Monomethyl Auristatin E Grafted-Liposomes to Target Prostate Tumor Cell Lines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Polyurethane-Polybenzoxazine Based
POLYURETHANE-POLYBENZOXAZINE BASED SHAPE MEMORY POLYMERS A Thesis Presented to The Graduate Faculty of The University of Akron In Partial Fulfillment of the Requirements for the Degree Master of Science Numan Erden December, 2009 POLYURETHANE-POLYBENZOXAZINE BASED SHAPE MEMORY POLYMERS Numan Erden Thesis Approved: Accepted: _______________________________ _______________________________ Advisor Department Chair Dr. Sadhan C. Jana Dr. Sadhan C. Jana _______________________________ _______________________________ Faculty Reader Dean of the College Dr. Kevin Cavicchi Dr. Stephen Z.D. Cheng _______________________________ _______________________________ Faculty Reader Dean of the Graduate School Dr. Robert A. Weiss Dr. George R. Newkome _______________________________ Date ii ABSTRACT Shape memory polyurethanes (SMPUs) have attracted much attention from academic and industrial researchers due to strong potential in biomedical and consumer applications. Some of the limiting factors of these materials are low recovery stress (RS) and shape recovery (SR). Fundamental studies have focused on the improvement of RS and SR values using primarily two approaches. The first utilizes the nanocomposite route by which a few weight percentages of nanofillers are added to SMPU in order to increase the modulus and consequently to obtain enhancement in recovery stress. Although successful in the case of SMPU with amorphous soft segments, the nanofillers caused reduction in crystallinity of crystalline soft segment leading to deterioration of shape memory properties of SMPUs. In the second approach, chemical additives are added which either chemically bond with SMPU chains or form a separate phase and offer much stronger modulus than the soft and hard segments of SMPU. This second approach was followed in the current study. Polybenzoxazine (PB-a) was incorporated into a thermoplastic polyurethane (PU) formulation, anticipating that it would play a similar role to hard segment and improve the shape memory properties. -

Exploiting Protected Maleimides to Modify Oligonucleotides, Peptides and Peptide Nucleic Acids
Molecules 2015, 20, 6389-6408; doi:10.3390/molecules20046389 OPEN ACCESS molecules ISSN 1420-3049 www.mdpi.com/journal/molecules Review Exploiting Protected Maleimides to Modify Oligonucleotides, Peptides and Peptide Nucleic Acids Clément Paris †, Omar Brun †, Enrique Pedroso and Anna Grandas * Departament de Química Orgànica i IBUB, Facultat de Química, Universitat de Barcelona, Martí i Franquès 1-11, 08028 Barcelona, Spain; E-Mails: [email protected] (C.P.); [email protected] (O.B.); [email protected] (E.P.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +34-934-021-263. Academic Editor: Scott Reed Received: 12 February 2015 / Accepted: 31 March 2015 / Published: 10 April 2015 Abstract: This manuscript reviews the possibilities offered by 2,5-dimethylfuran-protected maleimides. Suitably derivatized building blocks incorporating the exo Diels-Alder cycloadduct can be introduced at any position of oligonucleotides, peptide nucleic acids, peptides and peptoids, making use of standard solid-phase procedures. Maleimide deprotection takes place upon heating, which can be followed by either Michael-type or Diels-Alder click conjugation reactions. However, the one-pot procedure in which maleimide deprotection and conjugation are simultaneously carried out provides the target conjugate more quickly and, more importantly, in better yield. This procedure is compatible with conjugates involving oligonucleotides, peptides and peptide nucleic acids. A variety of cyclic peptides and oligonucleotides can be obtained from peptide and oligonucleotide precursors incorporating protected maleimides and thiols. Keywords: protected maleimides; oligonucleotides; peptides; conjugates; cyclization Molecules 2015, 20 6390 1. Introduction. Maleimide-Involving Click Conjugation Reactions with Oligonucleotides and Polyamides The Michael-type addition of thiols to electron deficient carbon-carbon double bonds is one of the oldest click reactions [1]. -
Exploring Maleimide-Based Nanoparticle Surface Engineering to Control Cellular Interactions # # Joanne C
www.acsanm.org Article Exploring Maleimide-Based Nanoparticle Surface Engineering to Control Cellular Interactions # # Joanne C. Lee, Nathan D. Donahue, Angelina S. Mao, Amber Karim, Mallikharjuna Komarneni, Emily E. Thomas, Emmy R. Francek, Wen Yang, and Stefan Wilhelm* Cite This: https://dx.doi.org/10.1021/acsanm.9b02541 Read Online ACCESS Metrics & More Article Recommendations *sı Supporting Information ABSTRACT: Nanoparticle cellular interactions are governed by nanoparticle surface chemistry and the surface display of functional (bio)molecules. To conjugate and display thiol-containing (bio)- molecules on nanoparticle surfaces, reactions between thiols and functional maleimide groups are often exploited. However, current procedures for modifying nanoparticle surfaces with maleimide groups are complex and can result in nanoparticle aggregation. Here, we demonstrate a straightforward, fast (∼30 min), efficient, and robust one-step surface engineering protocol for modifying gold nanoparticles with functional maleimide groups. We designed a hetero-bifunctional poly(ethylene glycol)-based molecule that attaches efficiently to the gold nanoparticle surface in a single step via its orthopyridyl disulfide (OPSS) terminal end, leaving its maleimide functional group available for downstream reaction with thiols. Using this surface engineering approach, we fabricated gold nanoparticles with near neutral and positive surface charges, respectively. We demonstrate that nanoparticle cellular uptake efficiencies in model mouse breast cancer (4T1) cells, -

Download Product Insert (PDF)
Product Information Monomethyl Auristatin E Item No. 16267 CAS Registry No.: 474645-27-7 Formal Name: N-methyl-L-valyl-N-[(1S,2R)-4-[(2S)- 2-[(1R,2R)-3-[[(1R,2S)-2-hydroxy- H H N 1-methyl-2-phenylethyl]amino]-1- N methoxy-2-methyl-3-oxopropyl]-1- pyrrolidinyl]-2-methoxy-1-[(1S)-1- O H O methylpropyl]-4-oxobutyl]-N-methyl- N L-valinamide O Synonyms: Brentuximab vedotin, MMAE O O O MF: C39H67N5O7 N FW: N 718.0 H Purity: ≥95% H OH Stability: ≥2 years at -20°C Supplied as: A crystalline solid Laboratory Procedures For long term storage, we suggest that monomethyl auristatin E (MMAE) be stored as supplied at -20°C. It should be stable for at least two years. MMAE is supplied as a crystalline solid. A stock solution may be made by dissolving the MMAE in the solvent of choice. MMAE is soluble in organic solvents such as ethanol, DMSO, and dimethyl formamide, which should be purged with an inert gas. The solubility of MMAE in these solvents is approximately 25, 5, and 20 mg/ml, respectively. Further dilutions of the stock solution into aqueous buffers or isotonic saline should be made prior to performing biological experiments. Ensure that the residual amount of organic solvent is insignificant, since organic solvents may have physiological effects at low concentrations. Organic solvent-free aqueous solutions of MMAE can be prepared by directly dissolving the crystalline solid in aqueous buffers. The solubility of MMAE in PBS, pH 7.2, is approximately 0.5 mg/ml. We do not recommend storing the aqueous solution for more than one day. -
NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’S Lymphomas Version 2.2015
NCCN Guidelines Index NHL Table of Contents Discussion NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines® ) Non-Hodgkin’s Lymphomas Version 2.2015 NCCN.org Continue Version 2.2015, 03/03/15 © National Comprehensive Cancer Network, Inc. 2015, All rights reserved. The NCCN Guidelines® and this illustration may not be reproduced in any form without the express written permission of NCCN® . Peripheral T-Cell Lymphomas NCCN Guidelines Version 2.2015 NCCN Guidelines Index NHL Table of Contents Peripheral T-Cell Lymphomas Discussion DIAGNOSIS SUBTYPES ESSENTIAL: · Review of all slides with at least one paraffin block representative of the tumor should be done by a hematopathologist with expertise in the diagnosis of PTCL. Rebiopsy if consult material is nondiagnostic. · An FNA alone is not sufficient for the initial diagnosis of peripheral T-cell lymphoma. Subtypes included: · Adequate immunophenotyping to establish diagnosisa,b · Peripheral T-cell lymphoma (PTCL), NOS > IHC panel: CD20, CD3, CD10, BCL6, Ki-67, CD5, CD30, CD2, · Angioimmunoblastic T-cell lymphoma (AITL)d See Workup CD4, CD8, CD7, CD56, CD57 CD21, CD23, EBER-ISH, ALK · Anaplastic large cell lymphoma (ALCL), ALK positive (TCEL-2) or · ALCL, ALK negative > Cell surface marker analysis by flow cytometry: · Enteropathy-associated T-cell lymphoma (EATL) kappa/lambda, CD45, CD3, CD5, CD19, CD10, CD20, CD30, CD4, CD8, CD7, CD2; TCRαβ; TCRγ Subtypesnot included: · Primary cutaneous ALCL USEFUL UNDER CERTAIN CIRCUMSTANCES: · All other T-cell lymphomas · Molecular analysis to detect: antigen receptor gene rearrangements; t(2;5) and variants · Additional immunohistochemical studies to establish Extranodal NK/T-cell lymphoma, nasal type (See NKTL-1) lymphoma subtype:βγ F1, TCR-C M1, CD279/PD1, CXCL-13 · Cytogenetics to establish clonality · Assessment of HTLV-1c serology in at-risk populations. -
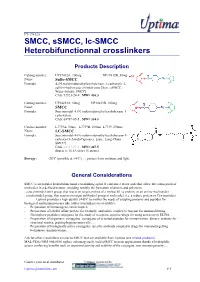
SMCC, Ssmcc, Lc-SMCC
FT-17412A SMCC, sSMCC, lc-SMCC Heterobifunctionnal crosslinkers Products Description Catalog number: UP17412A, 100mg UP17412B, 50mg Name: Sulfo-SMCC Formula : 4-(N-maleimidomethyl)cyclohexane-1-carboxylic 3- sulfo-n-hydroxysuccinimide ester [Syn.: sSMCC, Water-Soluble SMCC] CAS: 92921-24-9 , MW= 436.3 Catalog number: UP34253A, 50mg UP34253B, 100mg Name: SMCC Formula : Succinimidyl-4-(N-maleimidomethyl)cyclohexane-1- carboxylate CAS: 64987-85-5 , MW= 334.3 Catalog number: L7739A, 50mg L7739B, 100mg L7739, 250mg Name: LC-SMCC Formula : Succinimidyl-4-(N-maleimidomethyl)cyclohexane-1- carboxy-(3-AmidoCaproate) [syn.: Long-Chain SMCC] CAS: 64987-85-5 , MW= 447.5 Spacer is 16.1A long (16 atoms) Storage : -20°C (possible at +4°C) (M), protect from moisture and light. General Considerations SMCC is an popular heterobifunctional crosslinking agent. It contains 2 reactivities that allow the conjugation of molecules in a defined manner, avoiding notably the formation of dimers and polymers: . a succinimidyl ester group, that reacts on target amines of a moleucle1 (a protein, or an amino-nucleotide) . a maleimidyl group, that reactos on target sulfhydryl group of molecule2 (i.e. a reduce protein or Cys-peptides) Uptima provides a high quality SMCC to answer the needs of coupling proteins and peptides for biological and immunoassays like (other crosslinkers are available): - Preparation of immunogens carrier-hapten - Preparation of labeled affine probes: for example, antibodies coupled to enzyme for immunoblotting, fluorophore-peptides conjugates for the study of receptors, enzyme-drugs for using as tracers in ELISA… - Preparation of oligomeric conjugates: conjugates of oriented peptides for immunization, dimeric proteins for structural studies, grafting haptens onto cells… - Preparation of biologically active conjugates: specific antibody coupled to drugs for immunotargetting techniques, immunotoxins, … Ask for other crosslinkers similar to SMCC that are available from Uptima (see related products). -

Complete Remission of Refractory, Ulcerated, Primary Cutaneous CD30+ Anaplastic Large Cell Lymphoma Following Brentuximab Vedotin Therapy
Acta Derm Venereol 2015; 95: 233–234 SHORT COMMUNICATION Complete Remission of Refractory, Ulcerated, Primary Cutaneous CD30+ Anaplastic Large Cell Lymphoma Following Brentuximab Vedotin Therapy Nikolaos Patsinakidis, Alexander Kreuter, Rose K. C. Moritz, Markus Stücker, Peter Altmeyer and Katrin Möllenhoff Department of Dermatology, Venereology, and Allergology, Ruhr University Bochum, DE-44791 Germany. E-mail: [email protected] Accepted Apr 9, 2014; Epub ahead of print Apr 15, 2014 Primary cutaneous CD30+ anaplastic large cell lympho- consisting of large, anaplastic, proliferating, CD30+ lymphoid mas (pc-ALCL) belong to the group of rare, non-mycosis cells). Complete computed tomography (CT) scan and bone marrow biopsy were unremarkable. We decided to initiate radiation therapy fungoides T-cell lymphomas (1). Similar to lymphomatoid of the popliteal and inguinal area as well as low-dose therapy papulosis the characteristic immunohistochemical finding with methotrexate (15 mg/week). However, new skin lesions and of pc-ALCL is CD30-positivity of infiltrating neoplastic T lymph node metastases developed within a few weeks. Subsequent cells. To date, only limited data is available on the treatment inguinal lymphadenectomy, a second course of radiation therapy, of pc-ALCL and current recommendations are largely ba- low-dose interferon alpha, bexarotene, and 6 cycles of mono- chemotherapy with gemcitabine did not result in any substantial sed on case reports and small cohort studies (2). Surgical clinical improvement of the disease. Actually, new skin lesions excision and/or radiotherapy are usually performed in limi- occurred with rapid ulceration and secondary superinfection (Fig. ted disease. In cases of disseminated disease, multi-agent 2a). -

Optimization of a Pegylated Glucuronide-Monomethylauristatin E Linker For
Author Manuscript Published OnlineFirst on November 9, 2016; DOI: 10.1158/1535-7163.MCT-16-0343 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Optimization of a PEGylated glucuronide-monomethylauristatin E linker for antibody-drug conjugates Patrick J. Burke, Joseph Z. Hamilton, Scott C. Jeffrey, Joshua H. Hunter, Svetlana O. Doronina, Nicole M. Okeley, Jamie B. Miyamoto, Martha E. Anderson, Ivan J. Stone, Michelle L. Ulrich, Jessica K. Simmons, Erica E. McKinney, Peter D. Senter, and Robert P. Lyon Seattle Genetics, Inc., 21823 30th Drive SE, Bothell, WA 98021 Running title: Optimized glucuronide-monomethylauristatin E linker for ADCs Keywords: antibody-drug conjugates, auristatin, drug-linker, PEGylation, pharmacokinetics Corresponding author: Patrick J. Burke, Seattle Genetics, Inc., 21823 30th Drive SE, Bothell, WA 98021. Phone: 425-527-4766; Fax: 425-527-4109; Email: [email protected] Conflict of interest statement: The authors disclose no potential conflicts of interest. Word count: 5309 words # figures/tables: 7 1 Downloaded from mct.aacrjournals.org on September 27, 2021. © 2016 American Association for Cancer Research. Author Manuscript Published OnlineFirst on November 9, 2016; DOI: 10.1158/1535-7163.MCT-16-0343 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Abstract The emergence of antibody-drug conjugates (ADCs) such as brentuximab vedotin and ado- trastuzumab emtansine has led to increased efforts to identify new payloads and develop improved drug-linker technologies. Most antibody payloads impart significant hydrophobicity to the ADC, resulting in accelerated plasma clearance and suboptimal in vivo activity, particularly for conjugates with high drug-to-antibody ratios (DAR). -

A Phase II Study of Glembatumumab Vedotin for Metastatic Uveal Melanoma
cancers Article A Phase II Study of Glembatumumab Vedotin for Metastatic Uveal Melanoma 1, 2, 3 4 Merve Hasanov y , Matthew J. Rioth y, Kari Kendra , Leonel Hernandez-Aya , Richard W. Joseph 5, Stephen Williamson 6 , Sunandana Chandra 7, Keisuke Shirai 8, Christopher D. Turner 9, Karl Lewis 2, Elizabeth Crowley 10, Jeffrey Moscow 11, Brett Carter 12 and Sapna Patel 1,* 1 Department of Melanoma Medical Oncology, Division of Cancer Medicine, the University of Texas MD Anderson Cancer Center, Houston, TX 77030, USA; [email protected] 2 Division of Medical Oncology and Division of Biomedical Informatics and Personalized Medicine, Department of Medicine, University of Colorado Anschutz Medical Campus, Aurora, CO 80045, USA; [email protected] (M.J.R.); [email protected] (K.L.) 3 Division of Medical Oncology, Department of Medicine, the Ohio State University Comprehensive Cancer Center, Columbus, OH 43210, USA; [email protected] 4 Division of Medical Oncology, Department of Medicine, Washington University in St. Louis, St. Louis, MO 63110, USA.; [email protected] 5 Department of Hematology and Oncology, Mayo Clinic Hospital, Florida, Jacksonville, FL 32224, USA; [email protected] 6 Division of Medical Oncology, Department of Medicine, University of Kansas Medical Center, Kansas City, KS 66160, USA; [email protected] 7 Division of Hematology and Oncology, Department of Medicine, Northwestern University Feinberg School of Medicine, Chicago, IL 60611, USA; [email protected] 8 Division of Hematology -

A Rapid Crosslinkable Maleimide-Modified Hyaluronic
gels Article A Rapid Crosslinkable Maleimide-Modified Hyaluronic Acid and Gelatin Hydrogel Delivery System for Regenerative Applications Kyung Min Yoo 1, Sean V. Murphy 1,* and Aleksander Skardal 2,3,* 1 Wake Forest Institute for Regenerative Medicine, Wake Forest School of Medicine, 391 Technology Way, Winston-Salem, NC 27101, USA; [email protected] 2 Department of Biomedical Engineering, The Ohio State University, Fontana Labs., 140 W. 19th Ave, Columbus, OH 43210, USA 3 Ohio State University and Arthur G. James Comprehensive Cancer Center, Columbus, OH 43210, USA * Correspondence: [email protected] (S.V.M.); [email protected] (A.S.) Abstract: Hydrogels have played a significant role in many applications of regenerative medicine and tissue engineering due to their versatile properties in realizing design and functional requirements. However, as bioengineered solutions are translated towards clinical application, new hurdles and subsequent material requirements can arise. For example, in applications such as cell encapsulation, drug delivery, and biofabrication, in a clinical setting, hydrogels benefit from being comprised of natural extracellular matrix-based materials, but with defined, controllable, and modular properties. Advantages for these clinical applications include ultraviolet light-free and rapid polymerization crosslinking kinetics, and a cell-friendly crosslinking environment that supports cell encapsulation or in situ crosslinking in the presence of cells and tissue. Here we describe the synthesis and charac- terization of maleimide-modified hyaluronic acid (HA) and gelatin, which are crosslinked using a bifunctional thiolated polyethylene glycol (PEG) crosslinker. Synthesized products were evaluated by proton nuclear magnetic resonance (NMR), ultraviolet visibility spectrometry, size exclusion chro- Citation: Yoo, K.M.; Murphy, S.V.; matography, and pH sensitivity, which confirmed successful HA and gelatin modification, molecular Skardal, A. -

Adcetris® (Brentuximab Injection for Intravenous Use – Seattle Genetics, Inc.)
Utilization Review Policy 145 POLICY: Oncology – Adcetris® (brentuximab injection for intravenous use – Seattle Genetics, Inc.) EFFECTIVE DATE: 1/1/2021 LAST REVISION DATE: 09/25/2019 COVERAGE CRITERIA FOR: All Aspirus Medicare Plans OVERVIEW Adcetris is a CD30-directed antibody, produced in Chinese hamster ovary cells, conjugated with monomethyl auristatin E (MMAE).1 CD30 is expressed on systemic anaplastic large cell lymphoma cells and on Hodgkin Reed-Sternberg cells in classical Hodgkin lymphoma and MMAE is a microtubule- disrupting agent. The anticancer activity is due to the binding of Adcetris to the CD30 receptor, followed by internalization and release of MMAE. MMAE then binds to tubulin disrupting the microtubule network leading to cell cycle arrest and apoptosis. Adcetris is FDA-approved for the treatment of adults with: • Previously untreated Stage III or IV classical Hodgkin lymphoma, in combination with doxorubicin, vinblastine, and dacarbazine. • Classical Hodgkin lymphoma at high risk of relapse or progression as post-autologous hematopoietic stem cell transplantation consolidation. • Classical Hodgkin lymphoma after failure of autologous hematopoietic stem cell transplantation or after failure of at least two prior multi-agent chemotherapy regimens in patients who are not autologous hematopoietic stem cell transplantation candidates. • Previously untreated systemic anaplastic large cell lymphoma or other CD30-expressing peripheral T-cell lymphomas, including angioimmunoblastic T-cell lymphoma and peripheral T-cell lymphomas -

Chemical Protein Modification Through Cysteine 3 4 4 5 Smita B
DOI: 10.1002/cbic.201500667 Reviews 1 1 2 2 3 Chemical Protein Modification through Cysteine 3 4 4 5 Smita B. Gunnoo and Annemieke Madder*[a] 5 6 6 7 7 8 8 9 9 10 10 11 11 12 12 13 13 14 14 15 15 16 16 17 17 18 18 19 19 20 20 21 21 22 22 23 23 24 24 25 25 26 26 27 27 28 28 29 29 30 30 31 31 32 32 33 33 34 34 35 35 36 36 37 37 38 38 39 39 40 40 41 41 42 42 43 43 44 44 45 45 46 46 47 47 48 48 49 49 50 50 51 51 52 52 53 53 54 54 55 55 56 56 57 57 ChemBioChem 2016, 17,2–27 2 2016 Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim ÝÝ These are not the final page numbers! Reviews 1 The modification of proteins with non-protein entities is impor- for site-selective modification, including a unique nucleophilici- 1 2 tant for a wealth of applications, and methods for chemically ty, and a low natural abundance—both allowing chemo- and 2 3 modifying proteins attract considerable attention. Generally, regioselectivity. Native cysteine residues can be targeted, or 3 4 modification is desired at a single site to maintain homogenei- Cys can be introduced at a desired site in a protein by means 4 5 ty and to minimise loss of function. Though protein modifica- of reliable genetic engineering techniques. This review on 5 6 tion can be achieved by targeting some natural amino acid chemical protein modification through cysteine should appeal 6 7 side chains, this often leads to ill-defined and randomly modi- to those interested in modifying proteins for a range of appli- 7 8 fied proteins.