DENTAL
Care
Content
Dental Care
134 137 138
How must the professional proceed in order to obtain reimbursement for dental care?
Why is the professional/provider asking the client to pay for their service?
Reason 1 - The professional/provider refuses to collaborate with Health Canada to receive payment for the services or the professional is unfamiliar with Heath Canada’s reimbursement process.
140 141
Reason 2 - The client did not indicate their First Nations status to the professional/provider.
Reason 3 - Difference in cost between the amount reimbursed by Health Canada and the amount being billed by the professional/provider.
143 144 145
Reason 4 - Non-respect for the frequency limits in the client’s file (e.g. not enough time has passed between two treatments).
Reason 5 - The dental care being requested is excluded from the program.
Frequently Asked Questions
DENTAL CARE
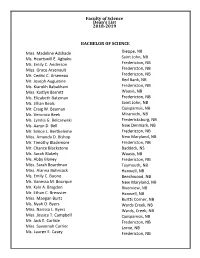
Since February 2013, preauthorisation for Health Canada’s dental care services is performed by
the National Dental Predetermination Centre located in Ottawa.
Health Canada’s Dental Care program covers care and services when these are not covered by Quebec’s health insurance plan. Client eligibility is described in the following table.
ELIGIBLE CLIENTELE
- RAMQ
- NIHB
- •
- The costs for cleaning, periodontal scaling
and the application of fluoride and sealants for children ages nine years or under
••
Children nine years of age or under (excludes: cleaning, periodontal scaling and fluoride)
•
•
First Nations members ten years and up (on- and off-reserve)
Provincial income security recipients
See the Provincial Health Care and Services section
Income security recipients on-reserve
The services covered by Health Canada are described in:
••
The Dental Benefits Guide (appended); The NIHB information booklet, pages 8 to 14.
Certain types of services provided by the Dental Care program must be preauthorised by Health Canada. All requests from professionals/providers are received and authorised by the National Dental Predetermination Centre in Ottawa.
Usually, in Quebec, the professionals/providers are quite familiar with how Health Canada operates. However, sometimes problems arise when attempting to access the care and services.
This section will enable you to better understand the request processing process for dental care and services. You will also find a list of commonly encountered problems as well as possible solutions in order to address these situations.
In this section, the term “professional/provider” includes dentists, dental care specialists (endodontists, periodontists, orthodontists, prosthodontists, etc.) and denturologists.
CONTENT - Dental Care
133
REGULAR DENTAL CARE REIMBURSEMENT PROCESS
HOW MUST THE PROFESSIONAL PROCEED IN ORDER TO OBTAIN REIMBURSEMENT FOR DENTAL CARE?
All the professionals/providers who wish to provide services to the First Nations and use the online billing system must be registered/connected to a national electronic system linking them directly to Health Canada.
Express Script Canada (ESC) is an organisation that uses an electronic system allowing the professionals/providers to bill Health Canada directly for the treatments provided.
ESC is also the organisation responsible for auditing the financial statements and the accuracy of the invoices submitted by the professionals/providers. It has the power to recover money when irregularities are found in the billing. ESC has no power related to
the authorisation of dental care and services. It is just the organisation responsible for
financial management. If the professional is not registered with ESC, they can contact the toll-free inquiry centre intended for providers (1-888-511-4666) to receive support for the registration steps.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
134
REGULAR REIMBURSEMENT PROCEDURES OF THE PROFESSIONALS/PROVIDERS
The professional/provider must seek predetermination for the majority of the dental care services before providing any care or treatment to the client.
See important note
Predeterminations must be performed by mail only. Once it is mailed, the professional/provider
will then obtain a predetermination number to be included on the invoice sent to ESC in order to receive reimbursement from Health Canada.
The professional must forward to the National Dental Predetermination Centre:
- •
- A Dent-29 form duly completed by the professional/provider;
See the appended form.
••
The x-rays; Any other diagnostic aid.
All the documentation must be transmitted to the following address:
National dental predetermination Centre
Non-Insured Health Benefits First Nations and Inuit Health Branch Health Canada Postal Locator 1902D 2nd floor, Jeanne Mance building 200, Eglantine Driveway Ottawa (Ontario) K1A 0K9
CONTENT - Dental Care
135
EXCEPTION FOR PREDETERMINATION BY MAIL
The only types of dental care that can be predetermined by telephone or fax are dentures.
National Dental Predetermination Centre Telephone: 1-855-618-6291 Fax: 1-855-618-6290
Any other predetermination requests for care and treatment must be sent by mail.
IMPORTANT NOTE
the predetermination performed by the professional:
Predetermination for dental care services is particularly important due to the fact that there are many exceptions and specific types of care that can be approved depending on certain conditions (position of the tooth in the mouth, treatment history, etc.).
See NIHB information booklet, pages 8 to 14.
It should be noted that if no predetermination is requested from the National Dental Predetermination Centre, the professional is at-risk of providing services to the patient that will not be eligible for the program and for which all of the costs must be covered by the patient. It is also possible that Health Canada’s reimbursement will be lower than what the professional/provider wishes to charge the client.
Note that, at all times, patients must be informed regarding what they will be required to pay before receiving their services. Then the patients can decide whether or not they wish to receive the service.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
136
PROBLEMS RELATED TO DENTAL CARE REIMBURSEMENT
WHY IS THE PROFESSIONAL/PROVIDER ASKING THE CLIENT TO PAY FOR THEIR SERVICE?
Usually, it is the dental care and services professional/provider who deals directly with Health Canada for predetermination and billing purposes. The client is therefore not required to pay with their own money.
However, certain circumstances can cause the professional/provider to ask your client to pay in order to access the health care and services that they need.
There are five possible reasons:
The professional/provider refuses to collaborate with Health Canada in order to receive payment for the services or the professional is unfamiliar with Health Canada’s reimbursement process.
Reason
Reason Reason
The client did not indicate their First Nations status to the professional/ provider.
There is a difference in cost between the amount reimbursed by Health Canada and the amount being billed by the professional/provider (overbilling).
Non-respect for the frequency limits in the client’s file (i.e. not enough time has passed between two treatments).
Reason Reason
The dental care being requested is excluded from the program.
CONTENT - Dental Care
137
The professional/provider refuses to collaborate with Health Canada to receive payment for the services or the professional is unfamiliar with Heath Canada’s reimbur- sement process.
Reason
SOLUTIONS
1. You can ask the professional/provider to contact the National Dental Predetermination Centre for more information on the billing system (ESC) and the process for obtaining reimbursement;
Health Canada’s National Dental Predetermination Centre: 1-855-618-6291.
2. You can help the client to find another professional/ provider who is willing to collaborate with Health Canada;
See the appended list of the professionals/providers by region.
3. Your client can accept to pay the invoice and then seek reimbursement from Health
Canada.
See important note
In this case, the client must forward by mail:
••
The professional/provider’s original invoice; A Dent-29 form duly completed by the professional.
See the appended form.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
138
All the documentation must be forwarded to the following address (a period of 30 days must be expected for reimbursement).
National dental predetermination Centre
Non-Insured Health Benefits First Nations and Inuit Health Branch Health Canada Postal Locator 1902D 2nd floor, Jeanne Mance building 200, Eglantine Driveway Ottawa (Ontario) K1A 0K9
IMPORTANT NOTE
The predetermination of the dental care by the client.
Ideally, the client must seek predetermination from Health Canada’s National Dental Predetermination Centre before their appointment in order to ensure that the services being requested are eligible for reimbursement.
If the client does not obtain predetermination, they are at-risk of receiving services that are not included in Health Canada’s Dental Benefits Guide and therefore ineligible for reimbursement. The client will be obligated to pay them completely.
CONTENT - Dental Care
139
The client did not indicate their First Nations status to the professional/provider.
Reason
SOLUTION
If the client has already paid the bill, the client can file the claim on their own in order to receive reimbursement. The client must send by mail:
See important note
••
The provider’s original invoice;
A Dent-29 form duly completed by the professional.
See the appended form.
All the documentation must be forwarded to the following address (a period of 30 days must be expected for the payment):
National dental predetermination Centre
Non-Insured Health Benefits First Nations and Inuit Health Branch Health Canada Postal Locator 1902D 2nd floor, Jeanne Mance building 200, Eglantine Driveway Ottawa (Ontario) K1A 0K9
IMPORTANT NOTE
The predetermination of the dental care by the client.
Ideally, the client must seek predetermination from Health Canada’s National Dental Predetermination Centre before their appointment in order to ensure that the services being requested are eligible for reimbursement.
If the client does not obtain predetermination, they are at-risk of receiving services that are not included in Health Canada’s Dental Benefits Guide and therefore ineligible for reimbursement. The client will be obligated to pay them completely.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
140
Difference in cost between the amount reimbursed by Health Canada and the amount being billed by the professional/provider.
Reason
As a general rule, the dental care professionals/providers set their prices while referring to the
fee schedule established by the Association des chirurgiens dentistes du Québec (ACDQ). In
parallel, Health Canada also provides its own fee schedule for reimbursements based on a percentage of the amounts reimbursed recorded in the fee schedule of the ACDQ.
No provider is obligated to apply the fee schedule proposed by Health Canada. This schedule
features Health Canada’s suggested rates and is based on an acceptable evaluation of the costs in Quebec. However, Health Canada does not reimburse rates higher than the amounts indicated in its fee schedule.
In most cases, the fee schedule does not cause any problems and the professionals/providers are satisfied with the compensation for the delivery of services to the First Nations clientele.
However, over the past few years, we have noticed that certain professionals are not respecting Health Canada’s rates and that an increasing number of clients are forced to cover a residual amount for their treatment.
For example: The dentist bills an amount of $30 for two x-rays (one for each side of the mouth) in the context of a routine examination. According to Health Canada’s fee schedule, an amount of $25.78 will be reimbursed to the provider. It is therefore possible that the client will be obligated to cover the difference of $4.22.
This overbilling can also apply to all the other services provided by the professional/provider (cleaning, fillings, root canal treatment, etc.). When adding up all of the amounts that could be charged to the client, the total amount could end up being considerable.
The professional/provider must inform the client of any differences in cost before providing the service to them. The client can then decide whether or not they wish to receive the service.
CONTENT - Dental Care
141
SOLUTIONS
1. You can help the client to find another professional/provider who is willing to respect
Health Canada’s reimbursement rate schedule;
See the appended list of professionals/providers.
2. The client can accept to cover the difference being billed by the professional. If you experience a problem related to overbilling in your region, you can contact the FNQLHSSC and ask to speak with the Health Care Liaison Agent.
We will ensure that follow-up with Health Canada is carried out. Other similar cases may have been identified in your region and by being informed of these types of cases, the FNQLHSSC will be able to take the necessary steps to correct the situation.
Health Care Liaison Agent (FNQLHSSC): 418-842-1540.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
142
Non-respect for the frequency limits in the client’s file (e.g. not enough time has passed between two treatments).
Reason
Some types of dental care or services are subjected to frequency limits before they can be approved again by Health Canada.
For example: An adult is entitled to one (1) set of dentures for each period of eight (8) years. If the client requests a new set of dentures before this period of time has passed, the request will automatically be denied.
However, if there is a medical condition justifying a new set of dentures, it may be possible to reach an agreement with the National Dental Predetermination Centre (1 855-618-6291) in order to evaluate the situation. If Health Canada continues to deny benefit coverage, the client can resort to the appeal process.
See the appended dental care appeal process and appeal letter.
SOLUTIONS
1. The client has the option to pay to immediately receive the service but will not be eligible for reimbursement from Health Canada;
2. The client can wait for the time limit to expire and then access the services freeof-charge;
3. For exceptional cases, the client can reach an agreement with the National Dental
Predetermination Centre to have the situation evaluated: 1-855-618-6291.
CONTENT - Dental Care
143
The dental care being requested is excluded from the program.
Reason
Some types of dental care constitute a program exclusion (examples: implants, whitening, etc.). Reimbursement for dental program exclusions is denied automatically and cannot be appealed.
See the dental program’s exclusions in the NIHB information booklet on page 12.
SOLUTIONS
1. The client has the option to pay to have access to the service but will not be eligible for reimbursement from Health Canada;
2. The professional/provider can be asked to consider alternative treatment and to seek predetermination for its coverage by Health Canada.
National Dental Predetermination Centre: 1 855 618-6291.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
144
Frequently Asked Questions
DENTAL CARE
HOW DOES DENTAL CODING FOR THE PROFESSIONALS/PROVIDERS WORK?
Health Canada’s National Dental Predetermination Centre as well as the professionals/providers use a wide range of codes that are connected to dental care services and the positions of the teeth in the mouth.
The following figure indicates the numbers corresponding to the teeth of adults and children.
- Adult
- Child
- 11
- 21
- 12
- 22
- 13
- 23
14
15
24
25
26
Top
51 61
Top
- 52
- 62
63
16
53
54
55
64
65
17 18
27 28
55...51 61...65
85...81 71...75
Bottom
18...11 21...28 48...41 31...38
48
47
38 37
85
84
75
74
- 83
- 73
- 82
- 72
46
45
36
35
81 71
Bottom
44
43
34
33
- 42
- 32
41 31
For example, the invoice or treatment plan from your provider could indicate the following:
- CODE
- TOOTH
NUMBER
- PRICE
- TREATMENT
33300 02142 23222
26
-
$676.71
$25.78
33300 : Root canal treatment on tooth #26. 02142 : Two basic x-rays for a routine examination.
- 23222 : A white composite filling on tooth #16.
- 16
- $134.42
Total : $836.91
CONTENT - Dental Care
145
WHAT IS HEALTH CANADA’S COVERAGE FOR ROOT CANAL TREATMENTS?
• As a general rule, this care is covered for all teeth except for the last molars (teeth
#17-27-47-37) and wisdom teeth (teeth #18-28-38-48);
Adult
- 11
- 21
- 12
- 22
- 13
- 23
14
15
16
24
25
26
Top
- 17
- 27
- 18
- 28
18...11 21...28
48...41 31...38
48
47
38 37
- 46
- 36
- 35
- 45
44
43
Bottom
34
33
- 42
- 32
41 31
• Root canal treatments on an adult’s anterior teeth can be performed without preauthorisation;
See important note
• Root canal treatments on the posterior teeth (last molars and wisdom teeth) must however always be preauthorised;
• If one of these posterior teeth is in need of root canal treatment and this tooth is essential to supporting a bridge or dentures or if it is the last remaining molar, the National Dental Predetermination Centre could make an exception and authorise root canal treatment for this tooth;
• Root canal treatment approval can be subjected to an analysis on a case by case basis and can also be influenced by other factors such as the client’s oral hygiene history.
IMPORTANT NOTE
Health Canada nonetheless suggests to dentists that they should seek predetermination for all root canal treatments since these types of treatments on the anterior teeth are subjected to auditing (recovery) if they do not meet the program’s criteria.
GPS • GUIDE TO PROCEDURES FOR ACCESSING HEALTH SERVICES
146
WHAT IS HEALTH CANADA’S COVERAGE FOR CROWNS?
WHAT IS A CROWN?
A crown can serve to cover a damaged portion of a tooth and protect it from additional damage. It can be needed in the following cases:
•••
Following root canal treatment; A large filling in a tooth; A broken tooth.