Effectiveness of Pfizer-Biontech and Moderna Vaccines in Preventing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Third Quarter 2020
March 31, 2020 Third Quarter 2020 Corporate update and financial results November 10, 2020 Forward-looking statements Various statements in this slide presentation concerning the future expectations of BioNTech, its plans and prospects, including the Company's views with respect to the potential for mRNA and other pipeline therapeutics; BioNTech's efforts to combat COVID-19; the collaborations between BioNTech and Pfizer and Fosun to develop a potential COVID-19 vaccine; our expectations regarding the potential characteristics of BNT162b2 in our continuing Phase 2/3 trial and/or in commercial use based on data observations to date; the expected timepoint for additional readouts on efficacy data of BNT162b2 in our Phase 2/3 trial; the nature of the clinical data for BNT162, BNT311 and our other product candidates, which is subject to ongoing peer review, regulatory review and market interpretation; the timing for submission of data for, or receipt of, any potential approval or Emergency Use Authorization with respect to our BNT162 program; the timing for submission of BNT162 manufacturing data to the FDA; the ability of BioNTech to supply the quantities of BNT162 to support clinical development and, if approved, market demand, including our production estimates for 2020 and 2021 and orders received to-date; the planned next steps in BioNTech's pipeline programs and specifically including, but not limited to, statements regarding plans to initiate clinical trials of BioNTech's product candidates and expectations for data announcements with -

Investor Presentation
Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Q1 2021 Results Investor presentation 1 Investor Relations │ Q1 2021 Results Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Disclaimer This presentation contains forward-looking statements within the meaning of the United States Private Securities Litigation Reform Act of 1995, that can generally be identified by words such as “potential,” “expected,” “will,” “planned,” “pipeline,” “outlook,” or similar expressions, or by express or implied discussions regarding potential new products, potential new indications for existing products, potential product launches, or regarding potential future revenues from any such products; or regarding the impact of the COVID-19 pandemic on certain therapeutic areas including dermatology, ophthalmology, our breast cancer portfolio, some newly launched brands and the Sandoz retail and anti-infectives business, and on drug development operations; or regarding potential future, pending or announced transactions; regarding potential future sales or earnings of the Group or any of its divisions; or by discussions of strategy, plans, expectations or intentions; or regarding the Group’s liquidity or cash flow positions and its ability to meet its ongoing financial obligations and operational needs; or regarding our collaboration with Molecular Partners to develop, manufacture and commercialize potential medicines for the prevention and treatment of COVID- 19 and our joining of the industry-wide efforts to meet global demand for COVID-19 vaccines and therapeutics by leveraging our manufacturing capacity and capabilities to support the production of the Pfizer-BioNTech vaccine and to manufacture the mRNA and bulk drug product for the vaccine candidate CVnCoV from CureVac. -

COVID-19 Mrna Pfizer- Biontech Vaccine Analysis Print
COVID-19 mRNA Pfizer- BioNTech Vaccine Analysis Print All UK spontaneous reports received between 9/12/20 and 22/09/21 for mRNA Pfizer/BioNTech vaccine. A report of a suspected ADR to the Yellow Card scheme does not necessarily mean that it was caused by the vaccine, only that the reporter has a suspicion it may have. Underlying or previously undiagnosed illness unrelated to vaccination can also be factors in such reports. The relative number and nature of reports should therefore not be used to compare the safety of the different vaccines. All reports are kept under continual review in order to identify possible new risks. Report Run Date: 24-Sep-2021, Page 1 Case Series Drug Analysis Print Name: COVID-19 mRNA Pfizer- BioNTech vaccine analysis print Report Run Date: 24-Sep-2021 Data Lock Date: 22-Sep-2021 18:30:09 MedDRA Version: MedDRA 24.0 Reaction Name Total Fatal Blood disorders Anaemia deficiencies Anaemia folate deficiency 1 0 Anaemia vitamin B12 deficiency 2 0 Deficiency anaemia 1 0 Iron deficiency anaemia 6 0 Anaemias NEC Anaemia 97 0 Anaemia macrocytic 1 0 Anaemia megaloblastic 1 0 Autoimmune anaemia 2 0 Blood loss anaemia 1 0 Microcytic anaemia 1 0 Anaemias haemolytic NEC Coombs negative haemolytic anaemia 1 0 Haemolytic anaemia 6 0 Anaemias haemolytic immune Autoimmune haemolytic anaemia 9 0 Anaemias haemolytic mechanical factor Microangiopathic haemolytic anaemia 1 0 Bleeding tendencies Haemorrhagic diathesis 1 0 Increased tendency to bruise 35 0 Spontaneous haematoma 2 0 Coagulation factor deficiencies Acquired haemophilia -

Statements Contained in This Release As the Result of New Information Or Future Events Or Developments
Pfizer and BioNTech Provide Update on Booster Program in Light of the Delta-Variant NEW YORK and MAINZ, GERMANY, July 8, 2021 — As part of Pfizer’s and BioNTech’s continued efforts to stay ahead of the virus causing COVID-19 and circulating mutations, the companies are providing an update on their comprehensive booster strategy. Pfizer and BioNTech have seen encouraging data in the ongoing booster trial of a third dose of the current BNT162b2 vaccine. Initial data from the study demonstrate that a booster dose given 6 months after the second dose has a consistent tolerability profile while eliciting high neutralization titers against the wild type and the Beta variant, which are 5 to 10 times higher than after two primary doses. The companies expect to publish more definitive data soon as well as in a peer-reviewed journal and plan to submit the data to the FDA, EMA and other regulatory authorities in the coming weeks. In addition, data from a recent Nature paper demonstrate that immune sera obtained shortly after dose 2 of the primary two dose series of BNT162b2 have strong neutralization titers against the Delta variant (B.1.617.2 lineage) in laboratory tests. The companies anticipate that a third dose will boost those antibody titers even higher, similar to how the third dose performs for the Beta variant (B.1.351). Pfizer and BioNTech are conducting preclinical and clinical tests to confirm this hypothesis. While Pfizer and BioNTech believe a third dose of BNT162b2 has the potential to preserve the highest levels of protective efficacy against all currently known variants including Delta, the companies are remaining vigilant and are developing an updated version of the Pfizer-BioNTech COVID-19 vaccine that targets the full spike protein of the Delta variant. -
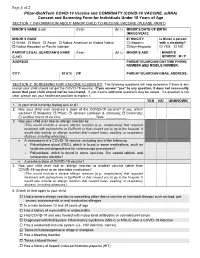
Pfizer-Biontech COVID-19 Vaccine Consent and Screening Form For
Page 1 of 2 Pfizer-BioNTech COVID-19 Vaccine and COMIRNATY (COVID-19 VACCINE, mRNA) Consent and Screening Form for Individuals Under 18 Years of Age SECTION 1: INFORMATION ABOUT MINOR CHILD TO RECEIVE VACCINE (PLEASE PRINT) MINOR’S NAME (Last) (First) (M.I.) MINOR’S DATE OF BIRTH (MM/DD/YEAR): MINOR’S RACE ETHNICITY Is Minor a person White Black Asian Native American or Alaska Native Hispanic with a disability? Native Hawaiian or Pacific Islander Non-Hispanic YES NO PARENT/LEGAL GUARDIAN’S NAME (First) (M.I.) MINOR’S AGE: MINOR’S (Last) GENDER: M / F ADDRESS PARENT/GUARDIAN DAYTIME PHONE NUMBER AND MOBILE NUMBER: CITY STATE ZIP PARENT/GUARDIAN EMAIL ADDRESS: SECTION 2: SCREENING FOR VACCINE ELIGIBILITY The following questions will help determine if there is any reason your child should not get the COVID-19 vaccine. If you answer “yes” to any question, it does not necessarily mean that your child should not be vaccinated. It just means additional questions may be asked. If a question is not clear, please ask your healthcare provider to explain it. YES NO UNKNOWN 1. Is your child currently feeling sick or ill? 2. Has your child ever received a dose of the COVID-19 vaccine? If yes, which vaccine? Moderna; Pfizer; Janssen (Johnson & Johnson); Comirnaty; another brand of vaccine: _________________ Date: ___________ 3. Has your child ever had an allergic reaction to: (This would include a severe allergic reaction [e.g., anaphylaxis] that required treatment with epinephrine or EpiPen® or that caused you to go to the hospital. It would also include an allergic reaction that caused hives, swelling, or respiratory distress, including wheezing.) A component of a COVID-19 vaccine, including any of the following: o Polyethylene glycol (PEG), which is found in some medications, such as laxatives and preparations for colonoscopy procedures? o Polysorbate, which is found in some vaccines, film coated tablets, and intravenous steroids? A previous dose of COVID-19 vaccine? 4. -

Biontech Publishes Data on Novel Mrna Vaccine Approach to Treat Autoimmune Diseases in Science
BioNTech Publishes Data on Novel mRNA Vaccine Approach to Treat Autoimmune Diseases in Science January 7, 2021 Collaborative study of BioNTech with TRON and the University Medical Center and Research Center for Immunotherapy at Johannes Gutenberg University of Mainz introduces novel non-inflammatory mRNA vaccine encoding disease-related autoantigens that suppressed disease activity in several complex mouse models of multiple sclerosis Approach addresses key pitfalls in the treatment of autoimmune diseases such as the induction of systemic immune suppression Approach can easily be tailored to individual disease-causing antigens of patients and confers bystander tolerance to address highly complex, polyclonal and rare autoimmune disease types Represents the first application of BioNTech’s mRNA technology for the purpose of antigen-specific immune-modulation of autoimmune diseases, which further expands BioNTech’s diversified immunology pipeline into another category of disease relevant targets MAINZ, GERMANY, January 7, 2021 (GLOBE NEWSWIRE) —BioNTech SE (Nasdaq: BNTX, “BioNTech” or “the Company”) announced today the publication of preclinical data on its novel mRNA vaccine approach against autoimmune diseases in the peer-reviewed journal Science. The publication titled “A non-inflammatory mRNA vaccine for treatment of experimental autoimmune encephalomyelitis” summarizes the findings on the disease-suppressing effects of a non-inflammatory, nucleoside-modified mRNA vaccine in several clinically relevant mouse models of multiple sclerosis (MS). Autoimmune diseases like MS represent conditions in which the immune system malfunctions and attacks healthy tissue or cells of the body. In MS, the inflammation causes the destruction of the protective myelin sheath that covers the nerve fibers. This damage disrupts the ability to transmit signals between nerve cells and the target tissue resulting in a range of neurological, sensory and motor symptoms that may differ greatly between individuals. -

Update on Our COVID-19 Vaccine Development Program with Bnt162b2
Update on our COVID-19 vaccine development program with BNT162b2 December 2, 2020 This slide presentation includes forward-looking statements Forward-Looking Statements Various statements in this slide presentation concerning the future expectations of BioNTech, its plans and prospects, including the Company’s views with respect to its efforts to combat COVID-19; the collaboration between BioNTech and Pfizer to develop a potential COVID-19 vaccine; its expectations regarding the potential characteristics of BNT162b2 in its Phase 2/3 trial and/or in commercial use based on data observations to date; the expected timepoint for additional readouts on efficacy data of BNT162b2 in our Phase 2/3 trial; the nature of the clinical data, which is subject to ongoing peer review, regulatory review and market interpretation; the timing for submission of data for, or receipt of, any marketing approval or additional Emergency Use Authorization; the timing for submission of manufacturing data to the FDA; its contemplated shipping and storage plan, including its estimated product shelflife at various temperatures; and the ability of BioNTech to manufacture and supply the quantities of BNT162 to support clinical development and, if approved, market demand, including our production estimates for 2020 and 2021, are forward-looking statements reflecting the current beliefs and expectations of management made pursuant to the safe harbor provisions of the Private Securities Litigation Reform Act of 1995, as amended. Words such as "expects," "plans," "potential," "target," "continue" and variations of these words or similar expressions are intended to identify forward-looking statements. Such statements are based on the current beliefs and assumptions of the management team of BioNTech and on the information currently available to the management team of BioNTech, and are subject to change. -

DARZALEX® (Daratumumab)
Year End Results Period Ended December 31, 2019 Forward Looking Statement This presentation contains forward looking statements. The words “believe”, “expect”, “anticipate”, “intend” and “plan” and similar expressions identify forward looking statements. All statements other than statements of historical facts included in this presentation, including, without limitation, those regarding our financial position, business strategy, plans and objectives of management for future operations (including development plans and objectives relating to our products), are forward looking statements. Such forward looking statements involve known and unknown risks, uncertainties and other factors which may cause our actual results, performance or achievements to be materially different from any future results, performance or achievements expressed or implied by such forward looking statements. Such forward looking statements are based on numerous assumptions regarding our present and future business strategies and the environment in which we will operate in the future. The important factors that could cause our actual results, performance or achievements to differ materially from those in the forward looking statements include, among others, risks associated with product discovery and development, uncertainties related to the outcome of clinical trials, slower than expected rates of patient recruitment, unforeseen safety issues resulting from the administration of our products in patients, uncertainties related to product manufacturing, the lack of market acceptance of our products, our inability to manage growth, the competitive environment in relation to our business area and markets, our inability to attract and retain suitably qualified personnel, the unenforceability or lack of protection of our patents and proprietary rights, our relationships with affiliated entities, changes and developments in technology which may render our products obsolete, and other factors. -

Comirnaty, INN-COVID-19 Mrna Vaccine (Nucleoside-Modified)
19 February 2021 EMA/707383/2020 Corr.1*1 Committee for Medicinal Products for Human Use (CHMP) Assessment report Comirnaty Common name: COVID-19 mRNA vaccine (nucleoside-modified) Procedure No. EMEA/H/C/005735/0000 Note Assessment report as adopted by the CHMP with all information of a commercially confidential nature deleted. 1 * Correction dated 19 February 2021 to clarify ERA statement Official address Domenico Scarlattilaan 6 ● 1083 HS Amsterdam ● The Netherlands Address for visits and deliveries Refer to www.ema.europa.eu/how-to-find-us An agency of the European Union Send us a question Go to www.ema.europa.eu/contact Telephone +31 (0)88 781 6000 © European Medicines Agency, 2021. Reproduction is authorised provided the source is acknowledged. Table of contents 1. Background information on the procedure .............................................. 8 1.1. Submission of the dossier ...................................................................................... 8 1.2. Steps taken for the assessment of the product ......................................................... 9 2. Scientific discussion .............................................................................. 11 2.1. Problem statement ............................................................................................. 11 2.1.1. Disease or condition ......................................................................................... 11 2.1.2. Epidemiology and risk factors ........................................................................... -

Pfizer-Biontech COVID-19 Vaccine Bnt162b2
DRAFT Prepared by the SAGE Working Group on COVID-19 Vaccines 22 December 2020 mRNA vaccines against COVID-19: Pfizer-BioNTech COVID-19 vaccine BNT162b2 Prepared by the Strategic Advisory Group of Experts (SAGE) on Immunization Working Group on COVID-19 vaccines 22 December 2020 © World Health Organization 2020. All rights reserved. This is a draft. The content of this document is not final, and the text may be subject to revisions before publication. The document may not be reviewed, abstracted, quoted, reproduced, transmitted, distributed, translated or adapted, in part or in whole, in any form or by any means without the permission of the World Health Organization. WHO reference number: WHO/2019-nCoV/vaccines/SAGE_evaluation/BNT162b2/2020.1 1 Background document for the Extraordinary meeting of the Strategic Advisory Group of Experts on Immunization (SAGE) - 5 January 2021 DRAFT Prepared by the SAGE Working Group on COVID-19 Vaccines 22 December 2020 Contents: General considerations on mRNA vaccines ............................................................................................................ 3 COVID-19 vaccine BNT162b2 (Pfizer-BioNTech) vaccine characteristics ................................................................ 3 Development process, contents, formulation ........................................................................................................ 3 Pre-clinical Studies ................................................................................................................................................. -

FDA Briefing Document: Pfizer-Biontech COVID-19 Vaccine
Vaccines and Related Biological Products Advisory Committee Meeting December 10, 2020 FDA Briefing Document Pfizer-BioNTech COVID-19 Vaccine Sponsor: Pfizer and BioNTech Table of Contents List of Tables ............................................................................................................................. 3 List of Figures ............................................................................................................................ 4 Glossary..................................................................................................................................... 5 1. Executive Summary ............................................................................................................... 6 2. Background ............................................................................................................................ 7 2.1. SARS-CoV-2 Pandemic ................................................................................................ 7 2.2. EUA Request for the Pfizer and BioNTech COVID-19 Vaccine BNT162b2 .................... 8 2.3. U.S. Requirements to Support Issuance of an EUA for a Biological Product ........................................................................................................................... 8 2.4. Applicable Guidance for Industry ................................................................................... 9 2.5. Safety and Effectiveness Information Needed to Support an EUA ................................. 9 2.6. Continuation -

Pfizer-Biontech COVID-19 Vaccine EUA Fact Sheet for Recipients And
FACT SHEET FOR RECIPIENTS AND CAREGIVERS EMERGENCY USE AUTHORIZATION (EUA) OF THE PFIZER-BIONTECH COVID-19 VACCINE TO PREVENT CORONAVIRUS DISEASE 2019 (COVID-19) IN INDIVIDUALS 12 YEARS OF AGE AND OLDER You are being offered the Pfizer-BioNTech COVID-19 Vaccine to prevent Coronavirus Disease 2019 (COVID-19) caused by SARS-CoV-2. This Fact Sheet contains information to help you understand the risks and benefits of the Pfizer-BioNTech COVID-19 Vaccine, which you may receive because there is currently a pandemic of COVID-19. The Pfizer-BioNTech COVID-19 Vaccine is a vaccine and may prevent you from getting COVID-19. There is no U.S. Food and Drug Administration (FDA) approved vaccine to prevent COVID-19. Read this Fact Sheet for information about the Pfizer-BioNTech COVID-19 Vaccine. Talk to the vaccination provider if you have questions. It is your choice to receive the Pfizer-BioNTech COVID-19 Vaccine. The Pfizer-BioNTech COVID-19 Vaccine is administered as a 2-dose series, 3 weeks apart, into the muscle. The Pfizer-BioNTech COVID-19 Vaccine may not protect everyone. This Fact Sheet may have been updated. For the most recent Fact Sheet, please see www.cvdvaccine.com. WHAT YOU NEED TO KNOW BEFORE YOU GET THIS VACCINE WHAT IS COVID-19? COVID-19 disease is caused by a coronavirus called SARS-CoV-2. This type of coronavirus has not been seen before. You can get COVID-19 through contact with another person who has the virus. It is predominantly a respiratory illness that can affect other organs.