Ownership, Coverage, Utilisation and Maintenance of Long
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dictionnaire Des Villages Du Fako : Village Dictionary of Fako Division
OFFICE DE LA RECHERCHE SCIENTIFIOUE ET TECHNIOUE OUTRE· MER Il REPUBLIQUE UNIE DU CAMEROUN DICTIONNAIRE DES VILLAGES DU FAKO VILLAGE DICTIONARY OF FAKO DIVISION SECTION DE GEOGRAPHIE 1 OFFICE DE LA RECHERCHE SCIm~TIFIQUE REPUBLIQUE UNIE ET TECmUQUE OUTRE-lViER DU CAlvŒROUN UNITED REPUBLIC OF CANEROON CENTRE O.R.S.T.O.N DE YAOUNDE DICTIONNAIRE DES VILLAGES DU FAKO VILLAGE DICTIONARY OF FAKO DIVISION Juillet 1973 July 1973 COPYRIGHT O.R.S.T.O.M 1973 TABLE DES NATIERES CONTENTS i l j l ! :i i ~ Présentation •••••.•.•.....••....•.....•....••••••.••.••••••.. 1 j Introduction ........................................•• 3 '! ) Signification des principaux termes utilisés •.............• 5 î l\lIeaning of the main words used Tableau de la population du département •...••.....•..•.•••• 8 Population of Fako division Département du Fako : éléments de démographie •.•.... ..••.•• 9 Fako division: demographic materials Arrondissements de Muyuka et de Tiko : éléments de . démographie 0 ••••••••••••••••••••••••••••••••••••••• 10 11uyul{a and Tileo sl)..bdivisions:demographic materials Arrondissement de Victoria: éléments de démographie •••.••• 11 Victoria subdivision:demographic materials Les plantations (12/1972) •••••••••••.•••••••••••••••••••••• 12 Plantations (12/1972) Liste des villages par arrondissement, commune et graupement 14 List of villages by subdivision, area council and customary court Signification du code chiffré •..•••...•.•...•.......•.•••.• 18 Neaning of the code number Liste alphabétique des villages ••••••.••••••••.•.•..•••.•.• 19 -

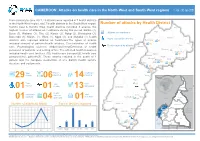
Shelter Cluster Dashboard NWSW052021
Shelter Cluster NW/SW Cameroon Key Figures Individuals Partners Subdivisions Cameroon 03 23,143 assisted 05 Individual Reached Trend Nigeria Furu Awa Ako Misaje Fungom DONGA MANTUNG MENCHUM Nkambe Bum NORD-OUEST Menchum Nwa Valley Wum Ndu Fundong Noni 11% BOYO Nkum Bafut Njinikom Oku Kumbo Belo BUI Mbven of yearly Target Njikwa Akwaya Jakiri MEZAM Babessi Tubah Reached MOMO Mbeggwi Ngie Bamenda 2 Bamenda 3 Ndop Widikum Bamenda 1 Menka NGO KETUNJIA Bali Balikumbat MANYU Santa Batibo Wabane Eyumodjock Upper Bayang LEBIALEM Mamfé Alou OUEST Jan Feb Mar Apr May Jun Jul Aug Sep Oct Nov Dec Fontem Nguti KOUPÉ HNO/HRP 2021 (NW/SW Regions) Toko MANENGOUBA Bangem Mundemba SUD-OUEST NDIAN Konye Tombel 1,351,318 Isangele Dikome value Kumba 2 Ekondo Titi Kombo Kombo PEOPLE OF CONCERN Abedimo Etindi MEME Number of PoC Reached per Subdivision Idabato Kumba 1 Bamuso 1 - 100 Kumba 3 101 - 2,000 LITTORAL 2,001 - 13,000 785,091 Mbongé Muyuka PEOPLE IN NEED West Coast Buéa FAKO Tiko Limbé 2 Limbé 1 221,642 Limbé 3 [ Kilometers PEOPLE TARGETED 0 15 30 *Note : Sources: HNO 2021 PiN includes IDP, Returnees and Host Communi�es The boundaries and names shown and the designations used on this map do not imply official endorsement or acceptance by the United Nations Key Achievement Indicators PoC Reached - AGD Breakdouwn 296 # of Households assisted with Children 27% 26% emergency shelter 1,480 Adults 21% 22% # of households assisted with core 3,769 Elderly 2% 2% relief items including prevention of COVID-19 21,618 female male 41 # of households assisted with cash for rental subsidies 41 Households Reached Individuals Reached Cartegories of beneficiaries reported People Reached by region Distribution of Shelter NFI kits integrated with COVID 19 KITS in Matoh town. -
MINMAP South-West Region
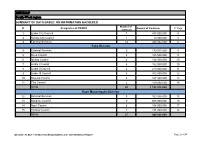
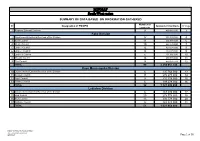
MINMAP South-West region SUMMARY OF DATA BASED ON INFORMATION GATHERED Number of N° Designation of PO/DPO Amount of Contracts N° Page contracts 1 Limbe City Council 7 475 000 000 4 2 Kumba City Council 1 10 000 000 5 3 External Services 14 440 032 000 6 Fako Division 4 External Services 9 179 015 000 8 5 Buea Council 5 125 500 000 9 6 Idenau Council 4 124 000 000 10 7 Limbe I Council 4 152 000 000 10 8 Limbe II Council 4 219 000 000 11 9 Limbe III Council 6 102 500 000 12 10 Muyuka Council 6 127 000 000 13 11 Tiko Council 5 159 000 000 14 TOTAL 43 1 188 015 000 Kupe Muanenguba Division 12 External Services 5 100 036 000 15 13 Bangem Council 9 605 000 000 15 14 Nguti Council 6 104 000 000 17 15 Tombel Council 7 131 000 000 18 TOTAL 27 940 036 000 MINMAP / PUBLIC CONTRACTS PROGRAMMING AND MONITORING DIVISION Page 1 of 34 MINMAP South-West region SUMMARY OF DATA BASED ON INFORMATION GATHERED Lebialem Division 16 External Services 5 134 567 000 19 17 Alou Council 9 144 000 000 19 18 Menji Council 3 181 000 000 20 19 Wabane Council 9 168 611 000 21 TOTAL 26 628 178 000 Manyu Division 18 External Services 5 98 141 000 22 19 Akwaya Council 6 119 500 000 22 20 Eyomojock Council 6 119 000 000 23 21 Mamfe Council 5 232 000 000 24 22 Tinto Council 6 108 000 000 25 TOTAL 28 676 641 000 Meme Division 22 External Services 5 85 600 000 26 23 Mbonge Council 7 149 000 000 26 24 Konye Council 1 27 000 000 27 25 Kumba I Council 3 65 000 000 27 26 Kumba II Council 5 83 000 000 28 27 Kumba III Council 3 84 000 000 28 TOTAL 24 493 600 000 MINMAP / PUBLIC CONTRACTS -
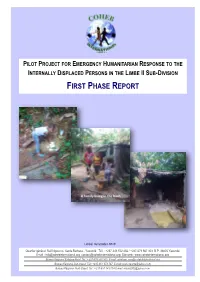
First Phase Report
Page 1 PILOT PROJECT FOR EMERGENCY HUMANITARIAN RESPONSE TO THE INTERNALLY DISPLACED PERSONS IN THE LIMBE II SUB-DIVISION FIRST PHASE REPORT A family living in the bush Limbé, December 2018 Quartier général: Rail Ngousso- Santa Barbara - Yaoundé Tél. : +237-243 572 456 / +237-679 967 303 B.P. 33805 Yaoundé Email : [email protected] [email protected] Site web : www.cohebinternational.org Bureau Régional Extrême-Nord: Tél.: +237-674 900 303 E-mail: [email protected] Bureau Régional Sud-Ouest: Tél.: +237-651 973 747 E-mail: [email protected] Bureau Régional Nord-Ouest: Tél.: +237-697 143 004 E-mail: [email protected] Emergency response to Limbe II IDPs - December 2018 Page 2 TABLE OF CONTENT PRESENTATION OF COHEB INT’L ................................................................. 3 SOME OF OUR EMERGENCY ACTIVITIES ......................................................... 4 CONTEXT OF THE PROJECT .......................................................................... 5 OBJECTIVE OF THE PROJECT ........................................................................ 6 EXECUTION OF THE PROJECT .................................................................... 7-9 CONCLUSION ............................................................................................ 10 ANNEX 1: IDP’S SETTLEMENT CAMP MUKUNDANGE LIMBE II SUB-DIVISION......................................................... 11 ANNEX 2: COHEB PROJECT OFFICE SOKOLO, LIMBE II OUR AGRO-FORESTRY TRANSFORMATION FACTORY AND LOGISTICS -

Country Travel Risk Summaries
COUNTRY RISK SUMMARIES Powered by FocusPoint International, Inc. Report for Week Ending September 19, 2021 Latest Updates: Afghanistan, Burkina Faso, Cameroon, India, Israel, Mali, Mexico, Myanmar, Nigeria, Pakistan, Philippines, Russia, Saudi Arabia, Somalia, South Sudan, Sudan, Syria, Turkey, Ukraine and Yemen. ▪ Afghanistan: On September 14, thousands held a protest in Kandahar during afternoon hours local time to denounce a Taliban decision to evict residents in Firqa area. No further details were immediately available. ▪ Burkina Faso: On September 13, at least four people were killed and several others ijured after suspected Islamist militants ambushed a gendarme patrol escorting mining workers between Sakoani and Matiacoali in Est Region. Several gendarmes were missing following the attack. ▪ Cameroon: On September 14, at least seven soldiers were killed in clashes with separatist fighters in kikaikelaki, Northwest region. Another two soldiers were killed in an ambush in Chounghi on September 11. ▪ India: On September 16, at least six people were killed, including one each in Kendrapara and Subarnapur districts, and around 20,522 others evacuated, while 7,500 houses were damaged across Odisha state over the last three days, due to floods triggered by heavy rainfall. Disaster teams were sent to Balasore, Bhadrak and Kendrapara districts. Further floods were expected along the Mahanadi River and its tributaries. ▪ Israel: On September 13, at least two people were injured after being stabbed near Jerusalem Central Bus Station during afternoon hours local time. No further details were immediately available, but the assailant was shot dead by security forces. ▪ Mali: On September 13, at least five government soldiers and three Islamist militants were killed in clashes near Manidje in Kolongo commune, Macina cercle, Segou region, during morning hours local time. -
MINMAP South-West Region
MINMAP South-West region SUMMARY OF DATA BASED ON INFORMATION GATHERED Number of N° Designation of PO/DPO Amount of Contracts N° Page contracts 1 Regional External Services 9 490 982 000 3 Fako Division 2 Départemental External Services of the Division 17 352 391 000 4 3 Buea Council 11 204 778 000 6 4 Idenau Council 10 224 778 000 7 5 Limbe I Council 12 303 778 000 8 6 Limbe II Council 13 299 279 000 9 7 Limbe III Council 6 151 900 000 10 8 Muyuka Council 16 250 778 000 11 9 Tiko Council 14 450 375 748 12 TOTAL 99 2 238 057 748 Kupe Muanenguba Division 10 Départemental External Services of the Division 6 135 764 000 13 11 Bangem Council 11 572 278 000 14 12 Nguti Council 9 215 278 000 15 13 Tombel Council 6 198 278 000 16 TOTAL 32 1 121 598 000 Lebialem Division 14 Départemental External Services of the Division 6 167 474 000 17 15 Alou Council 20 278 778 000 18 16 Menji Council 13 306 778 000 20 17 Wabane Council 12 268 928 000 21 TOTAL 51 1 021 958 000 PUBLIC CONTRACTS PROGRAMMING AND MONITORING DIVISION /MINMAP Page 1 of 36 MINMAP South-West region SUMMARY OF DATA BASED ON INFORMATION GATHERED Number of N° Designation of PO/DPO Amount of Contracts N° Page contracts Manyu Division 18 Départemental External Services of the Division 9 240 324 000 22 19 Akwaya Council 10 260 278 000 23 20 Eyumojock Council 6 195 778 000 24 21 Mamfe Council 7 271 103 000 24 22 Tinto Council 7 219 778 000 25 TOTAL 39 1 187 261 000 Meme Division 23 Départemental External Services of the Division 4 82 000 000 26 24 Konye Council 5 171 533 000 26 25 Kumba -

South West Assessment
Cameroon Emergency Response – South West Assessment SOUTH WEST CAMEROON November 2018 – January 2019 - i - CONTENTS 1 CONTEXT ..................................................................................................................... 4 1.1 The crisis in numbers:.................................................................................................... 5 1.2 Overall Objectives of SW Assessment ........................................................................... 5 1.3 Area of Intervention ...................................................................................................... 6 2 METHODOLOGY .......................................................................................................... 6 2.1 Assessment site selection: ............................................................................................ 8 2.2 Configuration of the assessment team: ........................................................................ 8 2.3 Indicators of vulnerability verified during the rapid assessment: ................................ 9 2.3.1 Nutrition and Health ............................................................................................. 9 2.3.2 WASH ..................................................................................................................... 9 3.1.1 Food Security ......................................................................................................... 9 2.4 Sources of Information ............................................................................................... -

Health Status of Elderly Population in the Buea Health District, Cameroon
Aging Medicine and Healthcare 2020;11(1):10-19. doi:10.33879/AMH.2020.033-1904.010 Aging Medicine and Healthcare https://www.agingmedhealthc.com Original Article Health Status of Elderly Population in the Buea Health District, Cameroon *Agbor Nathan Emeh1,2, Fongang Che Landis1,3, Tambetakaw Njang Gilbert1,2, Atongno Ashu Humphrey1,2 1University of Buea, Cameroon 2Ministry of Public Health, Yaounde, Cameroon 3Cameroon Christian University, Cameroon ABSTRACT Background/Purpose: The purpose of this study was to assess the socio- clinical profile, heath status and determine the impact of age on health related behaviors of geriatric population in the Buea Health District. Since studies on the subject are lacking in Cameroon, we believe this study provides ground work for further studies on geriatrics in Cameroon. Methods: Two-stage systematic sampling was used. Firstly, 30 communities of the Buea Health District were randomly selected. Eligible participants in these communities were then selected in turns. Interviewer-administered questionnaire, physical examination and health record checks were used to capture the study objectives. Results: Of the 142 sampled elderlies, 57.7% (82/142) were females with the young-old (60-75 years) constituted the majority (69.01%; 98/142). Most of the elderlies (88%; 125/142) had at least one chronic disease, 35.9% (51/142) had *Correspondence at least two and 9.86% (14/142) had at least three chronic diseases. The major Dr. Agbor Nathan Emeh chronic diseases suffered by elderlies included arthritis (38.73%; 55/142), gastritis (38.73%; 55/142) and hypertension (29.58%; 42/142). Most affected Department of Public Health body systems were musculoskeletal (86.62%; 123/142), neurologic (85.21%; and Hygiene, University of 121/142), and eye (76.76%; 109/142). -

Governance of Disaster Risk Reduction in Cameroon: the Need to Empower Local Government
Page 1 of 10 Original Research Governance of disaster risk reduction in Cameroon: The need to empower local government Author: The impact of natural hazards and/or disasters in Cameroon continues to hit local communities 1,2 Henry N. Bang hardest, but local government lacks the ability to manage disaster risks adequately. This Affiliations: is partly due to the fact that the necessity to mainstream disaster risk reduction into local 1African Centre for Disaster governance and development practices is not yet an underlying principle of Cameroon’s Studies, Potchefstroom, disaster management framework. Using empirical and secondary data, this paper analyses South Africa the governance of disaster risks in Cameroon with particular focus on the challenges local 2School of International government faces in implementing disaster risk reduction strategies. The hypothesis is that Development, University the governance of disaster risks is too centralised at the national level, with huge implications of East Anglia, Norwich, for the effective governance of disaster risks at the local level. Although Cameroon has United Kingdom reinvigorated efforts to address growing disaster risks in a proactive way, it is argued that Correspondence to: the practical actions are more reactive than proactive in nature. The overall aim is to explore Henry Bang the challenges and opportunities that local government has in the governance of disaster risks. Based on the findings from this research, policy recommendations are suggested on Email: ways to mainstream disaster risk reduction strategies into local governance, and advance [email protected] understanding and practice in the local governance of disaster risks in the country. Postal address: 37 Whitworth Court, Norwich, NR6 6GN, United Kingdom Introduction Natural hazards continue to pose a major threat to the entire world with prospects of even greater Dates: impacts to life and property in the future (Aini & Fakhrul-Razi 2010; Hayles 2010). -
SSA Infographic
CAMEROON: Attacks on health care in the North-West and South-West regions 1 Jan - 30 Jun 2021 From January to June 2021, 29 attacks were reported in 7 health districts in the North-West region, and 7 health districts in the South West region. Number of attacks by Health District Kumbo East & Kumbo West health districts recorded 6 attacks, the Ako highest number of attacks on healthcare during this period. Batibo (4), Wum Buea (3), Wabane (3), Tiko (2), Konye (2), Ndop (2), Benakuma (2), Attacks on healthcare Bamenda (1), Mamfe (1), Wum (1), Nguti (1), and Muyuka (1) health Injury caused by attacks Nkambe districts also reported attacks on healthcare.The types of attacks Benakuma 01 included removal of patients/health workers, Criminalization of health 02 Nwa Death caused by attacks Ndu care, Psychological violence, Abduction/Arrest/Detention of health Akwaya personnel or patients, and setting of fire. The affected health resources Fundong Oku Kumbo West included health care facilities (10), health care transport(2), health care Bafut 06 Njikwa personnel(16), patients(7). These attacks resulted in the death of 1 Tubah Kumbo East Mbengwi patient and the complete destruction of one district health service Bamenda Ndop 01 Batibo Bali 02 structure and equipments. Mamfe 04 Santa 01 Eyumojock Wabane 03 Total Patient Healthcare 29 Attacks 06 impacted 14 impacted Fontem Nguti Total Total Total 01 Injured Deaths Kidnapping EXTRÊME-NORD Mundemba FAR-NORTH CHAD 01 01 13 Bangem Health Total Ambulance services Konye impacted Detention Kumba North Tombel NONORDRTH 01 04 destroyed 01 02 NIGERIA Bakassi Ekondo Titi Number of attacks by Month Type of facilities impacted AADAMAOUADAMAOUA NORTH- 14 13 NORD-OUESTWEST Kumba South CENTRAL 12 WOUESTEST AFRICAN Mbonge SOUTH- SUD-OUEST REPUBLIC 10 WEST Muyuka CCENTREENTRE 8 01 LLITITTORALTORAL EASESTT 6 5 4 4 Buea 4 03 Tiko 2 Limbe Atlantic SSUDOUTH 1 02 Ocean 2 EQ. -

Restructuring of the Cameroon Development Corporation, Challenges and Coping Strategies of Plantation Workers in Fako Division, South West Region, Cameroon
International Journal of Research in Geography (IJRG) Volume 6, Issue 2, 2020, PP 07-19 ISSN 2454-8685 (Online) http://dx.doi.org/10.20431/2454-8685.0602002 www.arcjournals.org Restructuring of the Cameroon Development Corporation, Challenges and Coping Strategies of Plantation Workers in Fako Division, South West Region, Cameroon Clovis Ebot Obale* Ph.D candidate, Department of Geography University of Yaounde I, Yaounde-Cameroon, Faculty of Arts, letters and Social Sciences, Cameroon *Corresponding Author: Clovis Ebot Obale, Ph.D candidate, Department of Geography University of Yaounde I, Yaounde-Cameroon, Faculty of Arts, letters and Social Sciences, Cameroon Abstract: Industrial restructuring that took place in most developing countries after the mid-1980s failed to take into consideration the working and living conditions of workers, since multinational companies that bought over state owned enterprises focused more on profit maximization at the detriment of workers welfare. This study explores the challenges and coping strategies of workers of the Cameroon Development Corporation (CDC) in the context of neoliberal restructuring masterminded by the Bretton Wood Institutions. The researcher employed a qualitative phenomenological research design with purposeful sampling of participants. Data collection entailed conducting in-depth interviews and focus group discussions with 120 male and female workers drawn from four CDC camps in Fako Division. The study affirms that the restructuring of the CDC had negative consequences on the living and working conditions of workers. In a bid to salvage the situation workers had to reduce their expenditure and diversify their sources of income. The coping strategies that were employed by workers to curb the negative effects of these restructuring failed to ameliorate their living conditions, though little has been done by the CDC, CTE and Delmonte to ameliorate their situation, despite huge sacrifices they have made to restore the CDC to its past glory. -

Press Release Organisation of Mobile Clinic
PRESS RELEASE ORGANISATION OF MOBILE CLINIC ACTIVITIES IN THE SOUTH WEST REGION Buea, February 16th, 2021 - The United Nations Populations Fund (UNFPA) and the Ministry of Public Health in partnership with the Cameroon Baptist Convention Hospital Services will on Thursday February 25th, 2021 set up a mobile clinic in the village of Kosala in the Kumba II Subdivision of Meme Division, South West Region of Cameroon at 7am. The event which falls under the World Bank Pandemic Emergency Financing Facility (PEF) Project run in the North West and South West Regions,aims at: • Reducing preventable maternal and new-born morbidities and mortalities in the North West Region (NWR) within the covid-19 pandemic and ongoing humanitarian crisis. • Reducing unmet need for Family planning in underserved populations and communities in the North West and South West Regions (NWSW) Insecurity, destruction of health infrastructure and ‘ghost towns’ have significantly reduced access to basic health services. During 2018, 175/368 (47%) and 184/368 (50%) facilities reported being affected by the crisis in the first and second half of the year respectively in the NW region (displacement of staff, destruction, difficulties in the supply of medical products, and difficulties in geographical access due to the destruction of roads or barricades/checkpoints). As of December 31, 2019, 9% (33/368) of health facilities in the NW were non-functional, with the health districts of Ako (50%), Batibo (21%), Nkambe (16%) and Bafut (16%) being the most affected, and 3% were partially