Relevance of Intraocular Pressure Measurement in Ulcerative Microbial Keratitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

RFT List.Xlsx
RFT/Posters Last updated: May 7, 2019 RFT/Posters Session 2 Abstract Title Outcomes of Voretigene Neparvovec-rzyl for Leber Congenital Aaron Nagiel Amaurosis in Eleven Patients: The CHLA Experience AAV2/4-RS1 gene therapy in the retinoschisin knockout mouse Brittni Scruggs model of X-linked retinoschisis Fluorescence Lifetime Imaging Ophthalmoscopy (FLIO) in X-linked Alexandria Vitale retinoschisis RFT/Posters Session 3 Rajvardhan Azad Modified Staging System for FEVR Optical Coherence Tomography Measurements of Retinal and Nikisha Kothari Choroidal Thickness In Preterm Infants The Clinical course and progression of incontinentia pigmenti Charles Calvo retinopathy in treated and untreated patients RFT/Posters Session 7 Omar Moinuddin Patient Outcomes in Coats'-like Retinitis Pigmentosa Andrew Tsai Coats like response in Retinitis Pigmentosa Surgical Management of Advanced Coats' Disease - From Lauren Wright Beginning to End Effect of anti-VEGF therapy on persistent vascular leakage and Irina de la Huerta neovascularization in familial exudative vitreoretinopathy Rapid fire presentation A ROP Expert Confidence in Determining Plus Disease in Borderline Agnieshka Baumritter Images Mike Gaynon Prethreshold ROP - VEGF Inhibition Without VEGF Inhibitors Pre-treatment vs. Post-Treatment Optical Coherence Tomographic Robert Gunzenhauser Angiography in children with strabismic and anisometropic amblyopia. Progression from Pre-Plus Disease to Plus Disease in the G-ROP Alomi Parikh Study Practice patterns changes in the treatment of retinopathy -

HHS Public Access Author Manuscript
HHS Public Access Author manuscript Author Manuscript Author ManuscriptOphthalmology Author Manuscript. Author Author Manuscript manuscript; available in PMC 2016 December 01. Published in final edited form as: Ophthalmology. 2015 December ; 122(12): 2373–2379. doi:10.1016/j.ophtha.2015.06.013. Ability of bottle cap color to facilitate accurate glaucoma patient- physician communication regarding medication identity Pujan Dave, BA1, Guadalupe Villarreal Jr., MD1, David S. Friedman, MD, PhD1, Malik Y. Kahook, MD2, and Pradeep Y. Ramulu, MD, PhD1 1Wilmer Eye Institute, Johns Hopkins University, Baltimore, Maryland 2Department of Ophthalmology, University of Colorado School of Medicine, Aurora, Colorado Abstract Objective—To determine the accuracy of patient-physician communication regarding topical ophthalmic medication use based on bottle cap color, particularly amongst individuals who may have acquired color vision deficiency from glaucoma. Design—Cross-sectional, clinical study. Participants—Patients ≥ 18 years old with primary open-angle, primary angle-closure, pseudoexfoliation, or pigment dispersion glaucoma, bilateral visual acuity of 20/400 or better, and no concurrent conditions that may affect color vision. Methods—One hundred patients provided color descriptions of 11 distinct medication bottle caps. Patient-produced color descriptors were then presented to three physicians. Each physician matched each color descriptor to the medication they thought the descriptor was describing. Main Outcome Measures—Frequency of patient-physician agreement, occurring when all three physicians accurately matched the patient-produced color descriptor to the correct medication. Multivariate regression models evaluated whether patient-physician agreement decreased with degree of better-eye visual field (VF) damage, color descriptor heterogeneity, and/or color vision deficiency, as determined by Hardy-Rand-Rittler (HRR) score and the Lanthony D15 testing index (D15 CCI). -

Acquired Colour Vision Defects in Glaucoma—Their Detection and Clinical Significance
1396 Br J Ophthalmol 1999;83:1396–1402 Br J Ophthalmol: first published as 10.1136/bjo.83.12.1396 on 1 December 1999. Downloaded from PERSPECTIVE Acquired colour vision defects in glaucoma—their detection and clinical significance Mireia Pacheco-Cutillas, Arash Sahraie, David F Edgar Colour vision defects associated with ocular disease have The aims of this paper are: been reported since the 17th century. Köllner1 in 1912 + to provide a review of the modern literature on acquired wrote an acute description of the progressive nature of col- colour vision in POAG our vision loss secondary to ocular disease, dividing defects + to diVerentiate the characteristics of congenital and into “blue-yellow” and “progressive red-green blindness”.2 acquired defects, in order to understand the type of This classification has become known as Köllner’s rule, colour vision defect associated with glaucomatous although it is often imprecisely stated as “patients with damage retinal disease develop blue-yellow discrimination loss, + to compare classic clinical and modern methodologies whereas optic nerve disease causes red-green discrimina- (including modern computerised techniques) for tion loss”. Exceptions to Köllner’s rule34 include some assessing visual function mediated through chromatic optic nerve diseases, notably glaucoma, which are prima- mechanisms rily associated with blue-yellow defects, and also some reti- + to assess the eVects of acquired colour vision defects on nal disorders such as central cone degeneration which may quality of life in patients with POAG. result in red-green defects. Indeed, in some cases, there might be a non-specific chromatic loss. Comparing congenital and acquired colour vision Colour vision defects in glaucoma have been described defects since 18835 and although many early investigations Congenital colour vision deficiencies result from inherited indicated that red-green defects accompanied glaucoma- cone photopigment abnormalities. -

Ocular Hypertension-A Long-Term Follow-Up of Treated and Untreated Patients
Br J Ophthalmol: first published as 10.1136/bjo.61.11.668 on 1 November 1977. Downloaded from British Jouirnal of Ophthalmology, 1977, 61, 668-674 Ocular hypertension-a long-term follow-up of treated and untreated patients ROBERT DAVID, DESIREE G. LIVINGSTON, AND MAURICE H. LUNTZ From the Department of Ophthalmology, University of the Witwatersrand and Johannesburg Teaching Hospitals, Johannesbuirg, South Africa SUMMARY Sixty-one patients with ocular hypertension (1 17 eyes) were followed up for I to 11 years (average 40 7 months). Ten patients (12 eyes) developed visual field defects and optic disc lesions of glaucomatous type ( 10 2 %). Their average age was lower than the average of the sample, and the defect appeared between 1 and 5 years (average 41 3 months). The risk of developing glaucoma was related to the level of the intraocular pressure. Of the 75 eyes with pressures between 21 and 25 mmHg only 2 developed glaucoma, of the 25 cases with pressures of 26 to 30 only 3, but 7 of the 17 eyes with pressures of 31 mmHg or more did so. Prophylactic cryosurgery was carried out where indicated by the presence of lattice retinal degeneration or holes before starting miotic therapy. Fifty eyes were given antiglaucoma therapy and compared with 67 eyes not treated. Treatment did not prevent the development of glaucoma and did not seem to influence the course of the ocular hypertension. The response to treatment was also valueless in predicting future glaucoma. Two untreated patients with high pressures developed central vein occlusion. As no harmful effect of treatment could be detected in the 50 treated eyes, elderly patients (more than 70 years) with copyright. -

The Eyes Have It! Update on Common Conditions Affecting the Eye
Pharmacy Tech Topics™ VOLUME 22 NO. 2 | APRIL 2017 The Eyes Have It! Update on Common Conditions Affecting the Eye AUTHORS: Steven R. Abel, BS Pharm, PharmD, FASHP Kirk Evoy, PharmD, BCACP, BC-ADM, TTS PEER REVIEWERS: Sami Labib, RPh Rita Edwards, CPhT EDITOR: Patricia M. Wegner, BS Pharm, PharmD, FASHP DESIGN EDITOR: Leann Nelson Pharmacy Tech Topics™ (USPS No. 014-766) is published quarterly for $50 per year by the Illinois Council of Health-System Pharmacists, 4055 N. Perryville Road, Loves Park, IL 61111-8653. Phone 815-227-9292. Periodicals Postage Paid at Rockford, IL and additional mailing offices. POSTMASTER: Send address changes to: Pharmacy Tech Topics™, c/o ICHP, 4055 N. Perryville Road, Loves Park, IL 61111-8653 COPYRIGHT ©2017 by the Illinois Council of Health-System Pharmacists unless otherwise noted. All rights reserved. Pharmacy Tech Topics™ is a trademark of the Illinois Council of Health-System Pharmacists. This module is accredited for 2.5 contact hours of continuing pharmacy education and is recognized by the Pharmacy Technician Certification Board (PTCB). Cover image property of ©2017 Adobe Stock. LEARNING OBJECTIVES Upon completion of this module, the subscriber will be able to: 1. Identify the parts of the eye and the function of each part. 2. Summarize various eye disorders including ocular hypertension, glaucoma, infections, dry eyes, conjunctivitis, age-related macular degeneration, macular edema following retinal vein occlusion, and diabetic macular edema. 3. Discuss brand/generic substitutions, possible side effects, and proper administration of ophthalmic medications. 4. Describe the roles of various ophthalmic agents including those used to treat the following conditions: ocular hypertension, glaucoma, infections, dry eyes, conjunctivitis, age-related macular degeneration, macular edema following retinal vein occlusion, and diabetic macular edema. -

(SUNDROP): Five Years of Screening with Telemedicine
■ CLINICAL SCIENCE ■ Stanford University Network for Diagnosis of Retinopathy of Prematurity (SUNDROP): Five Years of Screening With Telemedicine Natalia Fijalkowski, BA; Luo Luo Zheng, BS; Michael T. Henderson, BA; Sean K. Wang, BS; Matthew B. Wallenstein, MD; Theodore Leng, MD, MS; Darius M. Moshfeghi, MD INTRODUCTION BACKGROUND AND OBJECTIVE: To report the 5-year results of the Stanford University Network for Diag- Retinopathy of prematurity (ROP) is a vision- nosis of Retinopathy of Prematurity (SUNDROP) tele- threatening disease of disordered retinal vasculature medicine initiative. development in premature and low birth weight in- fants.1,2 The underdeveloped retina overcompensates PATIENTS AND METHODS: Infants requiring retinopathy for ischemia at birth by promoting angiogenesis that of prematurity (ROP) screening at six neonatal inten- can damage nearby structures through retinal edema, sive care units from December 1, 2005, to November traction, or detachment.3,4 At United States schools, 30, 2010, were evaluated with remote retinal photogra- ROP accounts for 14% of pediatric blindness.5 The phy by an ROP specialist. Every infant received outpa- World Health Organization (WHO) found ROP to be tient binocular indirect ophthalmoscope examinations the leading cause of avoidable visual impairment in until termination criteria were achieved or until treat- high-income countries and the second leading cause ment. Outcomes were treatment-warranted ROP (TW- in middle-income countries,6 accounting for 15% to ROP, ETROP type 1) and adverse anatomical events. 35% of pediatric blindness in some nations.7-9 Randomized trials and observational studies RESULTS: Five hundred eleven infants (1,022 eyes) were demonstrate that cryotherapy,10,11 laser photocoagu- screened. -

Ophthalmic Medications
CHAPTER 33 Ophthalmic Medications Celtina K. Reinert, PharmD LEARNING OBJECTIVES KEY TERMS AND DEFINITIONS After completing this chapter, you should be able to Aqueous humor — the thick, watery fl uid located between the 1. Review the anatomy and physiology of the eye cornea and the lens. 2. Describe glaucoma and the most commonly used treatment approaches Cataract — an eye condition in 3. Describe the causes and symptoms of conjunctivitis and treatment options which a clouding of the lens occurs. Conjunctiva — the tissue around 4. Identify common causes of blindness the eye. 5. Identify medications used in the eye including their dosage forms, therapeutic Conjunctivitis — infl ammation effects, most common side effects, and mechanisms of action of the conjunctiva. Cornea — clear covering over the front of the eye. he eye is the organ for sight. Many things can affect the eye including diabetes, Cycloplegia — paralysis of the muscle that holds the lens in place. T trauma, vision problems, and allergies. Some of these can be improved with Causes a loss of accommodation or treatments including surgery and medications used in the eye. This chapter will ability to focus the lens. discuss these and how ophthalmic medications are used. Diplopia — double vision. Glaucoma — eye condition that can result from increased pressure in the eye and can cause nerve damage. Intraocular pressure (IOP) — measurement of pressure in the eye, usually < 21 mm Hg. Increases in IOP can lead to glaucoma or blindness. Iris — the colored part of the eye. Macula — focal point on the retina that allows for clear, sharp vision especially when focusing on tasks straight ahead. -

Ocular Hypertension in Myopia: Analysis of Contrast Sensitivity
New Frontiers in Ophthalmology Research Article ISSN: 2397-2092 Ocular hypertension in myopia: analysis of contrast sensitivity Arrico L*, Migliorini R, Quercia A, Bianchini D and Nebbioso M Department of Sense Organs, University of Rome “La Sapienza”, Italy Abstract Purpose: we evaluated the evolution of contrast sensitivity reduction in patients affected by ocular hypertension and glaucoma, with low to moderate myopia. We also evaluated the relationship between contrast sensitivity and mean deviation of visual field. Material and methods: 158 patients (316 eyes), aged between 38 and 57 years old, were enrolled and divided into 4 groups: emmetropes, myopes, myopes with ocular hypertension (IOP≥21 ±2 mmHg), myopes with glaucoma. All patients underwent anamnestic and complete eye evaluation, tonometric curves with Goldmann’s applanation tonometer, cup/disc ratio evaluation, gonioscopy by Goldmann’s three-mirrors lens, automated perimetry (Humphrey 30-2 full-threshold test) and contrast sensitivity evaluation by Pelli-Robson charts. A contrast sensitivity under 1,8 Logarithm of the Minimum Angle of Resolution (LogMAR) was considered abnormal. Results: contrast sensitivity was reduced in the group of myopes with ocular hypertension (1,788 LogMAR) and in the group of myopes with glaucoma (1,743 LogMAR), while it was preserved in the group of myopes (2,069 LogMAR) and in the group of emmetropes (1,990 LogMAR). We also found a strong correlation between contrast sensitivity reduction and mean deviation of visual fields in myopes with glaucoma (coefficient relation = 0.86) and in myopes with ocular hypertension (coefficient relation = 0.78). Conclusions: the contrast sensitivity assessment performed by the Pelli-Robson test should be performed in all patients with middle-grade myopia, ocular hypertension and optic disc suspected for glaucoma, as it may be useful in the early diagnosis of the disease. -

2019 CLINICAL GUIDE to OPHTHALMIC DRUGS 23Rd23rd Eeditiondition
2019 CLINICAL GUIDE TO OPHTHALMIC DRUGS 23rd23rd EditionEdition Expert advice to help you eradicate eye disease. Ron Melton, OD Randall Thomas, OD, MPH A Supplement to Patrick Vollmer, OD Supported by an unrestricted grant from Bausch + Lomb 001_dg0519_Cover.indd 3 5/14/19 3:39 PM FROM THE AUTHORS DEAR OPTOMETRIC COLLEAGUES: Supported by an Welcome to the 2019 edition of our annual Clinical Guide to Ophthalmic unrestricted grant from Drugs. In these pages, we offer you our collective clinical wisdom, gleaned Bausch + Lomb from over 75 years of combined experience, and the latest information on developments in ocular therapies and care to help you in your daily practice. Though advancements are always welcome, technology is a two-edged CONTENTS sword that can truly cut both ways. For example, refraction can now be performed by any number of scanning devices. And in many parts of the world, automated refraction is the only way to provide people with Thoughts from the Chair .....3 corrective lenses. 3D printers can now produce eyeglasses. Even more strikingly, eye drop technology will soon be available to dampen the onset and degree of presbyopia. We all know such advances will only continue. What we are getting at here is our strong admonition to begin diversifying Glaucoma Care ...........................5 your practice to embrace more medical eye care services. This is especially important for younger clinicians, since refractive-centric practices are already at risk of being replaced by technology. The time to plan ahead is now. Corticosteroids .........................14 Turning to the state of advancing therapies, the drug pipeline has been influenced by the patent expiration of Restasis and the advent of numerous generics. -

A Longitudinal Study to Establish the Normative Value and to Evaluate Perinatal Factors Affecting Intraocular Pressure in Preterm Infants
A Longitudinal Study to Establish the Normative Value and to Evaluate Perinatal Factors Affecting Intraocular Pressure in Preterm Infants Pak Cheung Ng,1 Barbara Sau Man Tam,2 Cheuk Hon Lee,1 Samuel Po Shing Wong,3 Hugh Simon Lam,1 Alvin Kwan Ho Kwok,2 and Tai Fai Fok1 PURPOSE. To establish a normative range of intraocular pressure vulnerable, high-risk infants after birth, and intraocular pres- (IOP) in preterm infants and to identify important perinatal sure (IOP) can be easily measured by a handheld instrument factors that could affect the IOP during the early weeks of during routine ophthalmic examination. An understanding of neonatal life. the natural maturation process of the visual system, establish- METHODS. The IOP of 104 preterm infants, with a median ment of a normative range of values, and identification of (interquartile range) gestational age of 29.8 (28.7–30.9) weeks important intrinsic or extrinsic factors that may affect various and birth weight of 1208 (1049–1370) g, were assessed in a ocular measurements, including IOP, are essential in assisting clinicians in assessing developmental abnormalities and con- university-affiliated tertiary neonatal center. These infants had 4 IOP measured by a handheld tonometer at 1, 4, 6, 8, and 10 genital diseases involving the eyes. To date, relatively few weeks of postnatal age. The mixed-effects models were used to studies have reported IOP in preterm infants. Of these studies, evaluate the longitudinal IOP measurements and to identify most obtained the IOP measurements in a cross-sectional man- ner.4–10 In only one small trial involving 20 preterm infants critical perinatal factors that would significantly affect the 11 ocular pressure. -
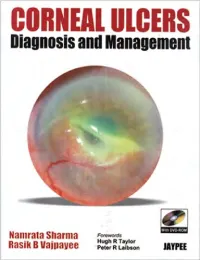
CORNEAL ULCERS Diagnosis and Management
CORNEAL ULCERS Diagnosis and Management System requirement: • Windows XP or above • Power DVD player (Software) • Windows Media Player 10.0 version or above • Quick time player version 6.5 or above Accompanying DVD ROM is playable only in Computer and not in DVD player. Kindly wait for few seconds for DVD to autorun. If it does not autorun then please do the following: • Click on my computer • Click the drive labelled JAYPEE and after opening the drive, kindly double click the file Jaypee CORNEAL ULCERS Diagnosis and Management Namrata Sharma MD DNB MNAMS Associate Professor of Ophthalmology Cornea, Cataract and Refractive Surgery Services Dr. Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi India Rasik B Vajpayee MS FRCSEd FRANZCO Head, Corneal and Cataract Surgery Centre for Eye Research Australia Royal Victorian Eye and Ear Hospital University of Melbourne Australia Forewords Hugh R Taylor Peter R Laibson ® JAYPEE BROTHERS MEDICAL PUBLISHERS (P) LTD New Delhi • Ahmedabad • Bengaluru • Chennai • Hyderabad • Kochi • Kolkata • Lucknow • Mumbai • Nagpur Published by Jitendar P Vij Jaypee Brothers Medical Publishers (P) Ltd B-3 EMCA House, 23/23B Ansari Road, Daryaganj New Delhi 110 002, India Phones: +91-11-23272143, +91-11-23272703, +91-11-23282021, +91-11-23245672 Rel: +91-11-32558559, Fax: +91-11-23276490, +91-11-23245683 e-mail: [email protected] Visit our website: www.jaypeebrothers.com Branches • 2/B, Akruti Society, Jodhpur Gam Road Satellite Ahmedabad 380 015, Phones: +91-79-26926233, -

EYENOVIA, INC. (Exact Name of Registrant As Specified in Its Charter) ______
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 __________________ FORM 8-K __________________ CURRENT REPORT Pursuant to Section 13 or 15(d) of the Securities Exchange Act of 1934 Date of Report (Date of earliest event reported) October 29, 2019 __________________ EYENOVIA, INC. (Exact name of registrant as specified in its charter) __________________ Delaware (State or other jurisdiction of incorporation) 001-38365 47-1178401 (Commission File Number) (IRS Employer Identification No.) 295 Madison Avenue, Suite 2400, New York, New York 10017 (Address of principal executive offices) (Zip Code) Registrant's telephone number, including area code (917) 289-1117 __________________ Check the appropriate box below if the Form 8-K filing is intended to simultaneously satisfy the filing obligation of the registrant under any of the following provisions: ¨ Written communications pursuant to Rule 425 under the Securities Act (17 CFR 230.425) ¨ Soliciting material pursuant to Rule 14a-12 under the Exchange Act (17 CFR 240.14a-12) ¨ Pre-commencement communications pursuant to Rule 14d-2(b) under the Exchange Act (17 CFR 240.14d-2(b)) ¨ Pre-commencement communications pursuant to Rule 13e-4(c) under the Exchange Act (17 CFR 240.13e-4(c)) Securities registered pursuant to Section 12(b) of the Act: Title of each class Trading Symbol(s) Name of each exchange on which registered Common Stock, $0.0001 Par Value EYEN Nasdaq Capital Market Indicate by check mark whether the registrant is an emerging growth company as defined in Rule 405 of the Securities Act of 1933 (§230.405 of this Chapter) or Rule 12b-2 of the Securities Exchange Act of 1934 (§240.12b-2 of this Chapter).