Combination of Entecavir Or Tenofovir with Pegylated Interferon
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Interbiotech Entecavir
InterBioTech FT-XLS250 Entecavir Product Description Catalog #: XLS250, 5mg XLS251, 10mg XLS252, 50mg XLS253, 100mg AXAIV0, 1ml 10mM in DMSO. Catalog #: Name: Entecavir, Monohydrate Syn: BMS200475 monohydrate; SQ34676 monohydrate CAS : 209216-23-9 MW : 295.29 Formula : C12H17N5O4 Properties : DMSO : ≥ 50 mg/mL (169.33 mM) H2O : 2.8 mg/mL (9.48 mM) >99.5% Storage: Powder: -20°C (long term; possible at +4°C (2 years) (M) Also available: In solvent: -80°C (6 months) -20°C (1 month) Entecavir free form #RO893P/Q/R (Syn.: BMS200475; SQ34676) CAS No. : 142217-69-4; MW: 277.2 For Research Use Only Introduction Entecavir monohydrate (BMS200475 monohydrate; SQ34676 monohydrate) is a potent and selective inhibitor of HBV, with an EC50 of 3.75 nM in HepG2 cell. IC50 & Target EC50:3.75 nM (anti-HBV, HepG2 cell)[1] In Vitro *Solubility : DMSO : ≥ 50 mg/mL (169.33 mM) H2O : 2.8 mg/mL (9.48 mM; Need ultrasonic and warming) *Preparation : 1mM = 1mg in 3.3865 mL Entecavir monohydrate (BMS200475 monohydrate; SQ34676 monohydrate) has a EC50 of 3.75 nM against HBV. It is incorporated into the protein primer of HBV and subsequently inhibits the priming step of the reverse transcriptase. The antiviral activity of BMS-200475 is significantly less against the other RNA and DNA viruses[1]. Entecavir monohydrate is more readily phosphorylated to its active metabolites than other deoxyguanosine analogs (penciclovir, ganciclovir, lobucavir, and aciclovir) or lamivudine. The intracellular half-life of entecavir is 15 h[2]. P.1 InterBioTech FT-XLS250 In Vivo *Preparation : 1. Add each solvent one by one: 10% DMSO 40% PEG300 5% Tween-80 45% saline Solubility: ≥ 3 mg/mL (10.16 mM); Clear solution 2. -

COVID-19) Pandemic on National Antimicrobial Consumption in Jordan
antibiotics Article An Assessment of the Impact of Coronavirus Disease (COVID-19) Pandemic on National Antimicrobial Consumption in Jordan Sayer Al-Azzam 1, Nizar Mahmoud Mhaidat 1, Hayaa A. Banat 2, Mohammad Alfaour 2, Dana Samih Ahmad 2, Arno Muller 3, Adi Al-Nuseirat 4 , Elizabeth A. Lattyak 5, Barbara R. Conway 6,7 and Mamoon A. Aldeyab 6,* 1 Clinical Pharmacy Department, Jordan University of Science and Technology, Irbid 22110, Jordan; [email protected] (S.A.-A.); [email protected] (N.M.M.) 2 Jordan Food and Drug Administration (JFDA), Amman 11181, Jordan; [email protected] (H.A.B.); [email protected] (M.A.); [email protected] (D.S.A.) 3 Antimicrobial Resistance Division, World Health Organization, Avenue Appia 20, 1211 Geneva, Switzerland; [email protected] 4 World Health Organization Regional Office for the Eastern Mediterranean, Cairo 11371, Egypt; [email protected] 5 Scientific Computing Associates Corp., River Forest, IL 60305, USA; [email protected] 6 Department of Pharmacy, School of Applied Sciences, University of Huddersfield, Huddersfield HD1 3DH, UK; [email protected] 7 Institute of Skin Integrity and Infection Prevention, University of Huddersfield, Huddersfield HD1 3DH, UK * Correspondence: [email protected] Citation: Al-Azzam, S.; Mhaidat, N.M.; Banat, H.A.; Alfaour, M.; Abstract: Coronavirus disease 2019 (COVID-19) has overlapping clinical characteristics with bacterial Ahmad, D.S.; Muller, A.; Al-Nuseirat, respiratory tract infection, leading to the prescription of potentially unnecessary antibiotics. This A.; Lattyak, E.A.; Conway, B.R.; study aimed at measuring changes and patterns of national antimicrobial use for one year preceding Aldeyab, M.A. -

Recommended Comparator Products: Medicines for Hepatitis B and C
Guidance Document WHO/PQT: medicines 10 December 2019 Recommended comparator products: Medicines for Hepatitis B and C Comparator products should be purchased from a well regulated market with stringent regulatory authority1. Recommended comparator product Invited medicinal products (Strength, Manufacturer) Hepatitis C Single Ingredient Daclatasvir tablet, 60mg, 30mg Daclatasvir 30 mg and 60 mg tablet, Mylan Laboratories Ltd3 Dasabuvir tablet, 250mg Exviera 250 mg tablet, AbbVie Inc. Viekirax copackaged, 250 mg tablet (+12.5mg/75mg/50mg tablet), AbbVie Inc. Ledipasvir tablet, 90mg No comparator available Ribavirin capsule, 200mg, 400mg, 600 mg Rebetol, 200 mg capsule, MSD Ribavirin syrup, 40mg/ml (oral) Rebetol solution, 40mg/ml, MSD Sofosbuvir tablet 400mg Sovaldi, 400 mg tablet, Gilead Sciences Velpatasvir tablet, 100mg No comparator available Fixed-dose combination (FDC) Ombitasvir/Paritaprevir/Ritonavir, tablet Viekirax, 12.5mg/75mg/50mg tablet, AbbVie Inc. 12.5mg/75mg/50mg, 25mg/150mg/100mg Technivie, 12.5mg/75mg/50mg tablet, AbbVie Inc., US2 Sofosbuvir/ Daclatasvir, tablet 400mg/30mg The individual comparators should be used. Sofosbuvir/ Daclatasvir, tablet 400mg/60mg The individual comparators should be used. 1 A regulatory authority that is: a) a member of ICH prior to 23 October 2015, namely: the US Food and Drug Administration, the European Commission and the Ministry of Health, Labour and Welfare of Japan also represented by the Pharmaceuticals and Medical Devices Agency; or b) an ICH observer prior to 23 October 2015, namely: the European Free Trade Association, as represented by Swissmedic and Health Canada; or c) a regulatory authority associated with an ICH member through a legally-binding, mutual recognition agreement prior to 23 October 2015, namely: Australia, Iceland, Liechtenstein and Norway. -

Tenofovir Alafenamide Rescues Renal Tubules in Patients with Chronic Hepatitis B
life Communication Tenofovir Alafenamide Rescues Renal Tubules in Patients with Chronic Hepatitis B Tomoya Sano * , Takumi Kawaguchi , Tatsuya Ide, Keisuke Amano, Reiichiro Kuwahara, Teruko Arinaga-Hino and Takuji Torimura Division of Gastroenterology, Department of Medicine, Kurume University School of Medicine, Kurume, Fukuoka 830-0011, Japan; [email protected] (T.K.); [email protected] (T.I.); [email protected] (K.A.); [email protected] (R.K.); [email protected] (T.A.-H.); [email protected] (T.T.) * Correspondence: [email protected]; Tel.: +81-942-31-7627 Abstract: Nucles(t)ide analogs (NAs) are effective for chronic hepatitis B (CHB). NAs suppress hepatic decompensation and hepatocarcinogenesis, leading to a dramatic improvement of the natural course of patients with CHB. However, renal dysfunction is becoming an important issue for the management of CHB. Renal dysfunction develops in patients with the long-term treatment of NAs including adefovir dipivoxil and tenofovir disoproxil fumarate. Recently, several studies have reported that the newly approved tenofovir alafenamide (TAF) has a safe profile for the kidney due to greater plasma stability. In this mini-review, we discuss the effectiveness of switching to TAF for NAs-related renal tubular dysfunction in patients with CHB. Keywords: adefovir dipivoxil (ADV); Fanconi syndrome; hepatitis B virus (HBV); renal tubular Citation: Sano, T.; Kawaguchi, T.; dysfunction; tenofovir alafenamide (TAF); tenofovir disoproxil fumarate (TDF); β2-microglobulin Ide, T.; Amano, K.; Kuwahara, R.; Arinaga-Hino, T.; Torimura, T. Tenofovir Alafenamide Rescues Renal Tubules in Patients with Chronic 1. -

Interplay Between Hepatitis D Virus and the Interferon Response
viruses Review Interplay between Hepatitis D Virus and the Interferon Response Zhenfeng Zhang 1 and Stephan Urban 1,2,* 1 Department of Infectious Diseases, Molecular Virology, University Hospital Heidelberg, 69120 Heidelberg, Germany; [email protected] 2 German Centre for Infection Research (DZIF), Partner Site Heidelberg, 69120 Heidelberg, Germany * Correspondence: [email protected]; Tel.: +49-6221-564-902 Received: 27 October 2020; Accepted: 18 November 2020; Published: 20 November 2020 Abstract: Chronic hepatitis D (CHD) is the most severe form of viral hepatitis, with rapid progression of liver-related diseases and high rates of development of hepatocellular carcinoma. The causative agent, hepatitis D virus (HDV), contains a small (approximately 1.7 kb) highly self-pairing single-strand circular RNA genome that assembles with the HDV antigen to form a ribonucleoprotein (RNP) complex. HDV depends on hepatitis B virus (HBV) envelope proteins for envelopment and de novo hepatocyte entry; however, its intracellular RNA replication is autonomous. In addition, HDV can amplify HBV independently through cell division. Cellular innate immune responses, mainly interferon (IFN) response, are crucial for controlling invading viruses, while viruses counteract these responses to favor their propagation. In contrast to HBV, HDV activates profound IFN response through the melanoma differentiation antigen 5 (MDA5) pathway. This cellular response efficiently suppresses cell-division-mediated HDV spread and, to some extent, early stages of HDV de novo infection, but only marginally impairs RNA replication in resting hepatocytes. In this review, we summarize the current knowledge on HDV structure, replication, and persistence and subsequently focus on the interplay between HDV and IFN response, including IFN activation, sensing, antiviral effects, and viral countermeasures. -

Estimating the Long-Term Clinical and Economic Outcomes of Daclatasvir
VALUE IN HEALTH REGIONAL ISSUES ] ( ]]]]) ]]]– ]]] Available online at www.sciencedirect.com journal homepage: www.elsevier.com/locate/vhri Estimating the Long-Term Clinical and Economic Outcomes of Daclatasvir Plus Asunaprevir in Difficult-to-Treat Japanese Patients Chronically Infected with Hepatitis C Genotype 1b Phil McEwan, PhD1,2, Thomas Ward, MSc1,*, Samantha Webster, BSc1, Yong Yuan, PhD3, Anupama Kalsekar, MS3, Kristine Broglio, MS4, Isao Kamae, PhD5, Melanie Quintana, PhD4, Scott M. Berry, PhD4, Masahiro Kobayashi, MD6, Sachie Inoue, PhD7, Ann Tang, PhD8, Hiromitsu Kumada, MD6 1Health Economics and Outcomes Research Ltd., Monmouth, UK; 2Centre for Health Economics, Swansea University, Swansea, UK; 3Global Health Economics and Outcomes Research, Princeton, NJ, USA; 4Berry Consultants, LLC, Austin, TX, USA; 5Graduate School of Public Policy, University of Tokyo, Tokyo, Japan; 6Department of Hepatology, Toranomon Hospital, Tokyo, Japan; 7CRECON Research and Consulting, Inc., Tokyo, Japan; 8Health Economics and Outcomes Research, Bristol-Myers K.K., Tokyo, Japan ABSTRACT Objectives: Japan has one of the highest endemic rates of hepatitis C treated with TVR þ pegIFN-α/RBV. Results: Initiating DCV þ ASV virus (HCV) infection. Treatments in Japan are currently limited to treatment in patients in the chronic hepatitis C disease stage resulted interferon-alfa–based regimens, which are associated with tolerability in quality-adjusted life-year gains of 0.96 and 0.77 over TVR þ pegIFN- and efficacy issues. A novel regimen combining two oral HCV α/RBV for NRs and PRs, respectively, and a gain of 2.61 in interferon- therapies, daclatasvir and asunaprevir (DCV þ ASV), has shown alfa–ineligible/intolerant patients over no treatment. -

Rash with Entecavir - Case Report Xiong Khee Cheong1, Zhiqin Wong2*, Norazirah Md Nor3 and Bang Rom Lee4
Cheong et al. BMC Gastroenterology (2020) 20:305 https://doi.org/10.1186/s12876-020-01452-3 CASE REPORT Open Access “Black box warning” rash with entecavir - case report Xiong Khee Cheong1, Zhiqin Wong2*, Norazirah Md Nor3 and Bang Rom Lee4 Abstract Background: Hepatitis B infection is a significant worldwide health issue, predispose to the development of liver cirrhosis and hepatocellular carcinoma. Entecavir is a potent oral antiviral agent of high genetic barrier for the treatment of chronic hepatitis B infection. Cutaneous adverse reaction associated with entecavir has rarely been reported in literature. As our knowledge, this case was the first case reported on entecavir induced lichenoid drug eruption. Case presentation: 55 year old gentlemen presented with generalised pruritic erythematous rash on trunk and extremities. Six weeks prior to his consultation, antiviral agent entecavir was commenced for his chronic hepatitis B infection. Skin biopsy revealed acanthosis and focal lymphocytes with moderate perivascular lymphocyte infiltration. Skin condition recovered completely after caesation of offending drug and short course of oral corticosteroids. Conclusion: This case highlight the awareness of clinicians on the spectrum of cutaneous drug reaction related to entecavir therapy. Keywords: Drug eruption, Entecavir, Hepatitis B Background Case presentation Hepatitis B infection is a global health issue, contribut- A 55 years old gentlemen, background of chronic ing to approximately 887,000 deaths in 2015 due to he- hepatitis B (treatment naïve), was referred for 2 patocellular carcinoma and liver cirrhosis [1, 2]. weeks of generalised itchy erythematous rash. His Entecavir is a nucleoside analogue reverse transcriptase other medical illnesses were ischemic heart disease, inhibitor that is widely used in the treatment of chronic chronic kidney disease stage 3, diabetes mellitus and hepatitis B (HBV) infection. -

Information for the User Valganciclovir <Invented Name>
Package Leaflet: Information for the user Valganciclovir <Invented Name> 450 mg film-coated tablets Valganciclovir Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. Keep this leaflet. You may need to read it again. If you have any further questions, ask your doctor or pharmacist. This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Valganciclovir <Invented Name> is and what it is used for 2. What you need to know before you take Valganciclovir <Invented Name> 3. How to take Valganciclovir <Invented Name> 4. Possible side effects 5. How to store Valganciclovir <Invented Name> 6. Contents of the pack and other information 1. What Valganciclovir <Invented Name> is and what it is used for Valganciclovir <Invented Name> belongs to a group of medicines, which work directly to prevent the growth of viruses. In the body the active ingredient in the tablets, valganciclovir, is changed into ganciclovir. Ganciclovir prevents a virus called cytomegalovirus (CMV) from multiplying and invading healthy cells. In patients with a weakened immune system, CMV can cause an infection in the body’s organs. This can be life threatening. Valganciclovir <Invented Name> is used: for treatment of CMV-infections of the retina of the eye in patients with acquired immunodeficiency syndrome (AIDS). -
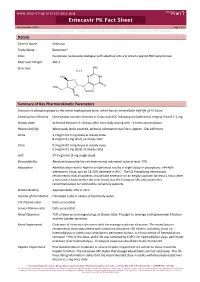
Entecavir PK Fact Sheet Reviewed March 2016 Page 1 of 2 for Personal Use Only
www.hep-druginteractions.org Entecavir PK Fact Sheet Reviewed March 2016 Page 1 of 2 For personal use only. Not for distribution. For personal use only. Not for distribution. For personal use only. Not for distribution. Details Generic Name Entecavir Trade Name Baraclude® Class Guanosine nucleoside analogue with selective antiviral activity against HBV polymerase Molecular Weight 295.3 Structure NH2 H2O HO NNH O HO N N CH2 Summary of Key Pharmacokinetic Parameters Entecavir is phosphorylated to the active triphosphate form, which has an intracellular half‐life of 15 hours. Linearity/non‐linearity Dose‐proportionate increases in Cmax and AUC following multiple doses ranging from 0.1‐1 mg. Steady state Achieved between 6‐10 days after once daily dosing with ~2 times accumulation. Plasma half life When peak levels reached, terminal elimination half life is approx. 128‐149 hours. Cmax 4.2 ng/ml (0.5 mg dose) at steady state 8.2 ng/ml (1 mg dose) at steady state Cmin 0.3 ng/ml (0.5 mg dose) at steady state 0.5 ng/ml (1 mg dose) at steady state AUC 27.9 ng.h/ml (1 mg single dose) Bioavailability Absolute bioavailability not determined; estimated to be at least 70%. Absorption Administration with a high fat or light meal results in slight delay in absorption; a 44‐46% decrease in Cmax, and an 18‐20% decrease in AUC. The US Prescribing Information recommends that all patients should take entecavir on an empty stomach (at least 2 hours after a meal and 2 hours before the next meal), but the European SPC only makes this recommendation for lamivudine‐refractory patients. -

Anogenital Warts) Contain Accumulations of HIV-1 Target Cells That May Provide Portals for HIV Transmission Jeffrey Pudney, Zoon Wangu, Lori Panther, Et Al
Journal Club: Journal of Infectious Diseases 13th Feb, 2019 Dr Alisa Pollack, SSHC HIV Hepatitis HPV Herpes Substantial Decline in Prevalence of Vaccine-Type and Nonvaccine-Type Human Papillomavirus (HPV) in Vaccinated and Unvaccinated Girls Berit Feiring, Ida Laake, Irene Kraus Christiansen, et al. What?: Estimation of the impact of quadrivalent HPV vaccination in Norway Why?: This is the first analysis of a population where there was no catch-up vaccination for older girls/women (only 12 year olds were vaccinated) How?: 17,749 17yo girls submitted urine samples (in return for 2 movie tickets) - Approximately two thirds were unvaccinated (born 1994 and 1996), and one third were the first vaccinated cohort (born 1997) - Tested by PCR for 37 HPV genotypes (incl low and high risk types) Substantial Decline in Prevalence of Vaccine-Type and Nonvaccine-Type Human Papillomavirus (HPV) in Vaccinated and Unvaccinated Girls Berit Feiring, Ida Laake, Irene Kraus Christiansen, et al. Results: Vaccination works. Condylomata Acuminata (Anogenital Warts) Contain Accumulations of HIV-1 Target Cells That May Provide Portals for HIV Transmission Jeffrey Pudney, Zoon Wangu, Lori Panther, et al. What?: 1. Examination for HIV target cells in anogenital warts compared to anatomically matched control skin samples 2. Pilot study of in vitro HIV infection of anogenital warts versus control skin Why?: A number of recent studies have shown an increased risk of HIV acquisition in individuals with anogenital warts but the mechanisms are unclear. How?: 1. Archived samples of biopsied warts from 91 subjects were examined for HIV target cells (CD1a dendritic cells, CD4 T lymphocytes, CD68 macrophages). -

S Sofosbuvir (Sovaldi )
Sofosbuvir (Sovaldi ™) UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Nucleotide Analog NS5B Polymerase Inhibitor BRAND (generic) NAME: Sovaldi (sofosbuvir ) 400 mg strength tablet FDA -APPROVED INDICATIONS Sovaldi is a hepatitis C virus (HCV) nucleotide analog NS5B polymerase inhibitor indicated for the treatment of chronic hepatitis C (CHC) infection as a component of a combination antiviral treatment regimen. • Sovaldi efficacy has been established in subjects with HCV genotype 1, 2, 3 or 4 infection, including those with hepatocellular carcinoma meeting Milan criteria (awaiting liver transplantation) and those with HCV/HIV -1 co-infection. COVERAGE AUTHORIZATION CRITE RIA Sofosbuvir (Sovaldi) is cover ed for the following condition and situations: • Diagnosis of chronic hepatitis C (CHC) infection with c onfirmed genotype 1, 2, 3, or 4, OR • CHC infection with hepatocellular carcinoma awaiting liver transplant, AND • Sofosbuvir is prescribed in combination with ribavirin and pegylated interferon alfa for genotypes 1 and 4, OR • Sofosbuvir is prescribed in combination with ribavirin for p atients with genotype 1 who are peginterferon-ineligible* (medical record documentation of ineligibility for peginterferon therapy must be submitted for review), OR • Sofosbuvir is prescribed in combination with simeprevir, with or without ribavirin, for 12 weeks duration of therapy, for patients with genotype 1 that have advanced fi brosis (METAVIR score 2, 3, 4, OR cirrhosis secondary to Hepatitis C ), and are peginterferon - ineligible* (medical record -

Pegasys®) Peginterferon Alfa-2B (Peg-Intron®
Peginterferon alfa-2a (Pegasys®) Peginterferon alfa-2b (Peg-Intron®) UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Pegylated Interferons BRAND (generic) NAME: Pegasys (peginterferon alfa-2a) Single-use vial 180 mcg/1.0 mL; Prefilled syringe 180 mcg/0.5 mL Peg-Intron (peginterferon alfa-2b) Single-use vial (with 1.25 mL diluent) and REDIPEN®: 50 mcg, 80 mcg, 120 mcg, 150 mcg per 0.5 mL. FDA-APPROVED INDICATIONS PEG-Intron (peginterferon alfa-2b): Combination therapy with ribavirin: • Chronic Hepatitis C (CHC) in patients 3 years of age and older with compensated liver disease. • Patients with the following characteristics are less likely to benefit from re-treatment after failing a course of therapy: previous nonresponse, previous pegylated interferon treatment, significant bridging fibrosis or cirrhosis, and genotype 1 infection. Monotherapy: CHC in patients (18 years of age and older) with compensated liver disease previously untreated with interferon alpha. Pegasys (Peginterferon alfa-2a): • Treatment of Chronic Hepatitis C (CHC) in adults with compensated liver disease not previously treated with interferon alpha, in patients with histological evidence of cirrhosis and compensated liver disease, and in adults with CHC/HIV coinfection and CD4 count > 100 cells/mm3. o Combination therapy with ribavirin is recommended unless patient has contraindication to or significant intolerance to ribavirin. Pegasys monotherapy is indicated for: • Treatment of adult patients with HBeAg positive and HBeAg negative chronic hepatitis B who have compensated