Clearing Date: 05/11/2017 - 05/31/2017 FOR THE PERIOD OF 05/11/2017 - 05/31/2017 Doc Type: All Vendor: All Clr Date Payee Check Amt G/L Description Public Purpose or Invoice Description 5/11/2017 CITY OF NAPLES FINANCE DEPARTMENT 132007 1,301.90 WATER AND SEWER 03/03/17-05/02/17 2375 TOWER RD 5/11/2017 CITY OF NAPLES FINANCE DEPARTMENT 132007 2,216.41 WATER AND SEWER 03/03/17-05/02/17 2885 S 3,518.31 5/11/2017 ACCU CARE NURSING SERVICE INC 132008 6,810.00 PERS/RESPITE/HOMEMAKER SERV 3/20/17-4/23/17 ADI 6,810.00 5/11/2017 VERIZON WIRELESS 132010 4,544.77 CELLULAR TELEPHONE 03/24/17-04/23/17 #342045 5/11/2017 VERIZON WIRELESS 132010 138.47 CELLULAR TELEPHONE 03/24/17-04/23/17 #342045 5/11/2017 VERIZON WIRELESS 132010 1,705.74 CELLULAR TELEPHONE 03/24/17-04/23/17 #342045 5/11/2017 VERIZON WIRELESS 132010 36.07 CELLULAR TELEPHONE 03/24/17-04/23/17 #342045 5/11/2017 VERIZON WIRELESS 132010 36.07 CELLULAR TELEPHONE 03/24/17-04/23/17 #342045 6,461.12 5/11/2017 FLORIDA DEPARTMENT OF ENVIRONMEN 132011 11,889.72 LICENSES AND PERMITS ANNUAL LEASE FEE 17/1 11,889.72 5/11/2017 COVER ALL INC 132012 53,775.00 PAINTING CONTRACTORS PAINT REC YARD NAPLES JAI 5/11/2017 COVER ALL INC 132012 1,039.68 PAINTING CONTRACTORS PAINT REC YARD NAPLES JAI 54,814.68 5/11/2017 RM ENTERPRISES OF SOUTHWEST FLOR 132013 7,370.00 OTHER CONTRACTUAL SERVICES SOD & INSTALLATION-E NAPL 5/11/2017 RM ENTERPRISES OF SOUTHWEST FLOR 132013 344.00