And Emerging, Pivotal Signalling Pathways in Metastatic Breast Cancer
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Proteomics and Drug Repurposing in CLL Towards Precision Medicine
cancers Review Proteomics and Drug Repurposing in CLL towards Precision Medicine Dimitra Mavridou 1,2,3, Konstantina Psatha 1,2,3,4,* and Michalis Aivaliotis 1,2,3,4,* 1 Laboratory of Biochemistry, School of Medicine, Faculty of Health Sciences, Aristotle University of Thessaloniki, GR-54124 Thessaloniki, Greece; [email protected] 2 Functional Proteomics and Systems Biology (FunPATh)—Center for Interdisciplinary Research and Innovation (CIRI-AUTH), GR-57001 Thessaloniki, Greece 3 Basic and Translational Research Unit, Special Unit for Biomedical Research and Education, School of Medicine, Aristotle University of Thessaloniki, GR-54124 Thessaloniki, Greece 4 Institute of Molecular Biology and Biotechnology, Foundation of Research and Technology, GR-70013 Heraklion, Greece * Correspondence: [email protected] (K.P.); [email protected] (M.A.) Simple Summary: Despite continued efforts, the current status of knowledge in CLL molecular pathobiology, diagnosis, prognosis and treatment remains elusive and imprecise. Proteomics ap- proaches combined with advanced bioinformatics and drug repurposing promise to shed light on the complex proteome heterogeneity of CLL patients and mitigate, improve, or even eliminate the knowledge stagnation. In relation to this concept, this review presents a brief overview of all the available proteomics and drug repurposing studies in CLL and suggests the way such studies can be exploited to find effective therapeutic options combined with drug repurposing strategies to adopt and accost a more “precision medicine” spectrum. Citation: Mavridou, D.; Psatha, K.; Abstract: CLL is a hematological malignancy considered as the most frequent lymphoproliferative Aivaliotis, M. Proteomics and Drug disease in the western world. It is characterized by high molecular heterogeneity and despite the Repurposing in CLL towards available therapeutic options, there are many patient subgroups showing the insufficient effectiveness Precision Medicine. -

Lung Cancer Drugs in the Pipeline
HemOnc today | JANUARY 10, 2016 | Healio.com/HemOnc 5 Lung Cancer Drugs in the Pipeline HEMONC TODAY presents this guide to drugs in phase 2 or phase 3 development for lung cancer-related indications. Clinicians can use this chart as a quick reference to learn about the status of those drugs that may be clinically significant to their practice. Generic name (Brand name, Manufacturer) Indication(s) Development status abemaciclib (Eli Lilly) non–small cell lung cancer phase 3 ABP 215 (Allergan/Amgen) non–small cell lung cancer (advanced disease) phase 3 ACP-196 (Acerta Pharma) non–small cell lung cancer (advanced disease) phase 2 ado-trastuzumab emtansine (Kadcyla, Genentech) non–small cell lung cancer (HER-2–positive disease) phase 2 afatinib (Gilotrif, Boehringer Ingelheim) lung cancer (squamous cell carcinoma) phase 3 aldoxorubicin (CytRx) small cell lung cancer phase 2 alectinib (Alecensa, Genentech) non–small cell lung cancer (second-line treatment of ALK-positive disease) phase 2 non–small cell lung cancer (first-line treatment of ALK-positive disease); phase 3 alisertib (Takeda) malignant mesothelioma, small cell lung cancer phase 2 avelumab (EMD Serono/Pfizer) non–small cell lung cancer phase 3 AZD9291 (AstraZeneca) non–small cell lung cancer (first-line treatment of advancedEGFR -positive disease; phase 3 second-line treatment of advanced EGFR-positive, T790M-positive disease) bavituximab (Peregrine Pharmaceuticals) non–small cell lung cancer (previously treated advanced/metastatic disease) phase 3 belinostat (Beleodaq, Spectrum -

Predictive QSAR Tools to Aid in Early Process Development of Monoclonal Antibodies
Predictive QSAR tools to aid in early process development of monoclonal antibodies John Micael Andreas Karlberg Published work submitted to Newcastle University for the degree of Doctor of Philosophy in the School of Engineering November 2019 Abstract Monoclonal antibodies (mAbs) have become one of the fastest growing markets for diagnostic and therapeutic treatments over the last 30 years with a global sales revenue around $89 billion reported in 2017. A popular framework widely used in pharmaceutical industries for designing manufacturing processes for mAbs is Quality by Design (QbD) due to providing a structured and systematic approach in investigation and screening process parameters that might influence the product quality. However, due to the large number of product quality attributes (CQAs) and process parameters that exist in an mAb process platform, extensive investigation is needed to characterise their impact on the product quality which makes the process development costly and time consuming. There is thus an urgent need for methods and tools that can be used for early risk-based selection of critical product properties and process factors to reduce the number of potential factors that have to be investigated, thereby aiding in speeding up the process development and reduce costs. In this study, a framework for predictive model development based on Quantitative Structure- Activity Relationship (QSAR) modelling was developed to link structural features and properties of mAbs to Hydrophobic Interaction Chromatography (HIC) retention times and expressed mAb yield from HEK cells. Model development was based on a structured approach for incremental model refinement and evaluation that aided in increasing model performance until becoming acceptable in accordance to the OECD guidelines for QSAR models. -

The Ongoing Search for Biomarkers of CDK4/6 Inhibitor Responsiveness in Breast Cancer Scott F
MOLECULAR CANCER THERAPEUTICS | REVIEW The Ongoing Search for Biomarkers of CDK4/6 Inhibitor Responsiveness in Breast Cancer Scott F. Schoninger1 and Stacy W. Blain2 ABSTRACT ◥ CDK4 inhibitors (CDK4/6i), such as palbociclib, ribociclib, benefit from these agents, often switching to chemotherapy and abemaciclib, are approved in combination with hormonal within 6 months. Some patients initially benefit from treatment, therapy as a front-line treatment for metastatic HRþ,HER2- but later develop secondary resistance. This highlights the need breast cancer. Their targets, CDK4 and CDK6, are cell-cycle for complementary or companion diagnostics to pinpoint – regulatory proteins governing the G1 S phase transition across patients who would respond. In addition, because CDK4 is a many tissue types. A key challenge remains to uncover biomar- bona fide target in other tumor types where CDK4/6i therapy is kers to identify those patients that may benefit from this class of currently in clinical trials, the lack of target identification may drugs. Although CDK4/6i addition to estrogen modulation ther- obscure benefit to a subset of patients there as well. This review apy essentially doubles the median progression-free survival, summarizes the current status of CDK4/6i biomarker test devel- overall survival is not significantly increased. However, in reality opment, both in clinical trials and at the bench, with particular only a subset of treated patients respond. Many patients exhibit attention paid to those which have a strong biological basis as primary resistance to CDK4/6 inhibition and do not derive any well as supportive clinical data. Introduction well (7). Although these results are promising, the clinical use of CDK4/6 inhibitors is confounded by the high individual variability in Breast cancer is the most common women's cancer worldwide, clinical response. -

Assessment for Clinical Trial Eligibility Testing in a Molecular Registry (PRAEGNANT) in Germany Hanna Huebner1†, Christian M
Huebner et al. BMC Cancer (2020) 20:1091 https://doi.org/10.1186/s12885-020-07546-1 RESEARCH ARTICLE Open Access Heregulin (HRG) assessment for clinical trial eligibility testing in a molecular registry (PRAEGNANT) in Germany Hanna Huebner1†, Christian M. Kurbacher2†, Geoffrey Kuesters3, Andreas D. Hartkopf4, Michael P. Lux5, Jens Huober6, Bernhard Volz7, Florin-Andrei Taran8, Friedrich Overkamp9, Hans Tesch10, Lothar Häberle1,11, Diana Lüftner12, Markus Wallwiener13, Volkmar Müller14, Matthias W. Beckmann1, Erik Belleville15, Matthias Ruebner1, Michael Untch16, Peter A. Fasching1* , Wolfgang Janni6, Tanja N. Fehm17, Hans-Christian Kolberg18, Diethelm Wallwiener4, Sara Y. Brucker4, Andreas Schneeweiss19 and Johannes Ettl20 Abstract Background: Eligibility criteria are a critical part of clinical trials, as they define the patient population under investigation. Besides certain patient characteristics, clinical trials often include biomarker testing for eligibility. However, patient-identification mostly relies on the trial site itself and is often a time-consuming procedure, which could result in missing out on potentially eligible patients. Pre-selection of those patients using a registry could facilitate the process of eligibility testing and increase the number of identified patients. One aim with the PRAEGN ANT registry (NCT02338167) is to identify patients for therapies based on clinical and molecular data. Here, we report eligibility testing for the SHERBOC trial using the German PRAEGNANT registry. Methods: Heregulin (HRG) has been reported to identify patients with better responses to therapy with the anti- HER3 monoclonal antibody seribantumab (MM-121). The SHERBOC trial investigated adding seribantumab (MM-121) to standard therapy in patients with advanced HER2-negative, hormone receptor–positive (HR-positive) breast cancer and HRG overexpression. -

Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy
cancers Review Primary and Acquired Resistance to Immunotherapy in Lung Cancer: Unveiling the Mechanisms Underlying of Immune Checkpoint Blockade Therapy Laura Boyero 1 , Amparo Sánchez-Gastaldo 2, Miriam Alonso 2, 1 1,2,3, , 1,2, , José Francisco Noguera-Uclés , Sonia Molina-Pinelo * y and Reyes Bernabé-Caro * y 1 Institute of Biomedicine of Seville (IBiS) (HUVR, CSIC, Universidad de Sevilla), 41013 Seville, Spain; [email protected] (L.B.); [email protected] (J.F.N.-U.) 2 Medical Oncology Department, Hospital Universitario Virgen del Rocio, 41013 Seville, Spain; [email protected] (A.S.-G.); [email protected] (M.A.) 3 Centro de Investigación Biomédica en Red de Cáncer (CIBERONC), 28029 Madrid, Spain * Correspondence: [email protected] (S.M.-P.); [email protected] (R.B.-C.) These authors contributed equally to this work. y Received: 16 November 2020; Accepted: 9 December 2020; Published: 11 December 2020 Simple Summary: Immuno-oncology has redefined the treatment of lung cancer, with the ultimate goal being the reactivation of the anti-tumor immune response. This has led to the development of several therapeutic strategies focused in this direction. However, a high percentage of lung cancer patients do not respond to these therapies or their responses are transient. Here, we summarized the impact of immunotherapy on lung cancer patients in the latest clinical trials conducted on this disease. As well as the mechanisms of primary and acquired resistance to immunotherapy in this disease. Abstract: After several decades without maintained responses or long-term survival of patients with lung cancer, novel therapies have emerged as a hopeful milestone in this research field. -

RB1 Dual Role in Proliferation and Apoptosis: Cell Fate Control and Implications for Cancer Therapy
www.impactjournals.com/oncotarget/ Oncotarget, Vol. 6, No. 20 RB1 dual role in proliferation and apoptosis: Cell fate control and implications for cancer therapy Paola Indovina1,2, Francesca Pentimalli3, Nadia Casini2, Immacolata Vocca3, Antonio Giordano1,2 1Sbarro Institute for Cancer Research and Molecular Medicine, Center for Biotechnology, College of Science and Technology, Temple University, Philadelphia, PA, USA 2 Department of Medicine, Surgery and Neuroscience, University of Siena and Istituto Toscano Tumori (ITT), Siena, Italy 3Oncology Research Center of Mercogliano (CROM), Istituto Nazionale Tumori “Fodazione G. Pascale” – IRCCS, Naples, Italy Correspondence to: Antonio Giordano, e-mail: [email protected] Keywords: RB family, apoptosis, E2F, cancer therapy, CDK inhibitors Received: May 14, 2015 Accepted: June 06, 2015 Published: June 18, 2015 ABSTRACT Inactivation of the retinoblastoma (RB1) tumor suppressor is one of the most frequent and early recognized molecular hallmarks of cancer. RB1, although mainly studied for its role in the regulation of cell cycle, emerged as a key regulator of many biological processes. Among these, RB1 has been implicated in the regulation of apoptosis, the alteration of which underlies both cancer development and resistance to therapy. RB1 role in apoptosis, however, is still controversial because, depending on the context, the apoptotic cues, and its own status, RB1 can act either by inhibiting or promoting apoptosis. Moreover, the mechanisms whereby RB1 controls both proliferation and apoptosis in a coordinated manner are only now beginning to be unraveled. Here, by reviewing the main studies assessing the effect of RB1 status and modulation on these processes, we provide an overview of the possible underlying molecular mechanisms whereby RB1, and its family members, dictate cell fate in various contexts. -

Palbociclib for Male Patients with Metastatic Breast Cancer
Author Manuscript Published OnlineFirst on October 24, 2019; DOI: 10.1158/1078-0432.CCR-19-2580 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. CCR-19-2580 Title: FDA Approval Summary: Palbociclib for Male Patients with Metastatic Breast Cancer Authors: Suparna Wedam1*, Lola Fashoyin-Aje1*, Erik Bloomquist1, Shenghui Tang1, Rajeshwari Sridhara1, Kirsten B. Goldberg2, Marc R. Theoret1, Laleh Amiri-Kordestani1, Richard Pazdur1,2, Julia A. Beaver1 Authors’ Affiliation: 1Center for Drug Evaluation and Research, U.S. Food and Drug Administration; 2Oncology Center of Excellence, U.S. Food and Drug Administration Running Title: FDA Approval of Palbociclib for Male Breast Cancer Corresponding Author: Suparna Wedam, Office of Hematology and Oncology Products, CDER, U.S. Food and Drug Administration, WO22 Room 2112, 10903 New Hampshire Avenue, Silver Spring, MD 20993. Phone: 301-796-1776 Fax: 301-796-9909. Email: [email protected] *: SW and LF-A contributed equally to this publication. Note: This is a U.S. Government work. There are no restrictions on its use. Disclosure of Potential Conflicts of Interest: The authors report no financial interests or relationships with the commercial sponsors of any products discussed in this report. Word count: Abstract, 187. Text: 2836. Tables: 1. Figures: 1. References: 17 1 Downloaded from clincancerres.aacrjournals.org on September 27, 2021. © 2019 American Association for Cancer Research. Author Manuscript Published OnlineFirst on October 24, 2019; DOI: 10.1158/1078-0432.CCR-19-2580 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract On April 4, 2019, the Food and Drug Administration (FDA) approved a supplemental new drug application for palbociclib (IBRANCE®), to expand the approved indications in women with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced or metastatic breast cancer (MBC) in combination with an aromatase inhibitor or fulvestrant, to include men. -

2017 Immuno-Oncology Medicines in Development
2017 Immuno-Oncology Medicines in Development Adoptive Cell Therapies Drug Name Organization Indication Development Phase ACTR087 + rituximab Unum Therapeutics B-cell lymphoma Phase I (antibody-coupled T-cell receptor Cambridge, MA www.unumrx.com immunotherapy + rituximab) AFP TCR Adaptimmune liver Phase I (T-cell receptor cell therapy) Philadelphia, PA www.adaptimmune.com anti-BCMA CAR-T cell therapy Juno Therapeutics multiple myeloma Phase I Seattle, WA www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 "armored" CAR-T Juno Therapeutics recurrent/relapsed chronic Phase I cell therapy Seattle, WA lymphocytic leukemia (CLL) www.junotherapeutics.com Memorial Sloan Kettering New York, NY anti-CD19 CAR-T cell therapy Intrexon B-cell malignancies Phase I Germantown, MD www.dna.com ZIOPHARM Oncology www.ziopharm.com Boston, MA anti-CD19 CAR-T cell therapy Kite Pharma hematological malignancies Phase I (second generation) Santa Monica, CA www.kitepharma.com National Cancer Institute Bethesda, MD Medicines in Development: Immuno-Oncology 1 Adoptive Cell Therapies Drug Name Organization Indication Development Phase anti-CEA CAR-T therapy Sorrento Therapeutics liver metastases Phase I San Diego, CA www.sorrentotherapeutics.com TNK Therapeutics San Diego, CA anti-PSMA CAR-T cell therapy TNK Therapeutics cancer Phase I San Diego, CA www.sorrentotherapeutics.com Sorrento Therapeutics San Diego, CA ATA520 Atara Biotherapeutics multiple myeloma, Phase I (WT1-specific T lymphocyte South San Francisco, CA plasma cell leukemia www.atarabio.com -

A Phase II Single Arm Study of Palbociclib in Patients with Metastatic HER2-Positive Breast Cancer with Brain Metastasis
IRB #: STU00202582-CR0003 Approved by NU IRB for use on or after 1/28/2019 through 1/27/2020. A Phase II Single Arm Study of Palbociclib in Patients with Metastatic HER2-positive Breast Cancer with Brain Metastasis Principal Investigator: Massimo Cristofanilli, MD Professor of Medicine Associate Director of Translational Research and Precision Medicine Department of Medicine-Hematology and Oncology Robert H Lurie Comprehensive Cancer Center Feinberg School of Medicine 710 N Fairbanks Court, Olson Building, Suite 8-250A Chicago, IL 60611 Tel: 312-503-5488 Email: [email protected] NU Sub-Investigator(s): Northwestern University Robert H. Lurie Comprehensive Cancer Center Priya Kumthekar, MD Jonathan Strauss Luis Blanco Sofia Garcia Northwestern Lake Forest Hospital Valerie Nelson, MD Affiliate Site PIs: Jenny Chang, MD Houston Methodist Hospital/Houston Methodist Cancer Center 6445 Main Street, P24-326 Houston, Texas 77030 Tel: 713-441-9948 [email protected] Biostatistician: Alfred Rademaker [email protected] Study Intervention(s): Palbociclib (Ibrance) IND Number: Exempt IND Holder: N/A Funding Source: Pfizer Version Date: August 15, 2017 (Amendment 5) Coordinating Center: Clinical Research Office Robert H. Lurie Comprehensive Cancer Center Northwestern University 676 N. St. Clair, Suite 1200 Chicago, IL 60611 http://cancer.northwestern.edu/CRO/index.cfm 1 Version :08.15.2017 IRB #: STU00202582-CR0003 Approved by NU IRB for use on or after 1/28/2019 through 1/27/2020. Table of Contents STUDY SCHEMA ........................................................................................................................... -
Palbociclib Capsules PALBACE®
For the use only of Registered Medical Practitioner (Oncologist) or a Hospital or a Laboratory. Palbociclib Capsules PALBACE® 1. GENERIC NAME Palbociclib 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each hard capsule contains 75 mg, 100 mg and 125 mg of Palbociclib. List of excipients: Microcrystalline cellulose, lactose monohydrate, sodium starch glycolate, colloidal silicon dioxide, magnesium stearate, and hard gelatin capsule shells. The light orange, light orange/caramel and caramel opaque capsule shells contain gelatin, red iron oxide, yellow iron oxide, and titanium dioxide; and the printing ink contains shellac, titanium dioxide, ammonium hydroxide, propylene glycol and simethicone. All strengths/presentations of this product may not be marketed. 3. DOSAGE FORM AND STRENGTH Hard gelatin capsules available in 75 mg, 100 mg and 125 mg strengths. 4. CLINICAL PARTICULARS 4.1 Therapeutic Indications For Women: Palbociclib is indicated for the treatment of hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative locally advanced or metastatic breast cancer: - in combination with an aromatase inhibitor; - in combination with fulvestrant in women who have received prior endocrine therapy (see section 5.2). In pre- or perimenopausal women, the endocrine therapy should be combined with a luteinizing hormone releasing hormone (LHRH) agonist. ®Trademark Proprietor: Pfizer Inc., USA Licensed User: Pfizer Products India Private Limited, India PALBACE Capsule Page 1 of 26 LPDPAB042021 PfLEET Number: 2021-0069100; 2021-0069426 For Men: Palbociclib is indicated for the treatment of hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative advanced or metastatic breast cancer in combination with: an aromatase inhibitor as initial endocrine-based therapy. -
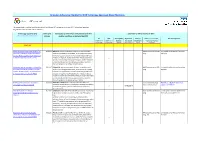
Formulary Adherence Checklist for NICE Technology Appraisals About Medicines
Formulary Adherence Checklist for NICE Technology Appraisals About Medicines This spreadsheet is updated monthly and details Pan Mersey APC adherence to current NICE Technology Appraisals. All guidelines refer to adults unless indicated. Technology appraisal (TA) Date of TA Availability of medicine for NHS patients with this Adherence of APC formulary to NICE Titles are hyperlinks to full guidance Release medical condition, as indicated by NICE Yes N/A Date of APC Implement Time to Notes (e.g. rationale, Pan Mersey Notes (mark 'x' if (mark 'x' if website by (30/90 implement method of making applicable) applicable) upload days of TA ) (days) available) 2017-18 Ribociclib with an aromatase inhibitor for 20/12/17 Ribociclib, with an aromatase inhibitor, is recommended NHSE commissioned RED Link added to Pan Mersey formulary previously untreated, hormone receptor- within its marketing authorisation, as an option for treating drug 28/12/17. positive, HER2-negative, locally advanced hormone receptor-positive, human epidermal growth factor or metastatic breast cancer [TA496] receptor 2‑negative, locally advanced or metastatic breast x cancer as initial endocrine-based therapy in adults. Ribociclib is recommended only if the company provides it with the discount agreed in the patient access scheme. Palbociclib with an aromatase inhibitor for 20/12/17 Palbociclib, with an aromatase inhibitor, is recommended NHSE commissioned RED Link added to Pan Mersey formulary previously untreated, hormone receptor- within its marketing authorisation, as an option for treating drug 28/12/17. positive, HER2-negative, locally advanced hormone receptor-positive, human epidermal growth factor or metastatic breast cancer [TA495] receptor 2-negative, locally advanced or metastatic breast x cancer as initial endocrine-based therapy in adults.