Optimization of a Pegylated Glucuronide-Monomethylauristatin E Linker For
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Polyurethane-Polybenzoxazine Based
POLYURETHANE-POLYBENZOXAZINE BASED SHAPE MEMORY POLYMERS A Thesis Presented to The Graduate Faculty of The University of Akron In Partial Fulfillment of the Requirements for the Degree Master of Science Numan Erden December, 2009 POLYURETHANE-POLYBENZOXAZINE BASED SHAPE MEMORY POLYMERS Numan Erden Thesis Approved: Accepted: _______________________________ _______________________________ Advisor Department Chair Dr. Sadhan C. Jana Dr. Sadhan C. Jana _______________________________ _______________________________ Faculty Reader Dean of the College Dr. Kevin Cavicchi Dr. Stephen Z.D. Cheng _______________________________ _______________________________ Faculty Reader Dean of the Graduate School Dr. Robert A. Weiss Dr. George R. Newkome _______________________________ Date ii ABSTRACT Shape memory polyurethanes (SMPUs) have attracted much attention from academic and industrial researchers due to strong potential in biomedical and consumer applications. Some of the limiting factors of these materials are low recovery stress (RS) and shape recovery (SR). Fundamental studies have focused on the improvement of RS and SR values using primarily two approaches. The first utilizes the nanocomposite route by which a few weight percentages of nanofillers are added to SMPU in order to increase the modulus and consequently to obtain enhancement in recovery stress. Although successful in the case of SMPU with amorphous soft segments, the nanofillers caused reduction in crystallinity of crystalline soft segment leading to deterioration of shape memory properties of SMPUs. In the second approach, chemical additives are added which either chemically bond with SMPU chains or form a separate phase and offer much stronger modulus than the soft and hard segments of SMPU. This second approach was followed in the current study. Polybenzoxazine (PB-a) was incorporated into a thermoplastic polyurethane (PU) formulation, anticipating that it would play a similar role to hard segment and improve the shape memory properties. -

Exploiting Protected Maleimides to Modify Oligonucleotides, Peptides and Peptide Nucleic Acids
Molecules 2015, 20, 6389-6408; doi:10.3390/molecules20046389 OPEN ACCESS molecules ISSN 1420-3049 www.mdpi.com/journal/molecules Review Exploiting Protected Maleimides to Modify Oligonucleotides, Peptides and Peptide Nucleic Acids Clément Paris †, Omar Brun †, Enrique Pedroso and Anna Grandas * Departament de Química Orgànica i IBUB, Facultat de Química, Universitat de Barcelona, Martí i Franquès 1-11, 08028 Barcelona, Spain; E-Mails: [email protected] (C.P.); [email protected] (O.B.); [email protected] (E.P.) † These authors contributed equally to this work. * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +34-934-021-263. Academic Editor: Scott Reed Received: 12 February 2015 / Accepted: 31 March 2015 / Published: 10 April 2015 Abstract: This manuscript reviews the possibilities offered by 2,5-dimethylfuran-protected maleimides. Suitably derivatized building blocks incorporating the exo Diels-Alder cycloadduct can be introduced at any position of oligonucleotides, peptide nucleic acids, peptides and peptoids, making use of standard solid-phase procedures. Maleimide deprotection takes place upon heating, which can be followed by either Michael-type or Diels-Alder click conjugation reactions. However, the one-pot procedure in which maleimide deprotection and conjugation are simultaneously carried out provides the target conjugate more quickly and, more importantly, in better yield. This procedure is compatible with conjugates involving oligonucleotides, peptides and peptide nucleic acids. A variety of cyclic peptides and oligonucleotides can be obtained from peptide and oligonucleotide precursors incorporating protected maleimides and thiols. Keywords: protected maleimides; oligonucleotides; peptides; conjugates; cyclization Molecules 2015, 20 6390 1. Introduction. Maleimide-Involving Click Conjugation Reactions with Oligonucleotides and Polyamides The Michael-type addition of thiols to electron deficient carbon-carbon double bonds is one of the oldest click reactions [1]. -
Exploring Maleimide-Based Nanoparticle Surface Engineering to Control Cellular Interactions # # Joanne C
www.acsanm.org Article Exploring Maleimide-Based Nanoparticle Surface Engineering to Control Cellular Interactions # # Joanne C. Lee, Nathan D. Donahue, Angelina S. Mao, Amber Karim, Mallikharjuna Komarneni, Emily E. Thomas, Emmy R. Francek, Wen Yang, and Stefan Wilhelm* Cite This: https://dx.doi.org/10.1021/acsanm.9b02541 Read Online ACCESS Metrics & More Article Recommendations *sı Supporting Information ABSTRACT: Nanoparticle cellular interactions are governed by nanoparticle surface chemistry and the surface display of functional (bio)molecules. To conjugate and display thiol-containing (bio)- molecules on nanoparticle surfaces, reactions between thiols and functional maleimide groups are often exploited. However, current procedures for modifying nanoparticle surfaces with maleimide groups are complex and can result in nanoparticle aggregation. Here, we demonstrate a straightforward, fast (∼30 min), efficient, and robust one-step surface engineering protocol for modifying gold nanoparticles with functional maleimide groups. We designed a hetero-bifunctional poly(ethylene glycol)-based molecule that attaches efficiently to the gold nanoparticle surface in a single step via its orthopyridyl disulfide (OPSS) terminal end, leaving its maleimide functional group available for downstream reaction with thiols. Using this surface engineering approach, we fabricated gold nanoparticles with near neutral and positive surface charges, respectively. We demonstrate that nanoparticle cellular uptake efficiencies in model mouse breast cancer (4T1) cells, -
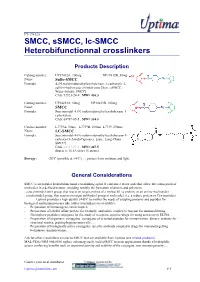
SMCC, Ssmcc, Lc-SMCC
FT-17412A SMCC, sSMCC, lc-SMCC Heterobifunctionnal crosslinkers Products Description Catalog number: UP17412A, 100mg UP17412B, 50mg Name: Sulfo-SMCC Formula : 4-(N-maleimidomethyl)cyclohexane-1-carboxylic 3- sulfo-n-hydroxysuccinimide ester [Syn.: sSMCC, Water-Soluble SMCC] CAS: 92921-24-9 , MW= 436.3 Catalog number: UP34253A, 50mg UP34253B, 100mg Name: SMCC Formula : Succinimidyl-4-(N-maleimidomethyl)cyclohexane-1- carboxylate CAS: 64987-85-5 , MW= 334.3 Catalog number: L7739A, 50mg L7739B, 100mg L7739, 250mg Name: LC-SMCC Formula : Succinimidyl-4-(N-maleimidomethyl)cyclohexane-1- carboxy-(3-AmidoCaproate) [syn.: Long-Chain SMCC] CAS: 64987-85-5 , MW= 447.5 Spacer is 16.1A long (16 atoms) Storage : -20°C (possible at +4°C) (M), protect from moisture and light. General Considerations SMCC is an popular heterobifunctional crosslinking agent. It contains 2 reactivities that allow the conjugation of molecules in a defined manner, avoiding notably the formation of dimers and polymers: . a succinimidyl ester group, that reacts on target amines of a moleucle1 (a protein, or an amino-nucleotide) . a maleimidyl group, that reactos on target sulfhydryl group of molecule2 (i.e. a reduce protein or Cys-peptides) Uptima provides a high quality SMCC to answer the needs of coupling proteins and peptides for biological and immunoassays like (other crosslinkers are available): - Preparation of immunogens carrier-hapten - Preparation of labeled affine probes: for example, antibodies coupled to enzyme for immunoblotting, fluorophore-peptides conjugates for the study of receptors, enzyme-drugs for using as tracers in ELISA… - Preparation of oligomeric conjugates: conjugates of oriented peptides for immunization, dimeric proteins for structural studies, grafting haptens onto cells… - Preparation of biologically active conjugates: specific antibody coupled to drugs for immunotargetting techniques, immunotoxins, … Ask for other crosslinkers similar to SMCC that are available from Uptima (see related products). -

A Rapid Crosslinkable Maleimide-Modified Hyaluronic
gels Article A Rapid Crosslinkable Maleimide-Modified Hyaluronic Acid and Gelatin Hydrogel Delivery System for Regenerative Applications Kyung Min Yoo 1, Sean V. Murphy 1,* and Aleksander Skardal 2,3,* 1 Wake Forest Institute for Regenerative Medicine, Wake Forest School of Medicine, 391 Technology Way, Winston-Salem, NC 27101, USA; [email protected] 2 Department of Biomedical Engineering, The Ohio State University, Fontana Labs., 140 W. 19th Ave, Columbus, OH 43210, USA 3 Ohio State University and Arthur G. James Comprehensive Cancer Center, Columbus, OH 43210, USA * Correspondence: [email protected] (S.V.M.); [email protected] (A.S.) Abstract: Hydrogels have played a significant role in many applications of regenerative medicine and tissue engineering due to their versatile properties in realizing design and functional requirements. However, as bioengineered solutions are translated towards clinical application, new hurdles and subsequent material requirements can arise. For example, in applications such as cell encapsulation, drug delivery, and biofabrication, in a clinical setting, hydrogels benefit from being comprised of natural extracellular matrix-based materials, but with defined, controllable, and modular properties. Advantages for these clinical applications include ultraviolet light-free and rapid polymerization crosslinking kinetics, and a cell-friendly crosslinking environment that supports cell encapsulation or in situ crosslinking in the presence of cells and tissue. Here we describe the synthesis and charac- terization of maleimide-modified hyaluronic acid (HA) and gelatin, which are crosslinked using a bifunctional thiolated polyethylene glycol (PEG) crosslinker. Synthesized products were evaluated by proton nuclear magnetic resonance (NMR), ultraviolet visibility spectrometry, size exclusion chro- Citation: Yoo, K.M.; Murphy, S.V.; matography, and pH sensitivity, which confirmed successful HA and gelatin modification, molecular Skardal, A. -

Chemical Protein Modification Through Cysteine 3 4 4 5 Smita B
DOI: 10.1002/cbic.201500667 Reviews 1 1 2 2 3 Chemical Protein Modification through Cysteine 3 4 4 5 Smita B. Gunnoo and Annemieke Madder*[a] 5 6 6 7 7 8 8 9 9 10 10 11 11 12 12 13 13 14 14 15 15 16 16 17 17 18 18 19 19 20 20 21 21 22 22 23 23 24 24 25 25 26 26 27 27 28 28 29 29 30 30 31 31 32 32 33 33 34 34 35 35 36 36 37 37 38 38 39 39 40 40 41 41 42 42 43 43 44 44 45 45 46 46 47 47 48 48 49 49 50 50 51 51 52 52 53 53 54 54 55 55 56 56 57 57 ChemBioChem 2016, 17,2–27 2 2016 Wiley-VCH Verlag GmbH & Co. KGaA, Weinheim ÝÝ These are not the final page numbers! Reviews 1 The modification of proteins with non-protein entities is impor- for site-selective modification, including a unique nucleophilici- 1 2 tant for a wealth of applications, and methods for chemically ty, and a low natural abundance—both allowing chemo- and 2 3 modifying proteins attract considerable attention. Generally, regioselectivity. Native cysteine residues can be targeted, or 3 4 modification is desired at a single site to maintain homogenei- Cys can be introduced at a desired site in a protein by means 4 5 ty and to minimise loss of function. Though protein modifica- of reliable genetic engineering techniques. This review on 5 6 tion can be achieved by targeting some natural amino acid chemical protein modification through cysteine should appeal 6 7 side chains, this often leads to ill-defined and randomly modi- to those interested in modifying proteins for a range of appli- 7 8 fied proteins. -

Monomethyl Auristatin E Grafted-Liposomes to Target Prostate Tumor Cell Lines
International Journal of Molecular Sciences Article Monomethyl Auristatin E Grafted-Liposomes to Target Prostate Tumor Cell Lines Ariana Abawi 1,†, Xiaoyi Wang 1,† , Julien Bompard 1, Anna Bérot 1, Valentina Andretto 2 , Leslie Gudimard 1, Chloé Devillard 1, Emma Petiot 1, Benoit Joseph 1, Giovanna Lollo 2, Thierry Granjon 1, Agnès Girard-Egrot 1 and Ofelia Maniti 1,* 1 Institut de Chimie et Biochimie Moléculaires et Supramoléculaires, ICBMS UMR 5246, Univ Lyon, Université Lyon 1, CNRS, F-69622 Lyon, France; [email protected] (A.A.); [email protected] (X.W.); [email protected] (J.B.); [email protected] (A.B.); [email protected] (L.G.); [email protected] (C.D.); [email protected] (E.P.); [email protected] (B.J.); [email protected] (T.G.); [email protected] (A.G.-E.) 2 Laboratoire d’Automatique, de Génie des Procédés et de Génie Pharmaceutique, LAGEPP UMR 5007, Univ Lyon, Université Lyon 1, CNRS, F-69622 Lyon, France; [email protected] (V.A.); [email protected] (G.L.) * Correspondence: [email protected]; Tel.: +33-(0)4-72-44-82-14 † These authors have equally contributed to the manuscript. Abstract: Novel nanomedicines have been engineered to deliver molecules with therapeutic po- tentials, overcoming drawbacks such as poor solubility, toxicity or short half-life. Lipid-based carriers such as liposomes represent one of the most advanced classes of drug delivery systems. A Monomethyl Auristatin E (MMAE) warhead was grafted on a lipid derivative and integrated in Citation: Abawi, A.; Wang, X.; fusogenic liposomes, following the model of antibody drug conjugates. -

RSC Advances
RSC Advances PAPER View Article Online View Journal | View Issue Synthesis, characterization, and properties of a novel aromatic ester-based polybenzoxazine Cite this: RSC Adv., 2020, 10, 6953 Chunli Zhu, Xing Gao, Weixi Fan and Xiaofen Fu * Polybenzoxazines with molecular design flexibility have excellent properties by using suitable raw materials. A new benzoxazine monomer terephthalic acid bis-[2-(6-methyl-4H-benzo[e][1,3]oxazin-3-yl)]ethyl ester (TMBE) with bis-ester groups has been synthesized from the simple esterification reaction of terephthaloyl chloride and 2-(6-methyl-4H-benzo[e][1,3]oxazin-3-yl)-ethanol (MB-OH). The chemical structure of TMBE was characterized by Fourier transform infrared spectroscopy (FT-IR) and nuclear magnetic resonance spectroscopy (1H-NMR, 13C-NMR). Polymerization behavior of TMBE was studied by differential scanning calorimetry (DSC) and FT-IR after each cure stage. The cross-linked polybenzoxazine (PTMBE) gave a transparent film through the thermal casting method. The dynamic mechanical analysis of PTMBE Received 5th December 2019 showed that the T was 110 C. Thermogravimetric analysis reveals better thermal stability as evidenced Accepted 16th January 2020 g by the 5% and 10% weight-loss temperatures (Td5 and Td10)ofPTMBE, which were 263 and 289 C, Creative Commons Attribution 3.0 Unported Licence. DOI: 10.1039/c9ra10191h respectively, with a char yield of 27% at 800 C. The tensile test of the film revealed that the elongation rsc.li/rsc-advances at break was up to 14.2%. 1. Introduction exibility of -

High Performance Polybenzoxazines As a Novel Type of Phenolic Resin
#2008 The Society of Polymer Science, Japan REVIEW ARTICLE High Performance Polybenzoxazines as a Novel Type of Phenolic Resin By Tsutomu TAKEICHI,Ã Takehiro KAWAUCHI, and Tarek AGAG Polybenzoxazines that can be obtained by the thermally induced ring-opening polymerization of cyclic benzoxazine monomers are expected as a novel type of phenolic resins. Various benzoxazine monomers are easily synthesized from mono- or diamines, mono- or bisphenols, and formaldehyde. Polybenzoxazines have not only the advantageous properties of the traditional phenolic resins such as the high thermal properties, but also other properties that are not found in the traditional phenolic resins such as the molecular design flexibility, and excellent dimensional stability. The disadvantages of the typical polybenzoxazines are high temperature needed for the cure and brittleness of the cured materials. Further enhancement of thermal properties is also expected for the applications in harsh conditions. Herein, we report on our various approaches for performance enhancement of the polybenzoxazine, including the designs of novel monomers, high molecular weight polymeric precursors, polymer alloys, and hybrids with inorganics. KEY WORDS: Thermoset / Ring-Opening Polymerization / Thermal Properties / Toughness / Polymer Alloy / Organic-Inorganic Hybrid / Nanocomposite / The traditional phenolic resins possess excellent character- Polybenzoxazines provide characteristics found in the tradi- istics such as good heat and chemical resistance, flame tional phenolic resins such as excellent heat resistance and retardancy, electrical properties, low water absorption, and flame retardance. They also provide characteristics that are not low cost due to the inexpensive raw materials and fabricating found in the traditional phenolic resins such as excellent processes. Therefore, they are widely used in various fields dimensional stability, low water absorption and stable low such as structural materials, adhesives, paints and matrix for dielectric properties. -

Recent Progress of High Performance Thermosets Based on Norbornene Functional Benzoxazine Resins
polymers Review Recent Progress of High Performance Thermosets Based on Norbornene Functional Benzoxazine Resins Yin Lu 1, Xinye Yu 1, Lu Han 2,* and Kan Zhang 1,* 1 Research School of Polymeric Materials, School of Materials Science and Engineering, Jiangsu University, Zhenjiang 212013, China; [email protected] (Y.L.); [email protected] (X.Y.) 2 Oak Ridge National Laboratory, Chemical Sciences Division, Oak Ridge, TN 37831, USA * Correspondence: [email protected] (L.H.); [email protected] (K.Z.); Tel.: +86-0571-85016616 (K.Z.) Abstract: With the growing demand for high performance polymeric materials in industry, several types of thermosets such as bismaleimides, advanced epoxy resins, cyanate esters, and phenolic resins have been widely investigated to improve the performance of thermosetting products. Among them, benzoxazine resins have received wide attention due to their extraordinarily rich molecular design flexibility, which can customize our needs and adapt increasing requirements. To further improve the properties of polybenzoxiazines, researchers have found that the introduction of a norbornene functional group into the benzoxazine moiety can effectively improve the comprehensive perfor- mance of polybenzoxazine thermosets. This article focused on reviewing the recent development of high-performance thermosets based on norbornene functional benzoxazine thermosetting resins. Keywords: benzoxazine; norbornene; polybenzoxazine; high performance Citation: Lu, Y.; Yu, X.; Han, L.; Zhang, K. Recent Progress of High 1. Introduction Performance Thermosets Based on In recent years, the application of high-performance thermosets in the field of aerospace, Norbornene Functional Benzoxazine electronic packing, automotive, and other high-performance areas has been extensively Resins. Polymers 2021, 13, 1417. broadened. -

Irdye 800CW Maleimide Labeling Application Guide
Application Guide IRDye® 800CW Maleimide Labeling Published February 2009. Revised January 2018. The most recent version of this Technical Note is posted at licor.com/bio/support. Page 2 - IRDye® 800CW Maleimide Labeling Table of Contents Page I. Introduction 2 II. Labeling Reaction Conditions and Considerations 3 III. Examples 4 Labeling of Affibody® Molecules with IRDye 800CW Maleimide 4 Labeling of Small Molecules with IRDye 800CW Maleimide 4 Labeling of Antibodies with IRDye 800CW Maleimide 5 IV. References 7 I. Introduction IRDye 800CW Maleimide is a functional derivative of infrared dye IRDye 800CW that is reactive toward free–SH (thiol, sulfhydryl) groups. Most molecules that contain free–SH groups can be labeled with maleimide dyes, including IRDye 800CW Maleimide Infrared Dye. IRDye® 800CW Maleimide Labeling- Page 3 II. Labeling Reaction Conditions and Considerations Maleimide groups react with sulfhydryl groups at pH 6.5-7.5, forming a stable thioether bond. A protein, peptide, or biomolecule containing a reactive sulfhydryl group can be labeled with IRDye 800CW using the maleimide functional group of IRDye 800CW Maleimide. The following conditions provide good labeling efficiency: Table 1. Labeling conditions for IRDye 800CW Maleimide. Buffer Phosphate buffered Saline (PBS), pH 7.2 Temperature Ambient* Time 2 hours Dye equivalents per free-SH 2-5 *Ambient temperature is preferred, but 4 °C may be used if the protein is not stable during incubation. If 4 °C is used for the labeling reaction, an overnight incubation should be performed. Generally, PBS works well for labeling, but other buffers with pH 6.5 to 7.5 can be used. -

A Review on Biological and Chemical Potential of Phthalimide and Maleimide Derivatives
Acta Scientific Pharmaceutical Sciences (ISSN: 2581-5423) Volume 3 Issue 9 September 2019 Review Article A Review on Biological and Chemical Potential of Phthalimide and Maleimide Derivatives Mohd Imran1, Ajay Singh Bisht2 and Mohammad Asif2* 1Department of Pharmaceutical Chemistry, Faculty of Pharmacy, Northern Border University, Saudi Arabia 2Department of Pharmaceutical chemistry, Himalayan Institute of Pharmacy and Research, Dehradun, (Uttarakhand), India *Corresponding Author: Mohammad Asif, Department of Pharmaceutical Chemistry, Himalayan Institute of Pharmacy and Research, Dehradun, (Uttarakhand), India. Received: June 27, 2019; Published: August 19, 2019 Abstract Phthalimide and maleimide derivatives have been reported as biologically compounds. In view of broad biological activities of phthalimide and maleimide derivatives, we herein plan to study of various phthalimide and maleimide derivatives, their chemistry, synthesis and biological activities. Diverse biological activities of phthalimide and maleimide and its derivatives have been exhibited such as antibacterial, antifungal, antiviral, analgesic, antiinflamatory, anticancer, anxiolytic, herbicides, insecticides and some other activities.Keywords: The Phthalimides; article also focuses Maleimide; on synthetic Biological methods Activities; of phthalimides Synthesis and maleimide having significant biological activities. Introduction Uses of imides Imide is the form of amide in which the nitrogen atom is at- Utilized in the preparation of pesticides and herbicides, to control diseases in fruits and vegetables. Used to give a fresh and tached to two carbonyl group. Imide refers to any compound bright look to many fruits. In the preparation of polyimides. N-bro- which contains the divalent radical "-C(=O)-NH-C(=O)-". These mosuccinimide is a good brominating agent [3]. compounds are derived from ammonia or primary amine, where two hydrogen atoms are replaced by a bivalent acid group or two monovalent acid groups, resulting in consisting of two carboxylic acid groups (or one dicarboxylic acid) [1].