BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Core Neurosurgery
BAYLOR SCOTT & WHITE TEXAS SPINE & JOINT HOSPITAL NEUROLOGICAL SURGERY CLINICAL PRIVILEGES NAME: ________________________________ Initial appointment Reappointment All new applicants must meet the following requirements as approved by the governing body. To be eligible to apply for core privileges in neurological surgery, the initial applicant must meet the following criteria: Successful completion of ACGME or American Osteopathic Association accredited residency in neurological surgery. Required previous experience: Applicants for initial appointment must be able to demonstrate the performance of at least 50 neurological surgical procedures, reflective of the scope of privileges requested, during the last 12 months or demonstrate successful completion of residency or fellowship within the past 12 months. Reappointment requirements: To be eligible to renew core privileges in Neurological Surgery, the applicant must meet the following maintenance of privilege criteria: Current demonstrated competence and an adequate volume of neurological surgery procedures with acceptable results, reflective of the scope of privileges requested, for the past 24 months based on results of ongoing professional practice evaluation and outcomes. Evidence of current ability to perform privileges requested is required of all applicants for renewal of privileges NEUROLOGICAL SURGERY CORE PRIVILEGES Requested: Admit, evaluate, diagnose, consult and provide nonoperative and pre-, intran, and postoperative care to patients of all ages presenting with injuries -

Neurosurgery
KALEIDA HEALTH Name ____________________________________ Date _____________ DELINEATION OF PRIVILEGES - NEUROSURGERY All members of the Department of Neurosurgery at Kaleida Health must have the following credentials: 1. Successful completion of an ACGME accredited Residency, Royal College of Physicians and Surgeons of Canada, or an ACGME equivalent Neurosurgery Residency Program. 2. Members of the clinical service of Neurosurgery must, within five (5) years of appointment to staff, achieve board certification in Neurosurgery. *Maintenance of board certification is mandatory for all providers who have achieved this status* Level 1 (core) privileges are those able to be performed after successful completion of an accredited Neurosurgery Residency program. The removal or restriction of these privileges would require further investigation as to the individual’s overall ability to practice, but there is no need to delineate these privileges individually. PLEASE NOTE: Please check the box for each privilege requested. Do not use an arrow or line to make selections. We will return applications that ignore this directive. LEVEL I (CORE) PRIVILEGES Basic Procedures including: Admission and Follow-Up Repair cranial or dural defect or lesion History and Physical for diagnosis and treatment plan* Seizure Chest tube placement Sterotactic framed localization of lesion Debride wound Sterotactic frameless localization Endotracheal intubation Transsphenoidal surgery of pituitary lesion Excision of foreign body Trauma Insertion of percutaneous arterial -

ICD~10~PCS Complete Code Set Procedural Coding System Sample
ICD~10~PCS Complete Code Set Procedural Coding System Sample Table.of.Contents Preface....................................................................................00 Mouth and Throat ............................................................................. 00 Introducton...........................................................................00 Gastrointestinal System .................................................................. 00 Hepatobiliary System and Pancreas ........................................... 00 What is ICD-10-PCS? ........................................................................ 00 Endocrine System ............................................................................. 00 ICD-10-PCS Code Structure ........................................................... 00 Skin and Breast .................................................................................. 00 ICD-10-PCS Design ........................................................................... 00 Subcutaneous Tissue and Fascia ................................................. 00 ICD-10-PCS Additional Characteristics ...................................... 00 Muscles ................................................................................................. 00 ICD-10-PCS Applications ................................................................ 00 Tendons ................................................................................................ 00 Understandng.Root.Operatons..........................................00 -

Neurosurgery
March 10, 2017 St Elizabeth Healthcare 9:02 am Privileges for: Neurosurgery Request ST. ELIZABETH - EDGEWOOD ST. ELIZABETH - FLORENCE ST. ELIZABETH - FT. THOMAS ST. ELIZABETH - GRANT CO. (Surgical & other invasive procedures requiring general anesthetic are not offered) MEC Approval: August 27, 2009; Rev. November 15, 2012, February 27, 2014 Board Approval: September 14, 2009; Rev. January 7, 2013, May 5, 2014 DEPARTMENT APPROVAL ________Approved ________Disapproved ___________________________________________ ________________ Department/Section Chair Signature Date MINIMUM REQUIREMENTS Degree required: MD or DO Successful completion of an ACGME or AOA accredited residency in neurosurgery. Note: For Practitoners (excluding AHPs) who apply for membership after March 2, 2009 be and remain (with a lapse of no longer than one year) board certified in their principal practice specialty, or become and remain (with a lapse of no longer than one year) board certified within six years of completion of their post-graduate medical training. Only those boards recognized by the American Board of Medical Specialties or the American Osteopathic Association are acceptable. This board certification requirement does not apply to applicants who on March 2, 2009 were members in good standing on the medical staff of the St. Luke Hospitals or St. Elizabeth Medical Center. PRIVILEGES REQUESTED Pursuant to Bylaws Section 6.1.4, practitioners may exercise the privileges requested and awarded below only at facilities where St. Elizabeth Healthcare offers those services. I. Core Privileges: Core privileges in neurosurgery include the care, treatment or services listed immediately below. I specifically acknowledge that board certification alone does not necessarily qualify me to perform all core privileges or assure competence in all clinical areas. -

Cervical Cordotomy in Terminal Cancer
Published online: 2020-11-26 THIEME Review Article | Artigo de Revisão 71 Cervical Cordotomy in Terminal Cancer: Pain Relieving in Oncological Treatment Cordotomia cervical em câncer terminal: Alívio da dor em tratamento oncológico Maria Clara Cardoso Seba1 Henrique Nicola Santo Antonio Bernardo1 Natally Marques Santiago Sarturi2 Thania Gonzalez Rossi2 Newton Maciel de Oliveira3 Paulo Henrique Pires de Aguiar1,2,4 1 Faculdade de Medicina do ABC, Santo André, SP, Brazil Address for correspondence Maria Clara Cardoso Seba, BA, Rua José 2 Divison of Neurosurgery, Hospital Santa Paula, São Paulo, SP, Brazil Abdo Marão, 3418, Votuporanga, São Paulo, 15501-031, Brazil 3 Department of Histology, Pontifícia Universidade Católica de (e-mail: [email protected]). São Paulo, Sorocaba, SP, Brazil 4 Pontifícia Universidade Católica de São Paulo, Sorocaba, Brazil Arq Bras Neurocir 2021;40(1):71–77. Abstract Cordotomy consists in the discontinuation of the lateral spinothalamic tract (LST) in the anterolateral quadrant of the spinal cord, which aims to reduce the transference of Keywords nociceptive information in the dorsal horn of the gray matter of the spinal cord to the ► cordotomy somatosensory cortex. The main indication is for patients with terminal cancer that ► intractable pain have a low life expectancy. It improves the quality of life by relieving pain. The results ► neoplasms are promising and the pain relief rate varies between 69 and 100%. Generally speaking, ► spinothalamic tracts the complications are mostly temporary and not remarkable. Resumo A cordotomia consiste na descontinuação do trato espinotalâmico lateral (LST, na sigla em inglês) no quadrante anterolateral da medula espinhal, que visa reduzir a trans- Palavras-chave ferência de informações nociceptivas no corno dorsal da substância cinzenta da medula ► cordotomia espinhal para o córtex somatossensorial. -

Report: Rs04328‐R1328 North Carolina Department of Health and Human Services Physician Fee Schedule As Of: 07/24/2018
REPORT: RS04328‐R1328 NORTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICES PHYSICIAN FEE SCHEDULE AS OF: 07/24/2018 Physician Fee Schedule Provider Specialty 001 Effective Date: 1/1/2018 The inclusion of a rate on this table does not guarantee that a service is covered. Please refer to the Medicaid Billing Guide and the Medicaid and Health Choice Clinical Policies on the DMA Web Site. Providers should always bill their usual and customary charges. Please use the monthly NC Medicaid Bulletins for additions, changes and deletion to this schedule. Medicaid Maximum Allowable NON-FACILITY PROCEDURE CODE MODIFIER PROCEDURE DESCRIPTION FACILITY RATE RATE EFFECTIVE DATE 01967 NEURAXIAL LABOR ANALGESIA/ANESTHESIA FOR $ 209.63 $ 209.63 01996 DAILY HOSPITAL MANAGEMENT OF EPIDURAL OR $ 38.93 $ 38.93 10021 FINE NEEDLE ASPIRATION; WITHOUT IMAGING $ 52.36 $ 100.48 10022 FINE NEEDLE ASPIRATION; WITH IMAGING GUI $ 51.97 $ 103.17 10030 GUIDE CATHET FLUID DRAINAGE $ 126.07 $ 615.23 10035 PERQ DEV SOFT TISS 1ST IMAG $ 74.46 $ 437.80 10036 PERQ DEV SOFT TISS ADD IMAG $ 37.49 $ 379.35 10040 ACNE SURGERY $ 63.53 $ 72.20 10060 DRAINAGE OF ABSCESS $ 67.39 $ 77.74 10061 DRAINAGE OF ABSCESS $ 120.14 $ 133.85 10080 DRAINAGE OF PILONIDAL CYST $ 68.87 $ 114.75 10081 DRAINAGE OF PILONIDAL CYST $ 120.71 $ 181.14 10120 FOREIGN BODY REMOVAL, SKIN $ 66.08 $ 94.90 10121 FOREIGN BODY REMOVAL, SKIN $ 135.29 $ 185.09 Printed 7/26/2018 Page 1 of 330 REPORT: RS04328‐R1328 NORTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICES PHYSICIAN FEE SCHEDULE AS OF: 07/24/2018 10140 -

NOMESCO Classification of Surgical Procedures
NOMESCO Classification of Surgical Procedures NOMESCO Classification of Surgical Procedures 87:2009 Nordic Medico-Statistical Committee (NOMESCO) NOMESCO Classification of Surgical Procedures (NCSP), version 1.14 Organization in charge of NCSP maintenance and updating: Nordic Centre for Classifications in Health Care WHO Collaborating Centre for the Family of International Classifications in the Nordic Countries Norwegian Directorate of Health PO Box 700 St. Olavs plass 0130 Oslo, Norway Phone: +47 24 16 31 50 Fax: +47 24 16 30 16 E-mail: [email protected] Website: www.nordclass.org Centre staff responsible for NCSP maintenance and updating: Arnt Ole Ree, Centre Head Glen Thorsen, Trine Fresvig, Expert Advisers on NCSP Nordic Reference Group for Classification Matters: Denmark: Søren Bang, Ole B. Larsen, Solvejg Bang, Danish National Board of Health Finland: Jorma Komulainen, Matti Mäkelä, National Institute for Health and Welfare Iceland: Lilja Sigrun Jonsdottir, Directorate of Health, Statistics Iceland Norway: Øystein Hebnes, Trine Fresvig, Glen Thorsen, KITH, Norwegian Centre for Informatics in Health and Social Care Sweden: Lars Berg, Gunnar Henriksson, Olafr Steinum, Annika Näslund, National Board of Health and Welfare Nordic Centre: Arnt Ole Ree, Lars Age Johansson, Olafr Steinum, Glen Thorsen, Trine Fresvig © Nordic Medico-Statistical Committee (NOMESCO) 2009 Islands Brygge 67, DK-2300 Copenhagen Ø Phone: +45 72 22 76 25 Fax: +45 32 95 54 70 E-mail: [email protected] Cover by: Sistersbrandts Designstue, Copenhagen Printed by: AN:sats - Tryk & Design a-s, Copenhagen 2008 ISBN 978-87-89702-69-8 PREFACE Preface to NOMESCO Classification of Surgical Procedures Version 1.14 The Nordic Medico-Statistical Committee (NOMESCO) published the first printed edition of the NOMESCO Classification of Surgical Procedures (NCSP) in 1996. -
Methods Series Report #2016-02
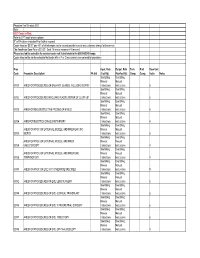
HCUP Methods Series Contact Information: Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality 5600 Fishers Lane Room 07W17B Mail Stop 7W25B Rockville, MD 20857 http://www.hcup-us.ahrq.gov For Technical Assistance with HCUP Products: Email: [email protected] or Phone: 1-866-290-HCUP Recommended Citation: Gibson T, Casto A, Young J, Karnell L, Coenen N. Impact of ICD-10- CM/PCS on Research Using Administrative Databases. HCUP Methods Series Report # 2016- 02 ONLINE. July 25, 2016. U.S. Agency for Healthcare Research and Quality. Available: http://www.hcup-us.ahrq.gov/reports/methods/methods.jsp. TABLE OF CONTENTS 1. EXECUTIVE SUMMARY ..................................................................................................... I 2. INTRODUCTION ................................................................................................................ 1 3. DIFFERENCES BETWEEN ICD-9-CM AND ICD-10-CM/PCS CODING SYSTEMS ........... 4 Diagnosis Coding Systems ............................................................................................. 4 Procedure Coding Systems ............................................................................................ 7 Focus Areas in the Medical and Surgical Section: Root Operations and Approaches ....10 4. LESSONS FROM DUALLY CODED DATA ........................................................................14 Differences in the ICD-9-CM and ICD-10-CM/PCS Coding Systems .............................14 Changes in Coding Rules ..............................................................................................15 -

Neurosurgical Treatment of Chronic Pain FUMIKAZU TAKEDA M.D
Postgrad Med J: first published as 10.1136/pgmj.60.710.905 on 1 December 1984. Downloaded from Postgraduate Medical Journal (December 1984) 60, 905-913 Neurosurgical treatment of chronic pain FUMIKAZU TAKEDA M.D. Neurosurgery Clinic, Saitama Cancer Center 818 Komuro, Ina, Saitama 362, Japan Introduction Cordotomy Neurosurgery is not a first-choice treatment for Cordotomy-section of the spinothalamic tract in chronic pain. It is indicated when chronic pain is the anterolateral quadrant of the spinal cord-used insufficiently relieved by analgesics, or when medica- to be carried out through a laminectomy until Mullan tion is effective but causes unacceptable side effects. et al. (1963, 1965) introduced the percutaneous Neurosurgical procedures may be ablative or aug- technique. Cordotomy is the treatment of choice to mentative (stimulating). An ablative procedure inter- relieve somatic non-dysaesthetic pain of organic rupts pain pathways at one of various levels in the origin in C5 dermatome or below. The most common central nervous system (CNS). In contrast, an aug- candidates for cordotomy are cancer patients, though mentative procedure is non-destructive and is gener- cordotomy is also performed for pain of benign ally considered to activate the inhibitory system in origin (Lorenz, 1976). Lipton (1979) states that copyright. the CNS, thereby suppressing pain perception. percutaneous cervical cordotomy (PCC) is not suffi- There is, however, no neurosurgical procedure ciently used, in spite of its superiority over all other which affords permanent pain relief. This stems from types of pain-relieving procedures. There are two the fact that pain is not simply the result of popular varieties of PCC: High (C1-C2) through a stimulation of specific sensory fibres in the peripheral lateral approach and low (C5-C6) through an and central nervous systems. -

ICD-10-PCS Reference Manual
ICD-10-PCS Reference Manual 3 Table of Contents Preface ............................................................................................ xi Manual organization ................................................................................................................. xi Chapter 1 - Overview ......................................................................................................... xi Chapter 2 - Procedures in the Medical and Surgical section ............................................. xi Chapter 3 - Procedures in the Medical and Surgical-related sections ............................... xi Chapter 4 - Procedures in the ancillary sections ............................................................... xii Appendix A - ICD-10-PCS definitions ................................................................................ xii Appendix B - ICD-10-PCS device and substance classification ........................................ xii Conventions used ..................................................................................................................... xii Root operation descriptions ............................................................................................... xii Table excerpts ................................................................................................................... xiii Chapter 1: ICD-10-PCS overview ......................................................... 15 What is ICD-10-PCS? ............................................................................................................. -
Physician Fee Schedule 2021 Note
Physician Fee Schedule 2021 Note: 2021 Codes in Red; Refer to CPT book for descriptions R" in PA column indicates Prior Auth is required Codes listed as '$0.00" pay 45% of billed amount not to exceed provider’s usual and customary charge for the service The Anesthesia Base Rate is $15.20. Each 15 minute increment=1 time unit. Please use lab fee schedule for covered codes not listed below in the 80000-89249 range. Codes listed on the lab fee schedule that begin with a P or Q are currently non-covered for physicians Proc Inpat. Rate Outpat. Rate Tech. Prof. Base Unit Code Procedure Description PA Ind (Facility) (NonFacility) Comp. Comp. Value Notes See Billing See Billing Manual Manual 00100 ANES FOR PROCEDURES ON SALIVARY GLANDS, INCLUDING BIOPSY Instructions Instructions 5 See Billing See Billing Manual Manual 00102 ANES FOR PROCEDURES INVOLVING PLASTIC REPAIR OF CLEFT LIP Instructions Instructions 6 See Billing See Billing Manual Manual 00103 ANES FOR RECONSTRUCTIVE PROCED OF EYELID Instructions Instructions 5 See Billing See Billing Manual Manual 00104 ANES FOR ELECTROCONVULSIVE THERAPY Instructions Instructions 4 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER EAR ,INC Manual Manual 00120 BIOPSY Instructions Instructions 5 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER Manual Manual 00124 EAR,OTOSCOPY Instructions Instructions 4 See Billing See Billing ANES FOR PROC ON EXTERNAL, MIDDLE, AND INNER EAR, Manual Manual 00126 TYMPANOTOMY Instructions Instructions 4 See Billing See Billing Manual -

Cms Icd-10-Pcs
ICD-10 Procedure Coding System (ICD-10-PCS) RLM.MD 1 ICD-10-PCS Development Background • CMS awarded a contract to 3M Health Information Systems to develop a new procedure coding system • The new system is intended to replace ICD-9-CM Volume 3 for reporting inpatient procedures RLM.MD 2 ICD-10-PCS Development History 1995 - 1996: First draft of ICD-10-PCS completed 1996 - 1997: Training program developed Informal testing conducted ICD-10-PCS revised 1997 - 1998: Independent formal testing conducted ICD-10-PCS revised Final draft completed 1998-present ICD-10-PCS updated annually RLM.MD 3 ICD-10-PCS Major Development Goals • Improve accuracy and efficiency of coding • Reduce training effort • Improve communication with physicians RLM.MD 4 ICD-10-PCS Essential Attributes • Completeness – All substantially different procedures have a unique code • Expandability – The structure of the system allows incorporation of new procedures as unique codes RLM.MD 5 ICD-10-PCS Essential Attributes Standardized terminology –Includes definitions of the terminology used. • While the meaning of specific words can vary in common usage, ICD-10-PCS defines a single meaning for each term used in the system. RLM.MD 6 ICD-10-PCS Essential Attributes Multiaxial – The system has a multi-axial structure. Each character has the same meaning within a section and across sections to the extent possible RLM.MD 7 ICD-10-PCS General Principles • Diagnostic information is not included in the code description • A ‘not elsewhere classified’ option is allowed for new devices