The Relationship of Dietary Pattern and Genetic Risk Score with the Incidence of Dyslipidemia: 14-Year Follow-Up Cohort Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Interplay Between Angiopoietin-Like Proteins and Adipose Tissue: Another Piece of the Relationship Between Adiposopathy and Cardiometabolic Diseases?
International Journal of Molecular Sciences Review The Interplay between Angiopoietin-Like Proteins and Adipose Tissue: Another Piece of the Relationship between Adiposopathy and Cardiometabolic Diseases? Simone Bini *,† , Laura D’Erasmo *,†, Alessia Di Costanzo, Ilenia Minicocci , Valeria Pecce and Marcello Arca Department of Translational and Precision Medicine, Sapienza University of Rome, Viale del Policlinico 155, 00185 Rome, Italy; [email protected] (A.D.C.); [email protected] (I.M.); [email protected] (V.P.); [email protected] (M.A.) * Correspondence: [email protected] (S.B.); [email protected] (L.D.) † These authors contributed equally to this work. Abstract: Angiopoietin-like proteins, namely ANGPTL3-4-8, are known as regulators of lipid metabolism. However, recent evidence points towards their involvement in the regulation of adipose tissue function. Alteration of adipose tissue functions (also called adiposopathy) is considered the main inducer of metabolic syndrome (MS) and its related complications. In this review, we intended to analyze available evidence derived from experimental and human investigations highlighting the contribution of ANGPTLs in the regulation of adipocyte metabolism, as well as their potential role in common cardiometabolic alterations associated with adiposopathy. We finally propose a model of ANGPTLs-based adipose tissue dysfunction, possibly linking abnormalities in the angiopoietins to the induction of adiposopathy and its related disorders. Keywords: adipose tissue; adiposopathy; brown adipose tissue; ANGPTL3; ANGPTL4; ANGPTL8 Citation: Bini, S.; D’Erasmo, L.; Di Costanzo, A.; Minicocci, I.; Pecce, V.; Arca, M. The Interplay between 1. Introduction Angiopoietin-Like Proteins and Adipose tissue (AT) is an important metabolic organ and accounts for up to 25% of Adipose Tissue: Another Piece of the healthy individuals’ weight. -
What Are Soybeans?
candy, cakes, cheeses, peanut butter, animal feeds, candles, paint, body lotions, biodiesel, furniture soybeans USES: What are soybeans? Soybeans are small round seeds, each with a tiny hilum (small brown spot). They are made up of three basic parts. Each soybean has a seed coat (outside cover that protects the seed), VOCABULARY cotyledon (the first leaf or pair of leaves within the embryo that stores food), and the embryo (part of a seed that develops into Cultivar: a variety of plant that has been created or a new plant, including the stem, leaves and roots). Soybeans, selected intentionally and maintained through cultivation. like most legumes, perform nitrogen fixation. Modern soybean Embryo: part of a seed that develops into a new plant, cultivars generally reach a height of around 1 m (3.3 ft), and including the stem, leaves and roots. take 80–120 days from sowing to harvesting. Exports: products or items that the U.S. sells and sends to other countries. Exports include raw products like whole soybeans or processed products like soybean oil or Leaflets soybean meal. Fertilizer: any substance used to fertilize the soil, especially a commercial or chemical manure. Hilum: the scar on a seed marking the point of attachment to its seed vessel (the brown spot). Leaflets: sub-part of leaf blade. All but the first node of soybean plants produce leaves with three leaflets. Legume: plants that perform nitrogen fixation and whose fruit is a seed pod. Beans, peas, clover and alfalfa are all legumes. Nitrogen Fixation: the conversion of atmospheric nitrogen Leaf into a nitrogen compound by certain bacteria, such as Stem rhizobium in the root nodules of legumes. -

Laboratory Mouse Models for the Human Genome-Wide Associations
Laboratory Mouse Models for the Human Genome-Wide Associations The Harvard community has made this article openly available. Please share how this access benefits you. Your story matters Citation Kitsios, Georgios D., Navdeep Tangri, Peter J. Castaldi, and John P. A. Ioannidis. 2010. Laboratory mouse models for the human genome-wide associations. PLoS ONE 5(11): e13782. Published Version doi:10.1371/journal.pone.0013782 Citable link http://nrs.harvard.edu/urn-3:HUL.InstRepos:8592157 Terms of Use This article was downloaded from Harvard University’s DASH repository, and is made available under the terms and conditions applicable to Other Posted Material, as set forth at http:// nrs.harvard.edu/urn-3:HUL.InstRepos:dash.current.terms-of- use#LAA Laboratory Mouse Models for the Human Genome-Wide Associations Georgios D. Kitsios1,4, Navdeep Tangri1,6, Peter J. Castaldi1,2,4,5, John P. A. Ioannidis1,2,3,4,5,7,8* 1 Institute for Clinical Research and Health Policy Studies, Tufts Medical Center, Boston, Massachusetts, United States of America, 2 Tufts University School of Medicine, Boston, Massachusetts, United States of America, 3 Department of Hygiene and Epidemiology, University of Ioannina School of Medicine and Biomedical Research Institute, Foundation for Research and Technology-Hellas, Ioannina, Greece, 4 Tufts Clinical and Translational Science Institute, Tufts Medical Center, Boston, Massachusetts, United States of America, 5 Department of Medicine, Center for Genetic Epidemiology and Modeling, Tufts Medical Center, Tufts University -

Soy Products As Healthy and Functional Foods
Middle-East Journal of Scientific Research 7 (1): 71-80, 2011 ISSN 1990-9233 © IDOSI Publications, 2011 Soy Products as Healthy and Functional Foods Hossein Jooyandeh Department of Food Science and Technology, Ramin Agricultural and Natural Resources University, Mollasani, Khuzestan, Iran Abstract: Over the recent decades, researchers have documented the health benefits of soy protein, especially for those who take soy protein daily. Soy products offer a considerable appeal for a growing segment of consumers with certain dietary and health concerns. It is quite evident that soy products do reduce the risks of developing various age-related chronic diseases and epidemiologic data strongly suggest that populations that regularly consume soy products have reduced incidence and prevalence of the aforementioned age-related conditions and diseases than populations that eat very little soy. The subject of what specific components is responsible for the plethora of reported health benefits of soybean remains a strong controversial issue, as the scientific community continues to understand what component(s) in soy is /are responsible for its health benefits. Soy constituents’ benefits mostly relate to the reduction of cholesterol levels and menopause symptoms and the reduction of the risk for several chronic diseases such as cancer, heart disease and osteoporosis. A variety of soy products are available on the market with different flavors and textures and a low-fat, nutritionally balanced diet can be developed from them. This article summarized the beneficial health, nutritional and functional properties of the soy ingredients and intends to illustrate the most current knowledge with a consciousness to motivate further research to optimize their favorable effects. -

Genetic and Genomic Analysis of Hyperlipidemia, Obesity and Diabetes Using (C57BL/6J × TALLYHO/Jngj) F2 Mice
University of Tennessee, Knoxville TRACE: Tennessee Research and Creative Exchange Nutrition Publications and Other Works Nutrition 12-19-2010 Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P. Stewart Marshall University Hyoung Y. Kim University of Tennessee - Knoxville, [email protected] Arnold M. Saxton University of Tennessee - Knoxville, [email protected] Jung H. Kim Marshall University Follow this and additional works at: https://trace.tennessee.edu/utk_nutrpubs Part of the Animal Sciences Commons, and the Nutrition Commons Recommended Citation BMC Genomics 2010, 11:713 doi:10.1186/1471-2164-11-713 This Article is brought to you for free and open access by the Nutrition at TRACE: Tennessee Research and Creative Exchange. It has been accepted for inclusion in Nutrition Publications and Other Works by an authorized administrator of TRACE: Tennessee Research and Creative Exchange. For more information, please contact [email protected]. Stewart et al. BMC Genomics 2010, 11:713 http://www.biomedcentral.com/1471-2164/11/713 RESEARCH ARTICLE Open Access Genetic and genomic analysis of hyperlipidemia, obesity and diabetes using (C57BL/6J × TALLYHO/JngJ) F2 mice Taryn P Stewart1, Hyoung Yon Kim2, Arnold M Saxton3, Jung Han Kim1* Abstract Background: Type 2 diabetes (T2D) is the most common form of diabetes in humans and is closely associated with dyslipidemia and obesity that magnifies the mortality and morbidity related to T2D. The genetic contribution to human T2D and related metabolic disorders is evident, and mostly follows polygenic inheritance. The TALLYHO/ JngJ (TH) mice are a polygenic model for T2D characterized by obesity, hyperinsulinemia, impaired glucose uptake and tolerance, hyperlipidemia, and hyperglycemia. -

Food System and Culture of Eating in India Impact Factor: 5.2 IJAR 2019; 5(3): 87-89 Received: 06-01-2019 Dr
International Journal of Applied Research 2019; 5(3): 87-89 ISSN Print: 2394-7500 ISSN Online: 2394-5869 Food system and culture of eating in India Impact Factor: 5.2 IJAR 2019; 5(3): 87-89 www.allresearchjournal.com Received: 06-01-2019 Dr. Durgesh Kumar Singh Accepted: 10-02-2019 Abstract Dr. Durgesh Kumar Singh India has one of the oldest civilizations in the world with a rich cultural heritage. In the sacred book of Principal, Swatantra Girls the Hindu called ‘Bhagavad Geeta’, foods are classified into three categories based on property, Degree College, Lucknow sanctity and quality – Sattvika, Raajasika and Taamasika. Sattvika food, which denotes food for University Lucknow, Uttar prosperity, longevity, intelligence, strength, health and happiness includes fruits, vegetables, legums, Pradesh, India cereals and sweets. Raajasika food, which signifies activity, passion and restlessness includes hot, sour, spicy and salty foods. Taamasika food is intoxicating and unhealthy. Keywords: health, food, diet, vegetarian, non- vegetarian, regional foods 1. Introduction Hindus are traditionally vegetarian but many non-Brahmins are non- vegetarians. Brahmin Hindu’s do not eat garlic, onion and intoxicants. Ethnic Indian foods have social importance for celebrations particularly during festivals and social occasions. The Indian food is spicy and salt is added directly by cooking seasoning such as soy-sauce and mono sodium glutamate are never used. The Dietary culture of India is a fusion of the Hindu-Aryan culture and the Tibetan–Mangolian culture influence by the ancient Chinese cuisines with modifications based on ethnic preference and sensory likings over a period of time. Use of fingers to grasp food items for feeding remains a traditional features of Hindu, Buddhist, and Muslim dietary cultures in India. -

China's Meat and Egg Production and Soybean Meal Demand for Feed: an Elasticity Analysis and Long-Term Projections
International Food and Agribusiness Management Review Volume 15, Issue 3, 2012 China's Meat and Egg Production and Soybean Meal Demand for Feed: An Elasticity Analysis and Long-Term Projections Tadayoshi Masudaa and Peter D. Goldsmithb aSenior Research Analyst, Research Institute for Humanity and Nature 457-4 Kamigamo Motoyama, Kita-ku, Kyoto 603-8047, Japan bAssociate Professor, Department of Agricultural and Consumer Economics, University of Illinois at Urbana, Champaign 1301 West Gregory Drive, Urbana, Illinois, 61801, USA Abstract China is a large meat and egg producer and correspondingly a large soybean meal consumer. Dual forces affect the derived demand for soybeans; rising livestock production to meet consum- er demand for protein and the shift to commercial feed by the livestock industry. We employ a unique elasticity approach to estimate these dual forces on soybean meal demand over the next 20 years. We then discuss the implications of these forecasts with respect to the modernization of China’s feed industry, land use changes in South America, and the need for yield research to reduce pressure on increasingly scarce land resources. Keywords: meat production; soybean meal; feed demand; elasticity; forecasting; land use Corresponding author: Tel: +217-333-5131 Email: P.D. Goldsmith: [email protected] +The IFAMR is a non-profit publication. The additional support provided from this issue advertisers, Novus International and GlobalGap help keep us open access and dedicated to serving management, scholars, and policy makers worldwide. 35 2012 International Food and Agribusiness Management Association (IFAMA). All rights reserved Madusa and Goldsmith / International Food and Agribusiness Management Review / Volume 15, Issue 3, 2012 Introduction Background The “livestock revolution” (Delgado et al. -

Winter Menu } February Fruit & Veg/ 1/2 Cup Total Milk 6Oz Cup
tm local & organic food for kids december Protein =2oz total january Grain>2oz winter menu } february Fruit & Veg/ 1/2 cup total Milk 6oz cup monday tuesday wednesday thursday friday Dec 31, Jan 28 January 1, 29 January 2, 30 January 3, 31 January 4 Roast Turkey w/ Gravy Three Cheese Baked Chicken Nuggets Beefy Sloppy Joe Three Bean Chili Lasagna Veggie “Chicken” Tenders Veggie Sloppy Joe Tofurkey Fresh Cucumbers Steamed Carrots Mixed Veggies Whipped Potatoes Fresh Broccoli Fruit Salad Fresh Pineapple Fresh Bananas Appleberry Sauce Pear Slices Elbow Pasta Whole Grain Bread Whole Grain Bread Whole Grain Bun January 7 January 8 January 9 January 10 January 11 Orange Chicken Farfalle w/ Tomato Beef Kabab Bites Creamy Three Cheese Orange Vegetarian Chicken Cream Sauce Falafel Mac n’ Cheese Pizza w/ Yogurt Dip Asian Veggies Steamed Carrots Sweet Local Peas Fresh Broccoli Honeydew Melon Fresh Cucumbers Fresh Pineapple Apple Slices Orange Slices Fruit Salad Brown Rice Whole Grain Pita January 14 January 15 January 16 January 17 January 18 Turkey Pot Pie Juicy Beef Burger Cheesy Quesadillas Cheesey Ravioli Sweet Apple Chicken Curry Veggie Pot Pie Veggie Burger w/ Sour Cream w/ Marinara Vegetarian Chicken Local Green Beans Fresh Steamed Broccoli Butternut Squash Sweet Local Peas Cauliflower & Carrots Orange Slices Appleberry Sauce Fresh Pineapple Fresh Melon Fruit Salad Fresh Baked Biscuit Whole Grain Bun Naan Bread January 21 January 22 January 23 January 24 January 25 Pasta w/ Alfredo Chicken w/ Plum Sauce Swedish Meatballs Fish Tenders Adobo -
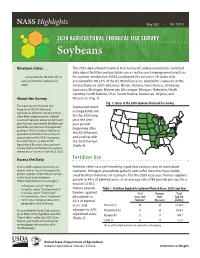
Soybeans USE
NASS Highlights May 2021 • No. 2021-1 AGRICULTURAL2020 AGRICULTURAL CHEMICAL USE SURVEY CHEMICALSoybeans USE Nineteen states . The 2020 Agricultural Chemical Use Survey of soybean producers collected data about fertilizer and pesticide use as well as pest management practices . accounted for 96.32% of U.S. for soybean production. NASS conducted the survey in 19 states that acres planted to soybeans AGRICULTURAL in accounted for 96.32% of the 83.08 million acres planted to soybeans in the 2020. United States in 2020: Arkansas, Illinois, Indiana, Iowa, Kansas, Kentucky, CHEMICALLouisiana, Michigan, USE Minnesota, Mississippi, Missouri, Nebraska, North Carolina, North Dakota, Ohio, South Dakota, Tennessee, Virginia, and About the Survey Wisconsin. (Fig. 1) Fig. 1. States in the 2020 Soybean Chemical Use Survey The Agricultural Chemical Use Soybean planted Program of USDA’s National Agricultural Statistics Service (NASS) acreage totals are is the federal government’s official for the 2020 crop source of statistics about on-farm and year, the one- post-harvest commercial fertilizer and year period pesticide use and pest management beginning after practices. NASS conducts field crop agricultural chemical use surveys in the 2019 harvest cooperation with USDA’s Economic and ending with Research Service as part of the the 2020 harvest. Agricultural Resource Management (Table 4) Survey. NASS conducted the soybean chemical use survey in the fall of 2020. Access the Data Fertilizer Use Access 2020 soybean chemical use Fertilizer refers to a soil-enriching input that contains one or more plant data as well as results from prior (or nutrients. Nitrogen, phosphate, potash, and sulfur were the most widely earlier) soybean chemical use surveys used fertilizer materials on soybeans. -

The Best Indian Diet Plan for Weight Loss
The Best Indian Diet Plan for Weight Loss Indian cuisine is known for its vibrant spices, fresh herbs and wide variety of rich flavors. Though diets and preferences vary throughout India, most people follow a primarily plant-based diet. Around 80% of the Indian population practices Hinduism, a religion that promotes a vegetarian or lacto-vegetarian diet. The traditional Indian diet emphasizes a high intake of plant foods like vegetables, lentils and fruits, as well as a low consumption of meat. However, obesity is a rising issue in the Indian population. With the growing availability of processed foods, India has seen a surge in obesity and obesity-related chronic diseases like heart disease and diabetes . This document explains how to follow a healthy Indian diet that can promote weight loss. It includes suggestions about which foods to eat and avoid and a sample menu for one week. A Healthy Traditional Indian Diet Traditional plant-based Indian diets focus on fresh, whole ingredients — ideal foods to promote optimal health. Why Eat a Plant-Based Indian Diet? Plant-based diets have been associated with many health benefits, including a lower risk of heart disease, diabetes and certain cancers such as breast and colon cancer. Additionally, the Indian diet, in particular, has been linked to a reduced risk of Alzheimer’s disease. Researchers believe this is due to the low consumption of meat and emphasis on vegetables and fruits. Following a healthy plant-based Indian diet may not only help decrease the risk of chronic disease, but it can also encourage weight loss. -

Reduced Mir-181D Level in Obesity and Its Role in Lipid Metabolism Via
www.nature.com/scientificreports OPEN Reduced miR-181d level in obesity and its role in lipid metabolism via regulation of ANGPTL3 Received: 12 October 2018 Mohamed Abu-Farha 1, Preethi Cherian1, Irina Al-Khairi1, Rasheeba Nizam2, Accepted: 29 July 2019 Abdullah Alkandari3, Hossein Arefanian 4, Jaakko Tuomilehto5, Fahd Al-Mulla2 & Published: xx xx xxxx Jehad Abubaker1 Obesity impacts the endocrine and metabolic functions of the adipose tissue. There is increasing interest in the role of epigenetic factors in obesity and its impact on diabetes and dyslipidemia. One such substance, miR-181, reduces plasma triglyceride levels in mice by targeting isocitrate dehydrogenase 1. In the other hand, the adipocyte diferentiation and lipid regulating hormone angiopoietin-like 3 (ANGPTL3) is a known regulator of circulating apolipoproteins through its inhibition of the lipoprotein lipase activity. We aimed to study the miR-181d expression in the blood and adipose tissue in a cohort of obese and non-obese people, assessing its possible role in obesity. We also aimed to confrm whether miR-181d can bind and regulate ANGPTL3. miR-181d expression levels were investigated in 144 participants, 82 who were non-obese (body mass index [BMI] < 30) and 62 who were obese (BMI > 30). miR-181d levels in plasma and adipose tissue were measured by RT-PCR. Hepatocyte cell cultures were assessed by overexpression and 3′-UTR-luciferase assays for miR-181d binding to its target protein and its efect on the protein. The plasma levels of ANGPTL3 were also measured by ELISA. The miR-181d levels were signifcantly lower in obese than in non-obese individuals. -
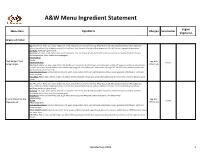
Menu Ingredient Statement
A&W Menu Ingredient Statement Vegan/ Menu Item Ingredients Allergen Sensitivities Vegetarian Burgers and Chicken Bun: Wheat Flour, Water, Corn Syrup, Soybean Oil, Yeast, Contains 2% or less of the following: Wheat Gluten, Salt, Malt, Dough Conditioners (Monoglycerides, Sodium Stearoyl Lactylate, Azodicarbonamide), Artificial Flavor, Yeast Nutrients (Calcium Sulfate, Ammonium Chloride), Calcium Propionate (Preservative). Beef Patty: Hamburger (ground beef). Seasoning: Salt, sugar, spices, paprika, dextrose, onion powder, corn starch, garlic powder, hydrolyzed cornprotein, extractive of paprika, disodium inosinate, disodium guanylate, silicon dioxide (anti-caking agent). Iceberg Lettuce Tomato Papa Burger/ Papa Egg, Milk, Yellow Onion Slices Gluten Burger Single Papa Sauce: Soybean oil, water, sugar, pickle relish (pickles, corn sweeteners, distilled vinegar, salt, xanthan gum, alum 0.10% potassium sorbate as a preservative, Wheat, Soy turmeric, natural spice flavors), tomato paste, distilled vinegar, egg yolk, salt, xanthan gum, artificial color including FD&C Red #40, spices, oleoresin paprika, Beta Apo-8-Carotenal, natural flavorings. Sharp American Cheese: Cultured milk and skim milk, water, cream, sodium citrate, salt, sorbic acid (preservative), sodium phosphate, artificial color, acetic acid, lecithin, enzymes. Pickle Slices: Pickles, water, distilled vinegar, salt, calcium chloride, potassium sorbate (as a preservative), polysorbate 80, natural flavors, turmeric oleoresin, garlic powder. Bun: Wheat Flour, Water, Corn Syrup, Soybean Oil, Yeast, Contains 2% or less of the following: Wheat Gluten, Salt, Malt, Dough Conditioners (Monoglycerides, Sodium Stearoyl Lactylate, Azodicarbonamide), Artificial Flavor, Yeast Nutrients (Calcium Sulfate, Ammonium Chloride), Calcium Propionate (Preservative). Beef Patty: Hamburger (ground beef). Seasoning: Salt, sugar, spices, paprika, dextrose, onion powder, corn starch, garlic powder, hydrolyzed cornprotein, extractive of paprika, disodium inosinate, disodium guanylate, silicon dioxide (anti-caking agent).