Describing Patient Populations for the My Health Team Initiative
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

May 5, 2021 COVID-19 VACCINE BULLETIN #74 Eligibility to Be
May 5, 2021 COVID-19 VACCINE BULLETIN #74 Eligibility to be immunized at a super site or pop-up clinic has been expanded to include individuals aged 45 or older and Indigenous people aged 18 and older. Manitoba expects that eligibility will expand to include all people aged 18 or older by May 21. In addition, all adults aged 18 and older who live or work in specified jobs in these priority communities continue to be eligible to make an appointment: • Prairie Mountain Health – Brandon East End and Brandon Downtown; • Winnipeg Regional Health Authority – Inkster West, Fort Garry South, Seven Oaks West, Downtown East, Point Douglas South, Inkster East, Point Douglas North, Downtown West, River East South, St. Vital North and Seven Oaks East; and • Interlake–Eastern Regional Health Authority – Powerview-Pine Falls. All adults who live or work (in any role) in the Northern Regional Health Authority, as well as Churchill, are also eligible. A map and other information about community-based eligibility is available at https://manitoba.ca/covid19/vaccine/eligibility-criteria.html#community-based. Eligibility also includes people aged 18 and older who: • are pregnant; • are a client of Community Living disABILITY Services; • work in any health-care setting including outpatient settings; or • work as a front-line police officer or firefighter. Eligibility for the AstraZeneca/Covishield vaccine includes individuals aged 40 or older and people aged 30 to 39 with priority health conditions. A complete list is available online. Appointments People will be able to begin booking second-dose appointments on May 22. Individuals who are immune-compromised or have other prioritized health conditions will be able to book their appointments first. -

Official Candidates: 42Nd General Election
OFFICIAL CANDIDATES: 42ND GENERAL ELECTION CANDIDATE AFFILIATION OFFICIAL CANDIDATE AFFILIATION OFFICIAL CANDIDATE AFFILIATION OFFICIAL AGENT AGENT AGENT AGASSIZ LAKESIDE ST. BONIFACE CLARKE, Eileen - 54 7TH ST., GLADSTONE PC Jodie Byram EICHLER, Ralph - 40 THIRD STREET S.E., TEULON PC Barry Jeske FORTIER, Simone - 253 LAURA STREET, WINNIPEG MBFWD Ryan Lafreniere CLAYTON, Liz - NW 23-7-8W, MUN. OF NORFOLK-TREHERNE GPM Henri Chatelain REGELSKY, Ilsa - 0132E 81N, ARGYLE Lib. Cecilia Connelly HOSKINS, Megan - 104-15 ARDEN AVE., WINNIPEG PC Darrell Girardin LEGASPI, Kelly - 50 HERRON ROAD, WINNIPEG NDP Kevin Dearing RUGG, Dan - 34 ELIE STREET WEST, ELIE NDP Janice Chase JEANSON, Jaclyn - 42 INMAN AVE, WINNIPEG GPM Luisa Sabourin SWANSON, Hector - 4-355 ISABEL ST., NEEPAWA Lib. Jason Nadeau LAMONT, Dougald - 318 WENTWORTH ST., WINNIPEG Lib. Kevin Gamble LA VÉRENDRYE SIMS, Laurissa - 10 OAKLEIGH PLACE, WINNIPEG NDP Allan Beach ASSINIBOIA MCGEE, Erin - 21072 MUN 50 N, ILE DES CHENES NDP Leo Van Den Bussche ANDERSON, Jeff - 53 LIPTON ST., WINNIPEG Lib. Jane Giesbrecht MITCHELL, Lorena - 92 BEAU SAPIN ST., MARCHAND Lib. Ernesto Torresmalaga ST. JAMES DELAAT, John - 113 LANARK ST., WINNIPEG GPM Durrenda Delaat SMOOK, Dennis - 225 PR 201 E, VITA PC Konrad Narth BUHSE, Jeff - 4B-448 HARGRAVE ST., WINNIPEG GPM Glenda Rempel JOHNSTON, Scott - 107 EMERALD GROVE DR., WINNIPEG PC J. Bryce Matlashewski HOHNE, Bernd - 73 EGESZ STREET, WINNIPEG Lib. Phillip Buckingham MCKELLEP, Joe - 110 TWAIN DR., WINNIPEG NDP Bela Gyarmati MCPHILLIPS RICHARD, Michelle - 38 HOME ST., WINNIPEG PC Justin Zarnowski CACAYURAN, John - 167 NEWTON AVE., WINNIPEG Lib. Michelle Reader SALA, Adrien - 297 MANDEVILLE ST., WINNIPEG NDP Josefino Rarama BORDERLAND MARTIN, Shannon - 42 RIVER HEIGHTS DR., LA SALLE PC Maxine Diamond BRAUL, Loren - 79 ALTBERGTHAL ST., RHINELAND Lib. -

Local Government Chapter Seven
Local Government Chapter Seven Chapter Seven Local Government Counties ....................................................................................................... 386 Metropolitan Council ................................................................................... 430 Regional Development Commissions .......................................................... 430 Cities ............................................................................................................ 431 Townships .................................................................................................... 442 School Districts ............................................................................................ 442 Local Government Chapter Seven Image provided by the Minnesota Historical Society Arch honoring black Civil War troops erected by St. Paul’s African-American community, 1896. The monument was at Summit Avenue and Sixth Street in St. Paul along the parade route for the Grand Army of the Republic gathering. Chapter Seven Local Government COUNTIES IN MINNESOTA When Minnesota officially became a territory in 1849, it followed the lead of other territories to the east and adopted county and township forms of government. This system of local governance was originally derived from England. In October of 1849 the first five counties of the state were established: Benton, Itasca, Ramsey, Wabasha, and Washington. The State of Minnesota has grown from five counties in 1849 to 87 counties today. Ramsey County is the smallest in -

Standing Committee on Justice
Third Session – Forty-Second Legislature of the Legislative Assembly of Manitoba Standing Committee on Justice Chairperson Mr. Andrew Micklefield Constituency of Rossmere Vol. LXXV No. 1 - 5:30 p.m., Monday, November 30, 2020 ISSN 1708-6671 MANITOBA LEGISLATIVE ASSEMBLY Forty-Second Legislature Member Constituency Political Affiliation ADAMS, Danielle Thompson NDP ALTOMARE, Nello Transcona NDP ASAGWARA, Uzoma Union Station NDP BRAR, Diljeet Burrows NDP BUSHIE, Ian Keewatinook NDP CLARKE, Eileen, Hon. Agassiz PC COX, Cathy, Hon. Kildonan-River East PC CULLEN, Cliff, Hon. Spruce Woods PC DRIEDGER, Myrna, Hon. Roblin PC EICHLER, Ralph, Hon. Lakeside PC EWASKO, Wayne Lac du Bonnet PC FIELDING, Scott, Hon. Kirkfield Park PC FONTAINE, Nahanni St. Johns NDP FRIESEN, Cameron, Hon. Morden-Winkler PC GERRARD, Jon, Hon. River Heights Lib. GOERTZEN, Kelvin, Hon. Steinbach PC GORDON, Audrey Southdale PC GUENTER, Josh Borderland PC GUILLEMARD, Sarah, Hon. Fort Richmond PC HELWER, Reg, Hon. Brandon West PC ISLEIFSON, Len Brandon East PC JOHNSON, Derek Interlake-Gimli PC JOHNSTON, Scott Assiniboia PC KINEW, Wab Fort Rouge NDP LAGASSÉ, Bob Dawson Trail PC LAGIMODIERE, Alan Selkirk PC LAMONT, Dougald St. Boniface Lib. LAMOUREUX, Cindy Tyndall Park Lib. LATHLIN, Amanda The Pas-Kameesak NDP LINDSEY, Tom Flin Flon NDP MALOWAY, Jim Elmwood NDP MARCELINO, Malaya Notre Dame NDP MARTIN, Shannon McPhillips PC MICHALESKI, Brad Dauphin PC MICKLEFIELD, Andrew Rossmere PC MORLEY-LECOMTE, Janice Seine River PC MOSES, Jamie St. Vital NDP NAYLOR, Lisa Wolseley NDP NESBITT, Greg Riding Mountain PC PALLISTER, Brian, Hon. Fort Whyte PC PEDERSEN, Blaine, Hon. Midland PC PIWNIUK, Doyle Turtle Mountain PC REYES, Jon Waverley PC SALA, Adrien St. -
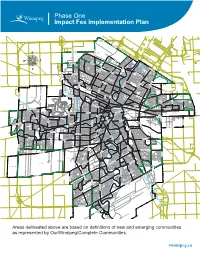
Impact Fee Implementation Plan
Phase One Impact Fee Implementation Plan ROSSER-OLD KILDONAN AMBER TRAILS RIVERBEND LEILA NORTH WEST KILDONAN INDUSTRIAL MANDALAY WEST RIVERGROVE A L L A TEMPLETON-SINCLAIR H L A NORTH INKSTER INDUSTRIAL INKSTER GARDENS THE MAPLES V LEILA-McPHILLIPS TRIANGLE RIVER EAST MARGARET PARK KILDONAN PARK GARDEN CITY SPRINGFIELD NORTH INKSTER INDUSTRIAL PARK TYNDALL PARK JEFFERSON ROSSMERE-A KILDONAN DRIVE KIL-CONA PARK MYNARSKI SEVEN OAKS ROBERTSON McLEOD INDUSTRIAL OAK POINT HIGHWAY BURROWS-KEEWATIN SPRINGFIELD SOUTH NORTH TRANSCONA YARDS SHAUGHNESSY PARK INKSTER-FARADAY ROSSMERE-B BURROWS CENTRAL ST. JOHN'S LUXTON OMAND'S CREEK INDUSTRIAL WESTON SHOPS MUNROE WEST VALLEY GARDENS GRASSIE BROOKLANDS ST. JOHN'S PARK EAGLEMERE WILLIAM WHYTE DUFFERIN WESTON GLENELM GRIFFIN TRANSCONA NORTH SASKATCHEWAN NORTH DUFFERIN INDUSTRIAL CHALMERS MUNROE EAST MEADOWS PACIFIC INDUSTRIAL LORD SELKIRK PARK G N LOGAN-C.P.R. I S S NORTH POINT DOUGLAS TALBOT-GREY O R C PEGUIS N A WEST ALEXANDER N RADISSON O KILDARE-REDONDA D EAST ELMWOOD L CENTENNIAL I ST. JAMES INDUSTRIAL SOUTH POINT DOUGLAS K AIRPORT CHINA TOWN C IVIC CANTERBURY PARK SARGENT PARK CE TYNE-TEES KERN PARK NT VICTORIA WEST RE DANIEL McINTYRE EXCHANGE DISTRICT NORTH ST. BONIFACE REGENT MELROSE CENTRAL PARK SPENCE PORTAGE & MAIN MURRAY INDUSTRIAL PARK E TISSOT LLIC E-E TAG MISSION GARDENS POR TRANSCONA YARDS HERITAGE PARK COLONY SOUTH PORTAGE MISSION INDUSTRIAL THE FORKS DUGALD CRESTVIEW ST. MATTHEWS MINTO CENTRAL ST. BONIFACE BUCHANAN JAMESWOOD POLO PARK BROADWAY-ASSINIBOINE KENSINGTON LEGISLATURE DUFRESNE HOLDEN WEST BROADWAY KING EDWARD STURGEON CREEK BOOTH ASSINIBOIA DOWNS DEER LODGE WOLSELEY RIVER-OSBORNE TRANSCONA SOUTH ROSLYN SILVER HEIGHTS WEST WOLSELEY A NORWOOD EAST STOCK YARDS ST. -

Adult Nuisance Mosquito Fogging Program Starts Tonight
Adult Nuisance Mosquito Fogging Program starts tonight Winnipeg, MB – The City of Winnipeg will start its adult nuisance mosquito fogging program tonight at 9:30 p.m. Crews will treat in Insect Management Areas 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, and 51. This includes the following neighbourhoods: Insect Management Area Neighbourhoods 34 Assiniboia Downs, Buchanan, Kirkfield, Glendale, Westwood 35 Crestview, Heritage Park, Saskatchewan North, Sturgeon Creek Birchwood, Booth, Jameswood, Murray Industrial Park, Silver Heights, 36 Woodhaven 37 Airport 38 Bruce Park, Deer Lodge, King Edward 39 Brooklands, Sargent Park, St. James Industrial 40 Kensington, Minto, Polo Park, St. Matthews, West Wolseley Armstrong Point, Broadway - Assiniboine, Legislature, Portage & Main, 41 South Portage, The Forks, West Broadway, Wolseley Central Park, Colony, Daniel McIntyre, Portage - Ellice, Spence, West 42 Alexander North Inkster Industrial, Oakpoint Highway, Omand's Creek Industrial, 43 Tyndall Park Burrows - Keewatin, Inkster Industrial Park, Mynarski, Pacific Industrial, 44 Shaughnessy Park, Weston, Weston Shops 45 Burrows Central, Robertson, William Whyte Centennial, China Town, Civic Centre, Dufferin, Dufferin Industrial, 46 Exchange District, Logan C.P.R., Lord Selkirk Park, North Point Douglas, South Point Douglas 47 Inkster - Faraday, Luxton, St. John's, St. John's Park 48 Inkster Gardens, Mandalay West, The Maples Garden City, Leila - McPhillips Triangle, Margaret Park, Templeton - 49 Sinclair 50 Jefferson, Kildonan Park, Seven Oaks Amber Trails, Leila North, Riverbend, Rivergrove, Rosser - Old Kildonan, 51 West Kildonan Industrial Fogging will take place until 6:30 a.m. tomorrow. Daily public service announcements Public Service Announcements (PSAs) will be released daily at least eight hours in advance of planned fogging. -

C O M M U N I Q U É
c o m m u n i q u é POUR DIFFUSION IMMÉDIATE Le 23 septembre 2011 Le vote par anticipation commence demain Il y a plus d’occasions de voter par anticipation que jamais auparavant Grâce au nombre accru de centres de scrutin et à une journée additionnelle pour le scrutin par anticipation, il est plus facile que jamais pour les Manitobains et Manitobaines d’exercer leur droit démocratique. Le jour du scrutin au Manitoba est le mardi 4 octobre, mais les Manitobains et Manitobaines peuvent voter par anticipation à partir de demain (le 24 septembre) jusqu’au samedi 1er octobre, une journée de plus qu’aux élections précédentes. Il y a environ 300 centres de scrutin par anticipation dans la province, y compris dans tous les bureaux du directeur du scrutin, ainsi que dans d’autres endroits pratiques comme des centres commerciaux, des campus universitaires et l’aéroport de Winnipeg. Les électeurs admissibles peuvent voter à n’importe quel centre de scrutin par anticipation sans devoir présenter d’explications. Pour être admissible à voter, il faut : • être citoyen canadien; • avoir au moins 18 ans le jour du scrutin; • avoir résidé au Manitoba pendant au moins six mois immédiatement avant le jour du scrutin. Les électeurs doivent présenter une pièce d’identité avec photo délivrée par le gouvernement (ex., un permis de conduire) ou deux autres documents portant leur nom. Il sera également utile d’apporter sa fiche de recensement. Les centres de scrutin par anticipation sont ouverts de 8 h à 20 h tous les jours, sauf le dimanche où ils sont ouverts de 12 h à 18 h. -

41St Legislature
JAMES ALLUM ROB ALTEMEYER KELLY BINDLE KEVIN CHIEF HON. EILEEN CLARKE AMANDA LATH LIN TOM LINDSEY JIMMALOWAY FLOR MARCELINO TED MARCELINO Fort Ga rry-Riverview Wolseley Thompson Point Douglas Agass iz Th e Pas Flin Flon Elmwood Logan Tyndall Park Minister of Indigenous and Northern Relations PATRICIA CHAYCHUK RICK YARISH Clerk Deputy Clerk HON. CATHY COX HON. CLIFF CULLEN NIC CURRY HON. RALPH EICHLER WAYNE EWASKO SHANNON MARTIN HON. COLLEEN MAYER BRAD MICHALES Kl ANDREW MICKLEFIELD JANICE MORLEY-LECOMTE River East Spruce Woods Kildonan Lakeside Lac du Bonnet Morris St. Vital Dauphin Rossmere Seine River Minister of Sport, Minister of Justice Minister of Agriculture Minister of Crown Services Culture and Heritage and Attorney General HON. MYRNA DRIEDGER DAVE SHUTTLEWORTH Speaker of the legislative Assembly BLAKE DUNN Sergeant-at-A rms Sergeant-at-Arms HON. SCOTT FIELDING HON. STEVEN FLETCHER NAHANNI FONTAINE HON. CAMERON FRIESEN GREG NESBITT HON. BLAINE PEDERSEN DOYLE PIWNIUK JON REYES Kirkfield Park Ass iniboia St. Johns Mord en-Winkler Riding Mountain Midland Arthur-Virden St. Norbert Minister of Finance Minister of Health, Minister of Growth, Seniors and Active Living Enterprise and Trade MONIQUE GRENIER CLAUDE MICHAUD TIM ABBOTT GREG RECKSIEDLER ANDREA SIGNORELLI Clerk Ass istant Clerk Assistant Clerk Assistant Clerk Assistant Clerk Assistant Clerk of Commrttees Journals Clerk Clerk of Committees Research Officer Clerk of Committees Journals Assistant ~ ~ §!;;?fdOUoe ~~ (j/S1f:Jnffflk 2016-2019 HON. JON GERRARD HON. KELVIN GOERTZEN CLIFF GRAYDON SARAH GUILLEMARD MOHINDER SARAN HON. RON SCHULER GREG SELINGER ANDREW SMITH BERNADETTE SMITH River Heights Steinbach Emerson Fort Richmond The Maples St. Paul St. Boniface Southdale Po int Douglas M inister of Education M inister of Infrastructure an d Training REG HELWER LEN ISLEIFSON DEREK JOHNSON SCOTT JOHNSTON WABKINEW DENNIS SMOOK HON. -

ORGANIZATIONS FUNDED in 2018 (Winnipeg
ORGANIZATIONS FUNDED IN 2018 (Winnipeg - sorted by area) ORGANISATIONS FINANCÉES EN 2018 (Winnipeg - classées par secteur) Charleswood-Tuxedo Archers & Bowhunters Assoc of MB Assiniboine Park Conservancy Canadian Mennonite University Family Dynamics of Winnipeg Fort Whyte Alive Friends of the Harte Trail Grace Community Church Manitoba Cycling Association Manitoba Sailing Assoc. Nature Manitoba Oasis Community Church Purple Loosestrife Project of Manitoba Rotary Club of Winnipeg - Charleswood Varsity View Community Centre Winnipeg Military Family Resource Centre Winnipeg South Minor Baseball Association Daniel McIntyre Daniel McIntyre / St. Matthew's Comm. Assoc. Emmanuel Mission Church Ethio-Canadian Cultural Academy Girls with Pride and Dignity Foundation Living Bible Explorers (Winnipeg) Mission Baptist Church Monyjang Society of Manitoba Mood Disorders Association of Manitoba Robert A. Steen Memorial Community Centre Sargent Park Lawn Bowling Club Spence Neighbourhood Assoc. Valour Community Centre West Central Community Program West Central Women's Resource Centre West End BIZ Wii Chii Waakanak Learning Centre Winnipeg Art Gallery Winnipeg School Division (special needs project) Elmwood-East Kildonan Bronx Park Community Centre Chalmers Community Centre Chalmers Neighbourhood Renewal Corp. Congo Canada Charity Foundation East Elmwood Community Centre Elmwood Community Resource Centre Elmwood Giants Baseball Club Elmwood Mennonite Brethren Church Frontier College Hope Centre Ministries One Hope Min. of Canada-Adventure Day Camp River -

President's Message
President’s Message The MMF consultation meetings wrapped up with Each of us has economic power through our visits to Mafeking, The Pas, and Flin Flon the week purchases. Every dollar is equal and has the ability of September 12. There were MMF local executive to change our world. If your dollar is spent at a representatives and Métis at these and other competing pharmacy, you may get a smile from locations from across the Region and from across the behind the counter but the profit goes to shareholders province. elsewhere in Canada or around the world. When you buy at our pharmacy, the profits stay home and come Each of us has economic power back to our community through our own initiatives. through our purchases... When This past Friday, September 23rd at the beginning of you buy at our pharmacy, the our Annual General Assembly (AGA), we undertook profits stay home and come back a special workshop about our Land Claim. I was pleased to see so many of our Métis Citizens there. This summer the MMF undertook Land Claims to our community through our We are in an exciting time and I look forward to consultation meetings. During the meetings we own initiatives. announcements about our Claim over the coming provided a history of the legal and policy summaries weeks and months. I was also pleased to see some of the Supreme Court of Canada’s 2016 Daniels I want to thank The Pas Regional, Vice President and many of our Métis Citizens – especially our Elders decision and the Court’s 2013 MMF v Canada Directors, office staff and Local volunteers, for their and Youth – at this past weekend’s AGA that took decision – also known as our Land Claim Decision. -

WARDS BOUNDARIES COMMISSION - File GL – 5.1
WARDS BOUNDARIES COMMISSION - File GL – 5.1 Communication dated August 24, 2017, from Lisa Schreier ‐‐‐‐‐Original Message‐‐‐‐‐ From: [email protected] [mailto:[email protected]] Sent: Thursday, August 24, 2017 7:42 AM To: CLK‐CityClerks Subject: Winnipeg.ca : Comment Good morning! This note is to submit a comment about the reassessing of the City of Winnipeg Boundaries, which is heading for reassessment. My family lives in the Richmond Lakes area of Winnipeg, which is currently a part of the St. Norbert area. Living in this area is wonderful, a small little pocket of community, with parks, walking trails, and a short walk to the area of St. Norbert with the world‐class Farmers' Market, and much more. We love it here! Our current Councillor, Janice Lukes has been OUTSTANDING in putting some love and attention into our area, as we have always suffered from Perimeter‐itis (all projects seemed to happen within the city perimeter). Ms. Lukes has spent a lot of time and money in fixing up our areas. We are all grateful for the construction projects along Pembina Highway, an area that sadly has been over looked and neglected for years and is quite a depressing entrance to our City and should instead be celebrated as a HUGE starting point of one of the the longest roadway system (through to Mexico). Grandmont Park, our little treasure, is getting some love now ‐ upgraded walking paths, opened up parking lot and we are hoping for lights to be installed for the walkers and dog‐walkers' safety. And, what's important, is that Ms. -

Voter Turnout in Manitoba: an Ecological Analysis
Canadian Political Science Review, Vol. 6, No. 2-3, 2012, 267-279 267 Voter Turnout in Manitoba: An Ecological Analysis Jared J. Wesley a and Lydia Summerlee b a Department of Political Studies, University of Manitoba. Department of Political Science, University of Alberta. E-mail address: [email protected] b Department of Political Science, University of Guelph. E-mail address: [email protected] Abstract. This article treats Manitoba as a case study in the Résumé. Cet article se penche sur le Manitoba comme cas community-level factors influencing the rate of voter turn- d’étude des facteurs liés à la communauté qui influencent le out. Combining data from Elections Manitoba and the Mani- taux de participation électorale. En associant des données toba Bureau of Statistics, it consists of an ecological analysis provenant d’Élections Manitoba et du Bureau de Statistiques of electoral participation among the province’s fifty-seven du Manitoba, il consiste en une analyse écologique de parti- constituencies from 1999 to 2007. The study reveals that, cipation électorale dans les 57 circonscriptions de la pro- while conventional variables like age and affluence play a vince, de 1999 à 2007. Cette étude révèle que, tandis que les role, the competitiveness of the constituency is by far the variables liées à l’âge et à l’aisance économique jouent un most important factor in determining a district’s rate of rôle certain, la compétitivité de la circonscription est de loin voter turnout. This finding required analysts to shift their le plus important facteur qui détermine le taux de participa- focus to “competitiveness” as the dependent variable, which, tion électorale de la circonscription.