Proquest Dissertations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmaceutical Nasal Compositions and Methods for Peptid Treatment
(19) TZZ ¥Z_T (11) EP 2 283 850 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.: of the grant of the patent: A61K 31/485 (2006.01) A61K 9/107 (2006.01) 25.04.2018 Bulletin 2018/17 A61K 9/08 (2006.01) A61K 38/02 (2006.01) A61K 38/25 (2006.01) A61K 31/12 (2006.01) (2006.01) (2006.01) (21) Application number: 10186116.9 A61K 31/365 A61K 9/00 A61K 47/32 (2006.01) A61K 47/22 (2006.01) A61K 47/06 (2006.01) A61K 47/08 (2006.01) (22) Date of filing: 07.03.2005 A61K 47/10 (2017.01) A61K 47/18 (2017.01) A61K 47/44 (2017.01) (54) Pharmaceutical nasal compositions and methods for peptid treatment Pharmazeutische nasale Zubereitungen und Peptidbehandlungen Compositions pharmaceutiques nasales et traitements aux peptides (84) Designated Contracting States: • Reppucci, Carl AT BE BG CH CY CZ DE DK EE ES FI FR GB GR North Andover, MA 01845 (US) HU IE IS IT LI LT LU MC NL PL PT RO SE SI SK TR (74) Representative: Chajmowicz, Marion et al (30) Priority: 05.03.2004 US 895465 Becker & Associés 25, rue Louis Le Grand (43) Date of publication of application: 75002 Paris (FR) 16.02.2011 Bulletin 2011/07 (56) References cited: (62) Document number(s) of the earlier application(s) in WO-A-03/000158 accordance with Art. 76 EPC: 05724894.0 / 1 773 369 Remarks: Thefile contains technical information submitted after (73) Proprietor: CPEX Pharmaceuticals, Inc. the application was filed and not included in this Exeter, NH 03833 (US) specification (72) Inventors: • Gyurik, Robert Exeter, NH 03833 (US) Note: Within nine months of the publication of the mention of the grant of the European patent in the European Patent Bulletin, any person may give notice to the European Patent Office of opposition to that patent, in accordance with the Implementing Regulations. -

2009-2010 Catalogue Peptide
20092010 Peptide Catalogue Generic Peptides Cosmetic Peptides Catalogue Peptides Designer BioScience Ltd Designer BioScience Table of Contents Ordering Information........................................................................................................................................2 Terms and Conditions.......................................................................................................................................3 Generic Peptides...............................................................................................................................................5 Cosmetic peptides...........................................................................................................................................10 Catalogue Peptides..........................................................................................................................................11 Custom Peptide Synthesis.............................................................................................................................292 Alphabetical Index........................................................................................................................................294 Catalogue Number Index..............................................................................................................................319 Designer BioScience Ltd, St John's Innovation Centre, Cambridge, CB4 0WS, United Kingdom Tel.: +44 (0) 1223 322931 Fax: +44 (0) 808 2801 506 [email protected] -

Part 7. Indexes
Peptide Sequences Index Part 7. Indexes Index A. Peptide Sequences White & White - Proteins, Peptides & Amino Acids SourceBook 975 Peptide Sequences Index Ala-Ala-Pro-Lys . 218 A Ala-Ala-Pro-Met . 218 Ala-Ala-Pro-Nle . 218 Abu-Ala· 208 Ala-Ala-Pro-Nva . 218 Abu-Arg . 208, 740 Ala-Ala-Pro-Orn • 218 Abu-Asn-Arg-Leu-Glu-Ala-Ser-Ser-Arg-Ser-Ser-Lys . 208 Ala-Ala-Pro-Phe . 209, 218, 219, 385 Abu-Gly . 208, 369 Ala-Ala-Pro-Val . 217, 219, 220 Abu-Ile-His-Pro-Phe-His-Leu-Val-Ile-His-Thr· 208 Ala-Ala-Ser-Thr-Thr-Thr-Asn-Tyr-Thr . 220 Abu-Ser-Gln-Asn-Tyr-Pro-lie-Val-Gin· 208 Ala-Ala-Trp-Phe-Lys· 220 Abz-Ala-Ala-Phe-Phe . 208 Ala-Ala-Trp-Phe-Pro-pro-Nle . 220 Abz-Ala-Arg-Val-Nle-Phe-Glu-Ala-Nle . 208 Ala-Ala-Tyr . 221 Abz-Ala-Gly-Leu-Ala . 208 Ala-Ala-Tyr-Ala . 221 Abz-Ala-Phe-Ala-Phe-Asp-Val-Phe-Tyr-Asp . 209 Ala-Ala-Tyr-Ala-Ala . 221 Abz-Arg-Val-Lys-Arg-Gly-Leu-Ala-Tyr-Asp . 209 Ala-Ala-Val· 221, 222 Abz-Arg-Val-Nle-Phe-Glu-Ala-Nle . 209 Ala-Ala-Val-Ala • 221, 222 Abz-Gln-Val-Val-Ala-Gly-Ala . 209 Ala-Ala-Val-Ala-Leu-Leu-Pro-Ala-Val-Leu-Leu-Ala-Leu-Leu- Abz-Glu-Thr-Leu-Phe-Gln-Gly-Pro-Val-Phe . 209 Ala-Pro-Asp-Glu-Val-Asp . 221 Abz-Gly . 209, 385 Ala-Ala-Val-Ala-Leu-Leu-Pro-Ala-Val-Leu-Leu-Ala-Leu-Leu Abz-Gly-Ala-Ala-Pro-Phe-Tyr-Asp . -

Ab136942 – LVV Hemorphin 7 ELISA Kit
ab136942 – LVV Hemorphin 7 ELISA Kit Instructions for Use For the quantitative measurement of LVV Hemorphin 7 concentrations in serum and tissue homogenate samples. This product is for research use only and is not intended for diagnostic use. 1 Table of Contents 1. Introduction 3 2. Principle of the Assay 4 3. Assay Summary 5 4. Kit Contents 6 5. Storage and Handling 7 6. Additional Materials Required 7 7. Protocol 8 8. Calculation of Results 15 9. Performance Characteristics 17 10. Troubleshooting 22 2 1. Introduction ab136942 is a complete kit for the quantitative determination of LVV Hemorphin 7 in serum and tissue homogenates, with results in three hours. Please read the entire kit insert before performing this assay. This kit is not intended for use with plasma samples. Hemorphins are opioid peptides derived by proteolysis from hemoglobin. Their sequences are identical in several mammalian species including human, sheep and bovine. LVV‐hemorphin 7 (LVVYPWTQRF) binds strongly to the Angiotensin IV (AT4) receptors in the brain. The AT4 receptor is an integral membrane aminopeptidase also known as IRAP (insulin‐ regulated membrane aminopeptidase). LVV‐hemorphin 7 and AT4 are not substrates but rather inhibitors of the AT4 (IRAP) receptor. Both promote learning and memory and reverse amnesia in animal models. Elevated serum levels of LVV Hemorphin 7 have also been documented in patients with some forms of breast cancers that are associated with an increased expression of Cathespins B and D. 3 2. Principle of the Assay 1. Standards and samples are added to wells coated with a GxR IgG antibody. -

(12) Patent Application Publication (10) Pub. No.: US 2008/0124279 A1 Andremont Et Al
US 2008O124279A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2008/0124279 A1 Andremont et al. (43) Pub. Date: May 29, 2008 (54) COLONIC DELIVERY USING ZN/PECTIN (52) U.S. Cl. .......................................... 424/9.1; 424/493 BEADS WITH AEUDRAGT COATING (76) Inventors: Antoine Andremont, Malakoff (FR); Helene Huguet, Paris (FR) (57) ABSTRACT Correspondence Address: Drug delivery systems that can deliver therapeutic and/or INTELLECTUAL PROPERTY f TECHNOLOGY diagnostic agents to the colon are disclosed. The systems LAW include pectin beads crosslinked with Zinc or any divalent PO BOX 14329 cation of interest, which beads are then coated with RESEARCH TRIANGLE PARK, NC 27709 Eudragit R-type polymers. The drug delivery systems are orally administrable, but can deliver the active agents to the (21) Appl. No.: 11/985.465 colon. In some embodiments, they can administer the agents to various positions in the gastro-intestinal tract, including the (22) Filed: Nov. 15, 2007 colon. The agent can be a small molecule, peptide, protein, nucleic acid, or complex structures of natural, recombinant or Related U.S. Application Data synthetic origin. In still other embodiments, the agent is a diagnostic agent. The agents can be used to diagnose, treat or (60) Provisional application No. 60/859,600, filed on Nov. investigate humans and animals for a variety of conditions, 17, 2006. including infectious diseases, inflammatory diseases, cancers O O and the like. Colon-specific delivery is obtained by formulat Publication Classification ing a prophylactic, therapeutic, and/or diagnostic agent with (51) Int. Cl. specific polymers that degrade in the colon, Such as pectin. -
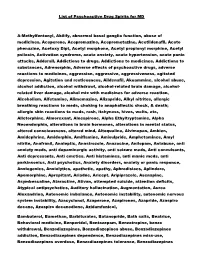
List of Psychoactive Drug Spirits for MD A-Methylfentanyl, Abilify
List of Psychoactive Drug Spirits for MD A-Methylfentanyl, Abilify, abnormal basal ganglia function, abuse of medicines, Aceperone, Acepromazine, Aceprometazine, Acetildenafil, Aceto phenazine, Acetoxy Dipt, Acetyl morphone, Acetyl propionyl morphine, Acetyl psilocin, Activation syndrome, acute anxiety, acute hypertension, acute panic attacks, Adderall, Addictions to drugs, Addictions to medicines, Addictions to substances, Adrenorphin, Adverse effects of psychoactive drugs, adverse reactions to medicines, aggression, aggressive, aggressiveness, agitated depression, Agitation and restlessness, Aildenafil, Akuammine, alcohol abuse, alcohol addiction, alcohol withdrawl, alcohol-related brain damage, alcohol- related liver damage, alcohol mix with medicines for adverse reaction, Alcoholism, Alfetamine, Alimemazine, Alizapride, Alkyl nitrites, allergic breathing reactions to meds, choking to anaphallectic shock, & death; allergic skin reactions to meds, rash, itchyness, hives, welts, etc, Alletorphine, Almorexant, Alnespirone, Alpha Ethyltryptamine, Alpha Neoendorphin, alterations in brain hormones, alterations in mental status, altered consciousness, altered mind, Altoqualine, Alvimopan, Ambien, Amidephrine, Amidorphin, Amiflamine, Amisulpride, Amphetamines, Amyl nitrite, Anafranil, Analeptic, Anastrozole, Anazocine, Anilopam, Antabuse, anti anxiety meds, anti dopaminergic activity, anti seizure meds, Anti convulsants, Anti depressants, Anti emetics, Anti histamines, anti manic meds, anti parkinsonics, Anti psychotics, Anxiety disorders, -

Molecular Insights Into the Interaction of Hemorphin and Its Targets
www.nature.com/scientificreports OPEN Molecular insights into the interaction of hemorphin and its targets Received: 21 January 2019 Amanat Ali1, Bincy Baby1, Soja Saghar Soman2 & Ranjit Vijayan1 Accepted: 17 September 2019 Hemorphins are atypical endogenous opioid peptides produced by the cleavage of hemoglobin beta Published: xx xx xxxx chain. Several studies have reported the therapeutic potential of hemorphin in memory enhancement, blood regulation, and analgesia. However, the mode of interaction of hemorphin with its target remains largely elusive. The decapeptide LVV-hemorphin-7 is the most stable form of hemorphin. It binds with high afnity to mu-opioid receptors (MOR), angiotensin-converting enzyme (ACE) and insulin-regulated aminopeptidase (IRAP). In this study, computational methods were used extensively to elucidate the most likely binding pose of mammalian LVV-hemorphin-7 with the aforementioned proteins and to calculate the binding afnity. Additionally, alignment of mammalian hemorphin sequences showed that the hemorphin sequence of the camel harbors a variation – a Q > R substitution at position 8. This study also investigated the binding afnity and the interaction mechanism of camel LVV-hemorphin-7 with these proteins. To gain a better understanding of the dynamics of the molecular interactions between the selected targets and hemorphin peptides, 100 ns molecular dynamics simulations of the best-ranked poses were performed. Simulations highlighted major interactions between the peptides and key residues in the binding site of the proteins. Interestingly, camel hemorphin had a higher binding afnity and showed more interactions with all three proteins when compared to the canonical mammalian LVV-hemorphin-7. Thus, camel LVV-hemorphin-7 could be explored as a potent therapeutic agent for memory loss, hypertension, and analgesia. -

Opioid Receptor
Opioid Receptor Opioid receptors are a group of G protein-coupled receptors with opioids as ligands. The endogenous opioids are dynorphins, enkephalins, endorphins, endomorphins and nociceptin. Opioid receptors are distributed widely in the brain, and are found in the spinal cord and digestive tract. Opioid receptors are molecules, or sites, within the body that are activated by opioid substances. Opioid receptors inhibit the transmission of impulse in excitatory pathways within the human body system. These pathways include the serotonin, catecholamine, and substance P pathways, which are all implicated in pain perception and feelings of well-being. Opioid receptors are further subclassified into mu, delta, and kappa receptors. All the classes, while exhibiting differing modes of action, share some basic similarities. They all are driven by the potassium pump mechanism, which is found on the plasma membrane of the majority of cells. www.MedChemExpress.com 1 Opioid Receptor Agonists, Antagonists, Inhibitors, Activators & Modulators 6'-GNTI dihydrochloride 6-Alpha Naloxol Cat. No.: HY-110302 (Alpha-Naloxol) Cat. No.: HY-12799 6'-GNTI dihydrochloride, a κ-opioid receptor (KOR) 6-Alpha Naloxol(Alpha-Naloxol) is an opioid agonist, displays bias toward the activation of G antagonist closely related to naloxone; a human protein-mediated signaling over β-arrestin2 metabolite of naloxone. recruitment. 6'-GNTI 6'-GNTI dihydrochloride only activates the Akt pathway in striatal neurons. Purity: >98% Purity: >98% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 1 mg, 5 mg Size: 1 mg, 5 mg 6-beta-Naloxol D5 hydrochloride Ac-RYYRIK-NH2 (6β-Naloxol D5 hydrochloride) Cat. No.: HY-12780S Cat. -

(12) Patent Application Publication (10) Pub. No.: US 2015/0018530 A1 Miao Et Al
US 201500 18530A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2015/0018530 A1 Miao et al. (43) Pub. Date: Jan. 15, 2015 (54) NOVEL PRODRUG CONTAINING Related U.S. Application Data MOLECULE COMPOSITIONS AND THEIR (60) Provisional application No. 61/605,072, filed on Feb. USES 29, 2012, provisional application No. 61/656,981, (71) Applicant: Ambrx, Inc., La Jolla, CA (US) filed on Jun. 7, 2012. (72) Inventors: Zhenwei Miao, San Diego, CA (US); Publication Classification Ho Sung Cho, San Diego, CA (US); Bruce E. Kimmel, Leesburg, VA (US) (51) Int. Cl. A647/48 (2006.01) (73) Assignee: AMBRX, INC., La Jolla, CA (US) C07K 6/28 (2006.01) (52) U.S. Cl. (21) Appl. No.: 14/381,196 CPC ....... A6IK 47/48715 (2013.01); C07K 16/2896 (2013.01); A61K 47/48215 (2013.01); A61 K (22) PCT Fled: Feb. 28, 2013 47/48284 (2013.01); A61K 47/48384 (2013.01) USPC ....................................................... 530/387.3 (86) PCT NO.: PCT/US2O13/028332 S371 (c)(1), (57) ABSTRACT (2) Date: Aug. 26, 2014 Novel prodrug compositions and uses thereof are provided. Patent Application Publication Jan. 15, 2015 Sheet 1 of 21 US 201S/0018530 A1 FIGURE 1. Antigen recognition site Hinge Peptide Patent Application Publication Jan. 15, 2015 Sheet 2 of 21 US 2015/0018530 A1 FIGURE 2 M C7 leader VH(108) (GGGGS)4 VL(108) Y96xs His A. ( +PEG ) His 144 Tyr190 Lys248 Ser136am (+PEG) Leu156 B. 6X His VH(108) (GGGGS)4 VL(108) H, is Leu156 g3 ST lear VL (108) Ck(hu) VH(108) CH1(hu) 6X His - SD L I (AA SP re A Lys 142 am Thr204 am Lys219 am Patent Application Publication Jan. -

(12) Patent Application Publication (10) Pub. No.: US 2003/0069170 A1 Soltero Et Al
US 2003OO6917OA1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2003/0069170 A1 Soltero et al. (43) Pub. Date: Apr. 10, 2003 (54) PHARMACEUTICAL COMPOSITIONS OF Related U.S. Application Data DRUG-OLIGOMER CONJUGATES AND METHODS OF TREATING DSEASES (60) Provisional application No. 60/318,193, filed on Sep. THEREWITH 7, 2001. Provisional application No. 60/377,865, filed on May 3, 2002. (76) Inventors: Richard Soltero, Holly Springs, NC Publication Classification (US); Nnochiri N. Ekwuribe, Cary, NC 5 1. Int.nt. Cl."Cl. ......................... A61K 38/23 ; A61K 31/56;5 (US); Foyeke Opawale, Raleigh, NC A61K 31/202; A61K 38/00 (US); Bruce Rehlander, Chapel Hill, NC (US); Anthony Hickey, Chapel (52) U.S. Cl. ................ 514/2; 514/12; 514/171; 514/560 Hill, NC (US); Bovet Li Li, Chapel Hill, NC (US) (57) ABSTRACT Pharmaceutical compositions that include a drug-oligomer Correspondence Address: conjugate, a fatty acid component, and a bile Salt component MYERS BIGELSIBLEY & SAJOVEC are described. The drug is covalently coupled to an oligo PO BOX 37428 meric moiety. The fatty acid component and the bile Salt RALEIGH, NC 27627 (US) component are present in a weight-to-weight ratio of between 1:5 and 5:1. Methods of treating diseases in a (21) Appl. No.: 10/235,284 Subject in need of Such treatment using Such pharmaceutical compositions are also provided, as are methods of providing (22) Filed: Sep. 5, 2002 Such pharmaceutical compositions. Patent Application Publication Apr. 10, 2003 Sheet 1 of 13 US 2003/0069170 A1 InáHI9 s (p16u) GSO3nS eu Sal Patent Application Publication Apr. -

Datasheet Inhibitors / Agonists / Screening Libraries a DRUG SCREENING EXPERT
Datasheet Inhibitors / Agonists / Screening Libraries A DRUG SCREENING EXPERT Product Name : Valorphin TFA(144313-54-2(free bas)) Catalog Number : T7666 CAS Number : T7666 Molecular Formula : C46H62F3N9O13 Molecular Weight : 1006.03 Description: Valorphin TFA is a semisynthetic derivative of dihydrovaltrate with opioid analgesic activity Storage: 2 years -80°C in solvent; 3 years -20°C powder; In vitro Activity In vitro binding studies using brain homogenates from rat and guinea-pig indicate a preference for the mu-receptor site. Bath application to cultured cerebellar Purkinje cells inhibited the spontaneous firing, similar to the effect seen with morphine. Analgesic activity has been demonstrated in the hot plate and the tail flick test in the mouse and the Randall-Selitto test in the rat. In the rhesus monkey valorphin was self-administered, but naloxone challenge induced only mild withdrawal signs. Valorphin is a novel chemical entity, structurally not related to known opioids, which interacts preferentially with opiate mu- receptors[1]. Reference 1. Maurer R , R Mer D , H.H. Büscher, et al. Valorphin: A novel chemical structure with opioid activity[J]. Neuropeptides, 1985, 5(4-6):387-390. 2. Smith W D . A COMPARISON IN MICE OF NALOXONE AND NALORPHINE AS ANTAGONISTS TO NEUROLEPTANALGESIC DRUGS[J]. BJA: British Journal of Anaesthesia(11):11. FOR RESEARCH PURPOSES ONLY. NOT FOR DIAGNOSTIC OR THERAPEUTIC USE. Information for product storage and handling is indicated on the product datasheet. Targetmol products are stable for long term under the recommended storage conditions. Our products may be shipped under different conditions as many of them are stable in the short-term at higher or even room temperatures. -

(12) Patent Application Publication (10) Pub. No.: US 2004/0152769 A1 Ekwuribe Et Al
US 2004O152769A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2004/0152769 A1 Ekwuribe et al. (43) Pub. Date: Aug. 5, 2004 (54) MODIFIED CARBAMATE-CONTAINING (52) U.S. Cl. ........................... 514,478; 514/615; 514/114 PRODRUGS AND METHODS OF SYNTHESIZING SAME (57) ABSTRACT (76) Inventors: Nnochiri Nkem Ekwuribe, Cary, NC (US); Jennifer Riggs-Sauthier, Prodrugs having a hydrolyzable carbamate moiety, compo Raleigh, NC (US); Tatyana A. Sitions including the prodrugs, methods of preparing the Dyakonov, Durham, NC (US) prodrugs and methods of treatment using the prodrugs are Correspondence Address: disclosed. The prodrug has the formula DC(X)XR, where D is a biologically active agent, X is O, S or NR', and R is a SS SIBLEY & SAJOVEC moiety that modifies various properties of the biologically RALEIGH, NC 27627 (US active agent. The biologically active agent either includes a 9 (US) functional group Such as an amide, thioamide, imide, thio imide, urea, thiourea, carbamate, thiocarbamate, Sulfona (21) Appl. No.: 10/703,647 mide, or Sulfonimide group, or includes a hydroxy, amine, 22) Filled: 7, 2003 carboxylic acid or thiol group that is modified to include (22) File Nov. 7, Such a group. An NH group from the biologically active Related U.S. Application Data agent can be coupled to an activated form the C(X)XR moiety to form the prodrugs described herein. Relative to a (60) Provisional application No. 60/424,796, filed on Nov. conventional carbamate group, the presence of the addi 9, 2002. Provisional application No. 60/483,676, filed tional carbonyl or Sulfonyl group makes the carbamate on Jun.