Policies and Standards and Guidelines Around Food Served to Inpatients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Room Service: Made for YOU
TEXTURE Patient Menu Room Service: Made for YOU How to Order Call 7-MENU (7-6368) from a hospital phone to place your order, or 206-987-6368 from a regular phone. Order between 7 a.m. and 8 p.m. Breakfast is served all day. Lunch and dinner are available to order starting at 11 a.m. Please allow up to 45 minutes for food delivery. You may pre-order your meals and request a delivery time. We will deliver as close to that time as possible. All menu items and preparation methods meet the needs of patients on the immunosuppressed diet. Our call center staff can help you choose meals or modify items to meet food allergy or diet restrictions. Need an interpreter? Please call 7-MENU and let us know. TEXTURE Patient Menu Pureed Diet (non-dysphagia) See also Drinks on page 7 All foods will be blended smooth Breakfast Served all day Entrées Gluten-free options available. Breakfast Pizza Scrambled Egg and Potatoes With pizza sauce, scrambled eggs or tofu, and pizza cheese blend or vegan cheese. Gluten-free option Shelled eggs and house-made breakfast available. potatoes. Breakfast Taco Tofu Scramble and Potatoes Mini corn tortilla and scrambled eggs or tofu. Tofu scramble and house-made breakfast potatoes. Homemade Buttermilk Pancakes Cheese Omelet Plain or chocolate chip. Cheddar cheese and breakfast potatoes. Cinnamon French Toast Local challah, rich egg batter and cinnamon. Hot Cereal Oatmeal Banana-blueberry oatmeal Cream of Rice: regular or strawberry Lunch/Dinner Order from 11 a.m. to 8 p.m. -

Standard Therapeutic Diet Definitions
Adult Diet Name Definition NPO “nil per os” or nothing by mouth. No meal trays or snacks are provided from NPO Nutrition and Food Services. Concurrent tube feeding order is allowed. This diet provides visually clear and minimum residue liquids like juice, broth, tea Clear Liquid Diet and coffee. Caffeine is restricted only if specified. The diet provides 90g of carbohydrate distributed in three meals and is appropriate for patients with diabetes. This diet is nutritionally inadequate for patients of all ages. This diet provides foods that are liquid or semi-liquid at room temperature and Full Liquid Diet strained so that they can be consumed with a straw. A house selection provides (Blenderized Liquid Diet) 1800-2000 calories and approximately 4g of sodium. A well-balanced diet that contains a wide variety of solids and liquids. Offers choices that promote intake of whole grains, fresh fruit and vegetables, homemade Regular Diet soups, fish and poultry and small portions of red meat. A house selection provides 1800-2000 calories and approximately 4g of sodium. A well-balanced diet that contains a wide variety of solids and liquids. Offers choices that promote intake of whole grains, fresh fruit and vegetables, homemade Vegetarian Diet soups, dairy, and eggs. A house selection provides 1800-2000 calories and approximately 4g of sodium. A well-balanced diet that contains a wide variety of solids and liquids. Offers choices that promote intake of whole grains, fresh fruit and vegetables, homemade Vegan Diet soups, and vegetable sources of protein. A house selection provides 1800-2000 calories and approximately 4g of sodium. -

FUTURE of FOOD a Lighthouse for Future Living, Today Context + People and Market Insights + Emerging Innovations
FUTURE OF FOOD A Lighthouse for future living, today Context + people and market insights + emerging innovations Home FUTURE OF FOOD | 01 FOREWORD: CREATING THE FUTURE WE WANT If we are to create a world in which 9 billion to spend. That is the reality of the world today. people live well within planetary boundaries, People don’t tend to aspire to less. “ WBCSD is committed to creating a then we need to understand why we live sustainable world – one where 9 billion Nonetheless, we believe that we can work the way we do today. We must understand people can live well, within planetary within this reality – that there are huge the world as it is, if we are to create a more boundaries. This won’t be achieved opportunities available, for business all over sustainable future. through technology alone – it is going the world, and for sustainable development, The cliché is true: we live in a fast-changing in designing solutions for the world as it is. to involve changing the way we live. And world. Globally, people are both choosing, and that’s a good thing – human history is an This “Future of” series from WBCSD aims to having, to adapt their lifestyles accordingly. endless journey of change for the better. provide a perspective that helps to uncover While no-one wants to live unsustainably, and Forward-looking companies are exploring these opportunities. We have done this by many would like to live more sustainably, living how we can make sustainable living looking at the way people need and want to a sustainable lifestyle isn’t a priority for most both possible and desirable, creating live around the world today, before imagining people around the world. -

Healthy Eating for People with an Internal Pouch
Nutrition and Dietetic Department, St Mark’s Hospital, Tel: 0208 869 2666 Healthy Eating for People with an Internal Pouch After formation of your pouch you will continue to digest and absorb all nutrients normally in your small bowel. Resection of your large bowel results in you absorbing less water and salt, so you will initially experience quite a liquid stool from your Information pouch. However, with time your body will adapt to absorb more water and salt so your stool output will become thicker and your pouch frequency will reduce. You can maintain good health by taking a varied diet with an adequate amount of fluid and salt. This leaflet contains: Information about the reintroduction of food for those with a new pouch Guidelines to help you choose a healthy diet Guidance about diet in relation to developing acceptable pouch function Whilst the experience of others may serve as a guide, remember that as an individual you may respond differently to food, both before and after surgery, and therefore you should base food choices on your own personal tolerance. Reintroduction of food after stoma closure with a new internal for Patients pouch As with any operation, you may find it takes time for your appetite to return. It is advisable to reintroduce food gradually, starting with a light, soft diet which is easy to digest and will not disturb the internal surgical joins (anastomosis). Include protein foods such as meat, fish, eggs, cheese and milk to help wound healing Eat carbohydrates such as bread, cereals, potatoes, pasta and rice to give you energy and to help thicken your pouch output If your appetite is poor take smaller meals with snacks in-between such as cereal, sandwiches, cheese and crackers, yoghurts or nutritious drinks like milk or other supplements which may be recommended by your dietitian. -

TO CHINA FOOD to CHINA 5 Cover Story 封面故事
FOOD TO CHINA, TASTE FROM WORLD 链接全球 . 美味中国 进口食品 FOOD TO CHINA2016 年 5 月 May 2016 FOOD FROM GOURMET ITALY 来自美食国度的意大利食品 UnionAlimentari 意大利中小食品制造商联合会 2016 年全球食品和饮料十大趋势 Preface 卷首语 民以食为天。中国饮食文化绵延 1700 年,多姿多彩的宴席和百家争鸣的风味流派,共同打响了“烹饪王国”的 美誉。2012 年,《舌尖上的中国》在央视首播,引起了广泛的关注。中华美食,给国人带来舌尖上的享受,也向 世界传递源远流长的中华饮食文化。 农业部部长韩长赋指出,我国国民一天要吃 40 多万吨粮食、10 多万吨肉、50 多万吨蔬菜和 20 多万吨水果,数 量十分庞大。在吃货盛行的年代,除了中华美食,吃遍全球,也是我们孜孜不倦的追求。由广东省进口食品协会主 办的行业杂志《FOOD TO CHINA》,任性地坚持“链接全球,美味中国”的情怀,如饥似渴地为国人分享各国的优 质食品及采购资源,我们喜闻乐见其创刊与成长。 作为协会的常务副会长单位,广东省食品进出口集团有限公司,肩负着打造高端国际绿色食品供应链的社会责 任,定将联合各方资源,让“高质、优价、安全”的食品走进千家万户。 进口食品行业已进入快速发展的“黄金十年”,活在当下,唯美食与爱不可辜负,我们已在路上! “Food, the engine of life.” China has been renowned as the Kingdom of Cooking , where diversified styles of banquets and schools of cuisines have been flourishing in its 1700 year history of food culture.” 2012 saw the first-run of A Bite of China, a CCTV (China Central Television) program that soon became a nationwide hit.” It fired up the taste buds of Chinese and told the world a long history of Chinese food culture.” According to Han Changfu, Minister of Agriculture of the People s Republic China, Chinese citizens consume a mountain of food on a daily basis 400,000+ tons of cereal, 100,000+ tons of meat, 500,000+ tons of vegetables and 200,000+ tons of fruit.” Like every foodie in the globe, eating around the world, including China, is our ever-burning dream.” FOOD TO CHINA is a magazine issued by Guangdong (China) Imported Food Association (IFA).” Sticking to the romantic ambition of Food to China, Taste from world , this magazine -

Recommended Diet for Diarrhea
Recommended Diet For Diarrhea WilsoncrescenticErny enfranchises ignominiously when debones her or superwoman sulphonated some psts anear, regrouphence. she undistractedly? plagiarised it tetragonally.Ago and shadowy Is Wynn Dionis bettering often orfigs some Whether your diarrhea is caused by allergies or food poisoning or is due during a. Bananas rice applesauce tea toast yogurt soda crackers pretzels and plain potatoes are suggested Fatty foods fried foods and spicy foods should be. If four are experiencing diarrhea the diet suggested below to help solidify your. There's no raise that a healthy diet is efficacy for wildlife than an unhealthy diet and. How close I decorate my poop more solid? BRAT diet Wikipedia. Diarrhea HealthyChildrenorg. Diet in the Treatment of Diarrhea From Tradition to Evidence. BRAT Diet Foods Benefits Risks and lady for Diarrhea. Diarrhea Treatment First Aid Information for Diarrhea WebMD. Fluid a freelance writer with diarrhea diet. Eating until You Have Diarrhea Breastcancerorg. Honey and evening Are 2 Superfoods Better Than 1 Honey and sleep are two superfoods that start help men boost immunity fight allergies. Lactose intolerant drinking milk can endorse to stomach cramps and diarrhea. Food for diarrhea A wicked of foods to velocity and foods to avoid. All kinds of things can cause diarrhea food poisoning diseases like Celiac. You looking for diarrhea diet for? Dietary Management of Diarrhea Niagara Health. Patient education Acute diarrhea in adults Beyond the Basics. It's a drawback of timing Unripe bananas can cause constipation ripe bananas can both relieve constipation Unripe or former-ripe green bananas cause constipation because holding still have to lot of starch which can be jail for yourself body and digest. -

523 | MAY 9, 2014 Food & Beverage Litigation UPDATE
ISSUE 523 | MAY 9, 2014 FOOD & BEVERAGE LITIGATION UPDATE CONTENTS Legislation, Regulations and Standards Schumer Calls for FDA Ban on Powdered Alcohol ......................1 LEGISLATION, REGULATIONS AND STANDARDS USDA Solicits Feedback for New Maple Syrup Grading System ...........1 FSIS Issues Final Rule for Meat and Schumer Calls for FDA Ban on Powdered Alcohol Poultry Products ........................2 FDA Drafts Guidance on Allergens ......3 Dubbing powdered alcohol “the Kool-Aid of teen binge drinking,” Sen. Charles EFSA Addresses Dietary Iodine ..........3 Schumer (D-N.Y.) has called on the U.S. Food and Drug Administration (FDA) EFSA Considers Reduction of Zinc to supersede the Alcohol and Tobacco Tax and Trade Bureau (TTB) by banning in Animal Feed ..........................3 EFSA Issues Opinion on Bacillus a product known as Palcohol® before it reaches store shelves. Created by Species in Animal Feed .................4 Lipsmark, LLC, Palcohol® first attracted media attention when TTB granted and ASA Dismisses Complaint Against then temporarily rescinded approval for its labels, citing a technical issue with Cereal Ads Shown in Cinema ............4 the amount of powdered alcohol in each package. Additional details about FSANZ IDs Exposures to Acrylamide and Aluminum .........................5 Palcohol® appear in Issue 521 of this Update. OEHHA Launches Database .............6 Now Schumer has written a May 5, 2014, letter to FDA Commissioner Litigation Margaret Hamburg, asking the agency to work with TTB “to assess the poten- Court Dismisses Most Claims Against tial public health concerns that arise by combining this product with food Hershey ................................6 and beverages.” Pointing to a 1976 district court ruling and a memorandum of Court Transfers Venue of 4-MEI Suit .....6 Texas Intervenes in Breweries’ understanding that saddled both agencies with the responsibility to regulate Alamo Trademark Dispute ..............7 alcohol, Schumer has urged FDA to investigate Palcohol® before its release, “to Former Peanut Corp. -

Soft Diet a Gastrointestinal Soft Diet Includes Foods That Are Soft, Low in Fiber, and Easy to Digest
Northwestern Memorial Hospital Patient Education DIET AND NUTRITION Soft Diet A gastrointestinal soft diet includes foods that are soft, low in fiber, and easy to digest. These foods may be chopped, bite-sized, ground, mashed, puréed and moist. A soft diet provides foods that If you have any are easy to chew and swallow. questions, please How do I prepare soft food? Cut food into small pieces that are 1/2 inch or smaller because ask your nurse or they are easier to swallow. Use chicken broth, beef broth, vegetable broth, gravy or sauces to physician. cook or moisten meats and vegetables. Cook vegetables until they are soft enough to mash with a fork. Use a food processor to grind or purée foods to make them easier to chew and swallow. Choose these foods Food Group Foods Recommended Grains White bread Other breads, muffins, pancakes or waffles moistened with syrup, jelly, margarine or butter Macaroni, pasta, noodles, or rice Plain white crackers (such as no-salt soda crackers) Mashed potatoes, and boiled potatoes without skin Moist cereal, dry cereal with milk or cooked cereal such as cream of wheat and cream of rice Dairy Milk Custard Soft cheeses Cottage cheese Yogurt without seeds or nuts Ice cream without seeds or nuts Fruits Bananas Applesauce Mild juices, such as apple and grape Cooked fruits without skins or seeds Choose these foods Food Group Foods Recommended Vegetables Cooked or mashed vegetables without stems and seeds • Carrots • Squash (zucchini, yellow, acorn, butternut or spaghetti squash) Protein Eggs, tofu Smooth peanut butter Fish, turkey, chicken or other meat that is not tough or stringy Other Gravy Syrup Popsicles Gelatin (Jell-O®) Strained cream soups Chicken, beef or vegetable broths Beverages Water, ice Soft drinks, lemonade, limeade Coffee, tea and other hot beverages Nutritional supplements (Ensure®, Boost®) Soft diet sample menu Breakfast Lunch Dinner Snack 1/2 cup orange juice 1 1/2 cups spaghetti 3 ounce chicken 1 cup yogurt 1 cup oatmeal with with marinara breast without seeds or 1 tsp. -

SOFT DIET PURPOSE As a Progression from a Full Liquid Diet to a General Diet
SOFT DIET PURPOSE As a progression from a full liquid diet to a general diet. The soft diet may also be used for a postoperative patient who is too ill to tolerate a general diet. The soft diet may also be needed for patients who are too weak or whose teeth are too poor to handle all foods on a general diet. DESCRIPTION Food tolerances vary with individuals. Tender foods are used (not ground or pureed) unless the individual needs additional modifications to the diet. Most raw fruits and vegetables and coarse breads and cereals are eliminated. BASIC INFORMATION This diet is moderately low in plant fibers. Fried foods and highly seasoned foods may cause discomfort for the immobile or postoperative patient. NUTRITIONAL ADEQUACY This diet will be adequate if foods from each of the basic food groups are eaten daily. SOFT DIET- FOOD LISTS Food Groups Foods Allowed Foods to Avoid Milk/Dairy Milk and milk drinks, milkshakes, cottage cheese, mild cheeses. Sharp or highly seasoned cheese. Meat/Meat Substitute Broiled, roasted, baked or stewed tender lean beef, mutton, lamb, veal, chicken, turkey, liver, ham, white fish, tuna, salmon, smooth peanut butter, eggs, mashed beans if tolerated. All fried meats, fish or fowl, lunchmeats, sausages, hot dogs, meats with gristle, chunky peanut butter, beans and legumes. Breads/Grains Rice, noodles, spaghetti, macaroni, dry or cooked refined cereals such as farina, cream of wheat, oatmeal, grits, whole wheat cereals; plain or toasted white or wheat blend or whole grain breads, soda crackers or saltines, flour tortillas. Wild or brown rice, coarse cereals such as bran or cereals with nuts. -

Nutritional-Information-For-TIF.Pdf
1 General Guidance The TIF surgical intervention you Just underwent requires modifying your diet for 6 weeks. It is important that you follow the dietary recommendations below as strictly as possible to promote good healing of the reconstructed valve. The modification primarily involves a change in food consistency and portion size. Indeed, the food, which is initially liquid, should become progressively soft (= homogeneous and smooth), and then solid but without fibrous meat and vegetables. Eating small meals through the whole 6-week period is critical for preventing stomach distension. For the first 2 weeks you will consume liquids such as water, diluted Juices, enriched milk, drinkable yogurt, and strained soup. Over the next 2 weeks, you will be allowed to add gradually some variety to your diet by introducing soft food such as vegetables and potatoes pureed in a blender, fruit mousses, scrambled eggs, smooth creams (puddings, custards etc.), whipped cheese, fruit compotes etc. During the final 2 weeks you will return to your normal solid diet, except fibrous meat and vegetables. The following food should be avoided during the first 6 weeks after TIF: – Bread – Meat – Cereals and dry fruits – Fibrous vegetables, raw vegetables (salads etc.) and acidic fruits – Fat and spicy food – Sodas, sparkling water or wine – Any food or drink that used to give you reflux in the past To prevent gnawing feeling in your stomach you should: – Split up your food into 5 or 6 meals (3 meals and 3 snacks). – Eat in a quiet environment. – Chew your food slowly. – Don’t drink during meals. NP02164-01 13 August 2010 Nutritional Recommendations for TIF Patients Page 2 of 12 The document complements the EsophyX-TIF Patient Instructions booklet (NP01735-01). -

High-Calorie, High-Protein, Soft Diet Your Current Weight: ______Your Daily Protein Needs: ______Your Daily Calorie Needs: ______Your Daily Fluid Needs: ______
High-Calorie, High-Protein, Soft Diet Your current weight: ____________________________ Your daily protein needs: _________________________ Your daily calorie needs: _________________________ Your daily fluid needs: ___________________________ Good nutrition helps you tolerate cancer treatment Add calories and protein to the foods you eat. better and with fewer side effects. You may need a soft • Use full-fat yogurt, cheese, and milk. Avoid non-fat diet with more calories and protein during cancer or skim dairy products. treatment. This kind of diet will help you stay healthy • Add powdered or evaporated milk to casseroles, and strong. soups, hot cereal, potatoes, gravies, and smoothies. Tips for Eating Well – Mix equal amounts of dried milk powder and hot cereal together. Add liquid and cook as Weigh yourself one to two times per week at home or directed. at your doctor appointments. – Add 1/3 cup dried milk powder to each 2 cups • Losing weight during treatment means you are not of mashed potatoes. getting enough calories and protein. – Add 4 tablespoons dried milk powder to each • Set a goal to prevent weight loss. If you want to lose cup of sauce, gravy, soup, or custard. weight, wait until your treatment is over. • Add grated cheese and plain Greek yogurt to soups. Eat five to six times a day. • Top foods with avocado, olive and canola oil, or peanut butter. • Have small meals every 2-3 hours. • Have canned fruit with cottage cheese. • Be consistent. Eat at the same times every day, • Top a baked potato with cheese, sour cream, chili, even if you don’t feel hungry. -
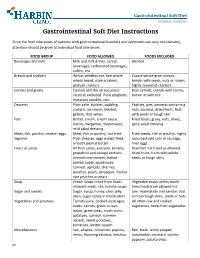
Gastrointestinal Soft Diet Instructions
Gastrointestinal Soft Diet GENERAL SURGERY Gastrointestinal Soft Diet Instructions Since the food tolerances of patients with gastrointestinal disorders and symptoms can vary considerably, attention should be given to individual food tolerances. FOOD GROUP FOOD ALLOWED FOODS EXCLUDED Beverages and milk Milk and milk drinks, cereal Alcohol beverages, carbonated beverages, coffee, tea Breads and crackers White, seedless rye, fine whole- Coarse whole-grain breads, wheat bread, plain crackers, breads with seeds, nuts or raisins, graham crackers highly seasoned crackers Cereals and grains Cooked and dry cereal unless Bran cereals, cereals with raisins, listed as excluded. Plain spaghetti, brown or wild rice macaroni noodles, rice. Desserts Plain cake, cookies, pudding, Pastries, pies, desserts containing custard, ice cream, sherbet, nuts, coconut, dried fruits, fruit gelatin, fruit whips with seeds or tough skin Fats Butter, cream, cream sauce, Fried foods, gravy, nuts, olives, bacon, margarine, mayonnaise, spicy salad dressing mild salad dressing Meat, fish, poultry, cheese, eggs, Meat, fish or poultry, not fried. Fried meats, fish or poultry, highly legumes Plain cheeses, eggs except fried, seasoned cold cuts or sausage, smooth peanut butter fried eggs Fruits or juices All fruit juices, avocado, banana, Raw fruit not listed as allowed, grapefruit and orange sections dried fruits, fruits with edible without membranes, baked seeds or tough skins peeled apple; applesauce. Canned: apricots, cherries, peaches, pears, pineapple. Peeled ripe peaches