New Hire Benefits Information
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pizza Hut 10-Year Single Tenant Absolute NNN Lease Investment 1301 Garth Road | BAYTOWN (HOUSTON), TEXAS
Pizza Hut 10-Year Single Tenant Absolute NNN Lease Investment 1301 Garth Road | BAYTOWN (HOUSTON), TEXAS Confidential Offering Memorandum $1,350,000 Cap Rate: 5.56% NOI: $75,000 Presented by Shireen Owlia | 281.477.4300 | www.newquest.com Contents Table of Table Table of Contents Confidentiality & Disclaimer 3 Investment Summary 4 Investment Highlights 5 Property Overview 6 Financial Overview The Offering 7 Rent Schedule 7 Operating Statement 7 Lease Abstract 8 Tenant Profile 9 Location Overview Houston MSA 10 Baytown Trade Area 12 Information About Brokerage Services 15 Contact: NewQuest Properties 8827 W. Sam Houston Parkway, N. Suite 200 Houston, Texas 77040 Shireen Owlia [email protected] 281.640.7693 *The information herein has been secured from sources we believe to be reliable, but we make no representations or warranties, expressed or implied, as to the accuracy thereof. References to square footage or age are approximate. Buyer must verify the information and bears all risk for any inaccuracies. 2 Confidentiality Disclaimer The information contained in this Offering Memorandum is This Offering Memorandum is furnished to prospective purchasers for the purpose of proprietary and strictly confidential. It is intended to be reviewed determining whether to invest in the subject property offered hereby. This Offering only by the party receiving it from NewQuest Properties and Memorandum has been prepared to provide summary, unverified financial and physical & Confidentiality it should not be made available to any other person or entity information to prospective purchasers, and to establish only a preliminary level of interest Disclaimer without the written consent of NewQuest Properties. By taking in the subject property. -

Volleyball Media Guide 2021 Schedule
LEE♦- COLLEGE .......... ' REBELS & ..,........ REBELSa 2021 ROSTER 1 2 3 4 ASHLYNN LEWIS MARIAH ELLIS JULIANA DAVIS ALISHYA ROMAN FR • 6-1 • MB FR • 6-1 • MB FR • 5-5 •DS/L FR • 5-5 • OH Texas City, TX Russelville, AR Houston, TX Kailua, HI 5 6 7 8 9 GRACIE LEWIS SAMIYA HARRIS DEANNA SPELL SINA TOROSLU CIERRA GILBERT FR • 5-3 • DS/L SO • 5-8 • OH FR • 5-7 • DS/U SO • 6-0 • MB FR • 6-1 • MB League City, TX Detroit, MI Houston, TXs Stuttgart, Germany College Station, TX 10 11 12 13 LEA VENGHAUS IMARI WILSON TRINIDIE DAVIS JANNIE BLAKE FR • 5-7 • S FR • 5-11 • OH/OPP FR • 5-9 • OPP/S FR • 5-6 • S Senden, Germany Humble, TX San Antonio, TX Lā’ie, O’ahu HEAD COACH ASSISTANT COACH ATHLETIC TRAINER DANIELLE ABOLANLE CAITLIN ESSIX “BONDIE” BLACKMORE ONIPEDE 2 LADY REBELS 2021 SEASON LEE COLLEGE VOLLEYBALL MEDIA GUIDE 2021 SCHEDULE DAY DATE OPPONENT LOCATION TIME Saturday August 14 Dillard University Scrimmage New Orleans, LA 11:00 AM Saturday August 14 Pearl River Scrimmage New Orleans, LA 1:00 PM Tuesday August 17 Texas Southern Scrimmage Houston, TX 2:00 PM Friday August 20 Dallas College – Northlake Baytown, TX 1:00 PM Friday August 20 Fort Scott Community College Baytown, TX 5:00 PM Saturday August 21 Dallas College – Cedar Valley Baytown, TX 11:00 AM Saturday August 21 Dallas College – Mountain View Baytown, TX 1:00 PM Saturday August 21 Dallas College – Eastfeld Baytown, TX 5:00 PM Wednesday August 25 Dallas College – Mountain View Dallas, TX 6:00 PM Friday August 27 Pima Community College Arizona Western 9:00 AM (PT) Friday August 27 Glendale -
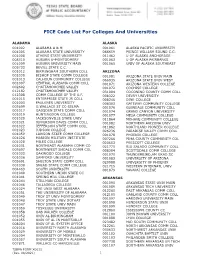
FICE Code List for Colleges and Universities (X0011)
FICE Code List For Colleges And Universities ALABAMA ALASKA 001002 ALABAMA A & M 001061 ALASKA PACIFIC UNIVERSITY 001005 ALABAMA STATE UNIVERSITY 066659 PRINCE WILLIAM SOUND C.C. 001008 ATHENS STATE UNIVERSITY 011462 U OF ALASKA ANCHORAGE 008310 AUBURN U-MONTGOMERY 001063 U OF ALASKA FAIRBANKS 001009 AUBURN UNIVERSITY MAIN 001065 UNIV OF ALASKA SOUTHEAST 005733 BEVILL STATE C.C. 001012 BIRMINGHAM SOUTHERN COLL ARIZONA 001030 BISHOP STATE COMM COLLEGE 001081 ARIZONA STATE UNIV MAIN 001013 CALHOUN COMMUNITY COLLEGE 066935 ARIZONA STATE UNIV WEST 001007 CENTRAL ALABAMA COMM COLL 001071 ARIZONA WESTERN COLLEGE 002602 CHATTAHOOCHEE VALLEY 001072 COCHISE COLLEGE 012182 CHATTAHOOCHEE VALLEY 031004 COCONINO COUNTY COMM COLL 012308 COMM COLLEGE OF THE A.F. 008322 DEVRY UNIVERSITY 001015 ENTERPRISE STATE JR COLL 008246 DINE COLLEGE 001003 FAULKNER UNIVERSITY 008303 GATEWAY COMMUNITY COLLEGE 005699 G.WALLACE ST CC-SELMA 001076 GLENDALE COMMUNITY COLL 001017 GADSDEN STATE COMM COLL 001074 GRAND CANYON UNIVERSITY 001019 HUNTINGDON COLLEGE 001077 MESA COMMUNITY COLLEGE 001020 JACKSONVILLE STATE UNIV 011864 MOHAVE COMMUNITY COLLEGE 001021 JEFFERSON DAVIS COMM COLL 001082 NORTHERN ARIZONA UNIV 001022 JEFFERSON STATE COMM COLL 011862 NORTHLAND PIONEER COLLEGE 001023 JUDSON COLLEGE 026236 PARADISE VALLEY COMM COLL 001059 LAWSON STATE COMM COLLEGE 001078 PHOENIX COLLEGE 001026 MARION MILITARY INSTITUTE 007266 PIMA COUNTY COMMUNITY COL 001028 MILES COLLEGE 020653 PRESCOTT COLLEGE 001031 NORTHEAST ALABAMA COMM CO 021775 RIO SALADO COMMUNITY COLL 005697 NORTHWEST -

Lee College President
Lee College President Dr. Lynda Villanueva As an administrator and leader with more than 20 years of experience in higher education, Dr. Lynda Villanueva is known for her bold and innovative leadership style, as well as her strategic approach to student success. Dr. Villanueva became the tenth president of Lee College in September 2019 and began her duties as president of the College in December 2019. As the first ethnic minority president in Lee College’s 86 year history, Dr. Villanueva has a passion for equity in education and believes in making every student feel valued and accepted, regardless of their background. During her first year as president of Lee College, Dr. Villanueva led the institution's transformation as it expanded its services to include virtual and hybrid learning modalities as a result of the COVID-19 pandemic. She also oversaw the implementation of a free tuition program for graduates of local independent school districts, which resulted in increased student enrollment at Lee College amid global economic hardship. Before becoming president of Lee College, Dr. Villanueva served as Provost and Vice President for Academic and Student Affairs at Brazosport College in Lake Jackson, Texas. Prior to that, she served as Dean of Instruction at Brazosport College. Dr. Villanueva earned a doctor of philosophy degree in industrial/organizational psychology; a master of arts in psychology from the University of Houston; and a bachelor of science in psychology from Colorado State University in Fort Collins, Colo. She is an Aspen Presidential Fellow, a Data Coach for Achieving the Dream, and a board member for the United Way of Greater Baytown Area and Chambers County, 1 Baytown Chamber of Commerce, Economic Alliance, and a member of the Rotary Club of Baytown. -

List of State Agencies and Higher Education Institutions
List of State Agencies and Institutions of Higher Education (List may not be all inclusive) Abilene State Supported Living Center Civil Commitment Office, Texas Fire Protection, Commission on Accountancy, Board of Public Clarendon College Forest Service, Texas Administrative Hearings, Office of Coastal Bend College Frank Phillips College Affordable Housing Corporation College of the Mainland Funeral Service Commission Aging and Disability Services, Dept. of Collin County Community College Galveston College Agriculture, Department of Competitive Government, Council on Geoscientists, Board of Professional AgriLife Extension Service, Texas Comptroller of Public Accounts Governor, Office of the AgriLife Research, Texas Consumer Credit Commissioner, Office of Grayson County College Alamo Community College District Corpus Christi State Supported Groundwater Protection Committee Alcoholic Beverage Commission County and District Retirement System Guadalupe-Blanco River Authority Alvin Community College Court Administration, Office of Gulf Coast Waste Disposal Authority Amarillo College Credit Union Department Headwaters Groundwater Conservation Anatomical Board Criminal Appeals, Court of Health and Human Services Commission Angelina and Neches River Authority Criminal Justice, Department of Health Professions Council Angelina College Dallas County Community College Health Services, Department of State Angelo State University Deaf, School for the High Plains Underground Water Conserv. Animal Health Commission Del Mar College Higher Education Coordinating -

PLEASE TAKE NOTICE That the Board of Trustees for the Lone Star College System Will Hold an Election on the 3Rd Day of November 2020 for Trustees in Districts No
NOTICE OF SCHOOL TRUSTEE ELECTION AVISO DE ELECCIÓN DE SÍNDICOS ESCOLARES THÔNG BÁO VỀ CUỘC BẦU CỬ ỦY VIÊN QUẢN TRỊ NHÀ TRƯỜNG 學校理事選舉通知 PLEASE TAKE NOTICE that the Board of Trustees for the Lone Star College System will hold an election on the 3rd day of November 2020 for Trustees in Districts No. 3 and 9 on the Board of the System. The Board shall conduct a joint election with Harris County. Harris County Elections Services shall conduct the election for the System at the designated polling sites for early voting and on Election Day within Harris County. Notice is hereby given that the polling places listed in Exhibit A will be open from 7:00 a.m. to 7:00 p.m. on November 3, 2020 for voting in this election. Early voting by personal appearance shall begin on October 13, 2020 and continue through October 30, 2020 as listed in Exhibit B. NOTIFÍQUESE que la Junta de Síndicos del Sistema de Lone Star College celebrará una elección el tercer día de noviembre de 2020 para Síndicos de los Distritos Nro. 3 y 9 de la Junta del Sistema. La Junta llevará a cabo una elección conjunta con el Condado de Harris. Los Servicios Electorales del Condado de Harris llevarán a cabo la elección para el Sistema en los lugares de votación designados para la votación anticipada y el Día de Elección dentro del Condado de Harris. Se notifica por el presente que los lugares de votación indicados en el Anexo A estarán abiertos de 7:00 a.m. -

Lee College Quick Facts 2018-2019
QUICK FACTS 2018-2019 LEE♦- COLLEGE . QUICK. .FACTS . Fall 2018 Enrollment 8,234 4% LEE COLLEGE increase over --•-•-•--- Fall 2017 4,838 2,293 1,103 Baytown Dual Credit Huntsville Top 10 Degrees & Certificates 1,655 ■ 1. Business Management (Huntsville) ■ 2. Process Technology ■ 3. Instrumentation 1,155 1,107 ■ 4. CADD and Engineering Technology 879 863 ■ 5. General Studies ■ 6. Business Management 630 ■ 489 7. Welding Technology (Huntsville) 372 ■ 8. Culinary (Huntsville) 320 287 ■ 9. Nursing ■10. Horticulture (Huntsville) Total Associate Degrees & Certificates Awarded Last 5 Years: 11,675 t • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • • Ethnicity Age Breakdown Gender 43% 14% 18-24 37% 11% 25-29 43% 23% 13% under 18 30-39 tt 6% 54% 46% 1% 7% 60+ 40-49 African American Hispanic/Latino 3% ■ 50-59 Other White Notable Achievements, Initiatives and Programs • Achieving the Dream 2019 Leader College of Distinction • 2nd in the Nation for Value of Technical Degrees • 2019 American Association of Community Colleges Award of (Brookings Institution) Excellence Finalist for Faculty Innovation – Paul Allen • Top 50 Associate-Degree Producers in the Nation for • 2018 Association of Community College Trustees Regional Science Technologies/Technicians, Precision Production Equity Award Winner and National Finalist and Engineering Technologies, Engineering-Related Fields • 2018 American Association of Community Colleges Award of (Community College Week) Excellence Winner for Advancing Diversity • Lead Institution, Community College Petrochemical Initiative • 2018 American Association of Community Colleges Award of • Federal Hispanic-Serving Institution Excellence Finalist for College/Corporate Partnership • U.S. Department of Education Developing Hispanic-Serving • 2018 Bellwether Award Finalist for Instructional Programs & Institutions Program Title V Grant – $2.6 million Services recognizing Lee College’s Weekend College • U.S. -

Undergraduate Catalog 2011-2012
Undergraduate Catalog 2011-2012 VOLUME 38 PLEASE VISIT OUR WEB SITE AT: http://www.uhcl.edu This publication is available on the internet at: http://www.uhcl.edu/catalog or by request to the Office of Admissions UNIVERSITY OF HOUSTON-CLEAR LAKE 2700 Bay Area Boulevard Houston, Texas 77058-1098 Telephone: 281-283-2500 Important dates and Quick Reference Guide are available at: http://www.uhcl.edu/records DIRECTORY Office *Phone Academic Records S1109 283-2525 Admissions S1101 283-2500 Alumni Relations B1604 283-2021 Bookstore B1206 283-2180 Business, Dean B2239 283-3100 Academic Advising B2111 283-3110 Administration B2239 283-3100 Career Services S3109 283-2590 Cashier and Collections S1103 283-2170 Communications B2519 283-2015 Community Relations B1604 283-2021 Counseling Services S3103 283-2580 Dean of Students S1201 283-2567 Development B1604 283-2021 Distance and Off-Campus Education B1406 283-3031 Education, Dean B1237 283-3501 Academic Advising B1231 283-3615 Center for Educational Programs A190 283-3530 Center for Professional Development of Teachers B1231 283-3612 Teacher and Professional Certification B1231 283-3618 Health and Disability Services S1301 283-2626 Human Sciences and Humanities, Dean B1529 283-3300 Academic Affairs B1539 283-3400 Academic Advising B1539 283-3333 Administration and Finance B1617 283-3350 Intercultural and International Student Services S1203 283-2575 International Initiatives B1402 283-2531 Library B2402 283-3900 Office of Online Programs B1402 283-3056 Parking Permits B1636 283-2222 Police B1636 283-2222 Registrar S1109 283-2525 Science and Computer Engineering, Dean B3611 283-3703 Academic Affairs B3611 283-3711 Academic Advising B3611 283-3700 Student Assistance Center S1102 283-2722 Student Financial Aid S1105 283-2480 Student Information and Assistance (Bayou Bldg). -
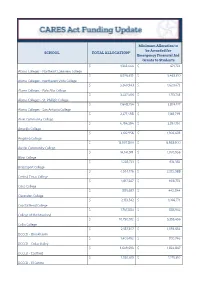
SCHOOL TOTAL ALLOCATION* Minimum Allocation to Be Awarded
Minimum Allocation to be Awarded for SCHOOL TOTAL ALLOCATION* Emergency Financial Aid Grants to Students $ 1,343,444 $ 671,722 Alamo Colleges - Northeast Lakeview College $ 6,926,619 $ 3,463,310 Alamo Colleges - Northwest Vista College $ 3,240,943 $ 1,620,472 Alamo Colleges - Palo Alto College $ 3,427,506 $ 1,713,753 Alamo Colleges - St. Phillip's College $ 7,648,254 $ 3,824,127 Alamo Colleges - San Antonio College $ 2,277,498 $ 1,138,749 Alvin Community College $ 4,794,394 $ 2,397,197 Amarillo College $ 2,612,956 $ 1,306,478 Angelina College $ 13,907,800 $ 6,953,900 Austin Community College $ 14,141,911 $ 7,070,956 Blinn College $ 1,228,723 $ 614,362 Brazosport College $ 4,544,176 $ 2,272,088 Central Texas College $ 1,817,547 $ 908,774 Cisco College $ 885,687 $ 442,844 Clarendon College $ 2,133,542 $ 1,066,771 Coastal Bend College $ 1,767,883 $ 883,942 College of the Mainland $ 10,790,912 $ 5,395,456 Collin College $ 2,187,307 $ 1,093,654 DCCCD - Brookhaven $ 1,401,492 $ 700,746 DCCCD - Cedar Valley $ 3,649,693 $ 1,824,847 DCCCD - Eastfield $ 2,550,619 $ 1,275,310 DCCCD - El Centro $ 2,902,459 $ 1,451,230 DCCCD - Mountain View $ 2,498,181 $ 1,249,091 DCCCD - North Lake $ 4,316,107 $ 2,158,054 DCCCD - $ 3,854,029 $ 1,927,015 Del Mar College $ 16,590,145 $ 8,295,073 El Paso Community College District $ 488,436 $ 244,218 Frank Phillips College $ 1,212,226 $ 606,113 Galveston College $ 2,157,844 $ 1,078,922 Grayson College $ 1,336,557 $ 668,279 Hill College $ 28,294,391 $ 14,147,196 Houston Community College System $ 1,454,607 $ 727,304 -

Report to the Community an INSTITUTIONAL YEAR in REVIEW for Display Until December 2019 Driving Diversity
Driving Diversity 2018 Report to the Community AN INSTITUTIONAL YEAR IN REVIEW For display until December 2019 Driving Diversity Table of Contents 3 Message from the President 4 Message from the Chairman 6 Driving Diversity 10 Our Service to Our Home 12 Our Mission & Purpose 29 Second Chances 22 Supporting Workforce 24 Pride in our people 26 Lee College Alliance 27 Lee College Foundation 2 2018 Report to the Community An Institutional Year In Review Lee College from the President A message from the President Lee College had an amazing year in 2018. We achieved record enrollment, earned a number of national awards, increased the number of students graduating with certificates and degrees, and continued our rise as a shining star within the regional communities we serve. The 2018 Report to the Community is full of inspiring stories, life changing experiences and many notable achievements. I know that you will enjoy reading our 2018 Institutional Year in Review. Lee College’s unduplicated credit enrollment in fall 2018 reached 8,234 students. The College has never seen an enrollment that high since its creation in 1934. In addition to our enrollments at the main campus in Baytown and the McNair Center, we have experienced robust enrollments in college courses taught to high school students in 17 different school systems in the Lee College Service Area. Also of note is our Second Chance Prison Education Program in Huntsville, where we have seen exceptional enrollment growth. The collaboration between Lee College and five school districts (Anahuac, Dayton, Hardin, Hulls-Daisetta and Liberty) at the Lee College Education Center in South Liberty County continues to flourish. -

Chapter 6 • the Community and Lee College
Chapter 6 • The Community and Lee College The Community & Lee College DISTANCE EDUCATION Flexible: The lab portion of the beginning and experienced exercise classes allow students to work out in the Wellness Center at times convenient to To provide quality education to service area residents, Lee College of- their school and work schedules. Students meet with their instructor fers educational services for students who find it difficult to attend classes periodically to review their progress. on the main campus. Instructors are selected from full-time faculty, outstanding area educators, and other professional specialists. Classes Individualized Instruction: Two means of individual instruction are pro- are held on the main campus and at off-site locations including the fol- vided. (1) Students work independently to study assigned materials, lowing: meeting with the instructor periodically. (2) Self-paced sections are available for those students taking computer-assisted developmental Lee College at Crosby math. Like a regular class, students meet in the computer classroom on a scheduled basis to receive individual instruction from faculty but are Students may enroll in credit and continuing education classes at this able to work at their own pace to meet the course objectives. Those up-to-date facility. A state-of-the-art cosmetology facility is available who have completed a sufficient amount of work yet not finished by the for students and patrons. For more information on this program, call end of the term, receive an in-progress grade (“R”) and enroll in the (281) 328-5757. Refer to the class schedules for current offerings. course again. -

College Signing
Class of 2018 College Signing Day May 4, 2018 STUDENT COLLEGE ATTENDING Coates, Ragan Texas A&M University Kennedy, Maddi Texas A&M University Pelata, Mya Texas A&M University Thomas, Skylar Texas A&M University Outley, Mykael Academy of Art San Francisco Holcomb, Keara US Air Force Berlier, Angel Angelo St. University Baird, Thomas Austin Community College Wright, Madison Belmont Abbey College Constantine, Cierra Blinn College Hall, Madison Blinn College Lamb, Kaci Blinn College Netherly, Paris Florida International University Boyette, Rachel Houston Baptist University Brooks, Matthew Jarvis Christian College Taylor, Dominique Lamar University Barnhill, Emilie-Grace Lee College Guzman, Josh Lee College Hill, Cade Lee College Landry, Chris Lee College Mendez, Dalton Lee College Moon, Nicole Lee College Hairell-Sweat, Taylor Lonestar College Patterson III, Cedric New Mexico University Cannon, Katrell Prairie View A&M University Stewart, Kordell Sam Houston State University Brooks, Kaleb San Jacinto College Celania, Brianna San Jacinto College Celania, Celeste San Jacinto College STUDENT COLLEGE ATTENDING Hampton, Albert San Jacinto College Phillips, Jarret San Jacinto College Sosa, Samantha San Jacinto College Torres, Ramiro San Jacinto College Delome, Miranda Stephen F. Austin State University Martinez, Victoria Stephen F. Austin State University Odell, Rebekah Stephen F. Austin State University Schneider, Matthew Stephen F. Austin State University Schreiber, Olivia Stephen F. Austin State University Guajardo, Danny Southern Nazarene