Disaster Response Patient Care Guidelines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Personal Protective Equipment (PPE) Guide
Personal Protective Equipment (PPE) Guide Volume 1: General PPE February 2003 F417-207-000 This guide is designed to be used by supervisors, lead workers, managers, employers, and anyone responsible for the safety and health of employees. Employees are also encouraged to use information in this guide to analyze their own jobs, be aware of work place hazards, and take active responsibility for their own safety. Photos and graphic illustrations contained within this document were provided courtesy of the Occupational Safety and Health Administration (OSHA), Oregon OSHA, United States Coast Guard, EnviroWin Safety, Microsoft Clip Gallery (Online), and the Washington State Department of Labor and Industries. TABLE OF CONTENTS (If viewing this pdf document on the computer, you can place the cursor over the section headings below until a hand appears and then click. You can also use the Adobe Acrobat Navigation Pane to jump directly to the sections.) How To Use This Guide.......................................................................................... 4 A. Introduction.........................................................................................6 B. What you are required to do ..............................................................8 1. Do a Hazard Assessment for PPE and document it ........................................... 8 2. Select and provide appropriate PPE to your employees................................... 10 3. Provide training to your employees and document it ........................................ 11 -
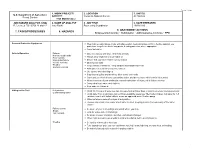
7. Tasks/Procedures 8. Hazards 9. Abatement
FS-6700-7 (11/99) 1. WORK PROJECT/ 2. LOCATION 3. UNIT(S) U.S. Department of Agriculture ACTIVITY Coconino National Forest All Districts Forest Service Trail Maintenance JOB HAZARD ANALYSIS (JHA) 4. NAME OF ANALYST 5. JOB TITLE 6. DATE PREPARED References-FSH 6709.11 and 12 Amy Racki Partnership Coordinator 10/28/2013 9. ABATEMENT ACTIONS 7. TASKS/PROCEDURES 8. HAZARDS Engineering Controls * Substitution * Administrative Controls * PPE Personal Protective Equipment Wear helmet, work gloves, boots with slip-resistant heels and soles with firm, flexible support, eye protection, long sleeve shirts, long pants, hearing protection where appropriate Carry first aid kit Vehicle Operation Fatigue Drive defensively and slow. Watch for animals Narrow, rough roads Always wear seatbelts and turn lights on Poor visibility Mechanical failure Ensure that you have reliable communication Vehicle Accients Obey speed limits Weather Keep vehicles maintained. Keep windows and windshield clean Animals on Road Anticipate careless actions by other drivers Use spotter when backing up Stay clear of gullies and trenches, drive slowly over rocks. Carry and use chock blocks, use parking brake, and do not leave vehicle while it is running Inform someone of your destination and estimated time of return, call in if plans change Carry extra food, water, and clothing Stop and rest if fatigued Hiking on the Trail Dehydration Drink 12-15 quarts of water per day, increase fluid on hotter days or during extremely strenuous activity Contaminated water Drink -

Hazard Control Selection and Management Requirements
ENVIRONMENT, SAFETY & HEALTH DIVISION Chapter 1: General Policy and Responsibilities Hazard Control Selection and Management Requirements Product ID: 671 | Revision ID: 1744 | Date published: 27 May 2015 | Date effective: 27 May 2015 URL: http://www-group.slac.stanford.edu/esh/eshmanual/references/eshReqControls.pdf 1 Purpose This document defines how a risk-based approach is used to determine the need for controls on facilities, systems, or components to protect the public, workers, and the environment. For controls necessary to prevent or mitigate serious events, specific devices and procedures will be formally credited as part of the approved safety envelope. How these controls are selected, evaluated, and approved, and the process for maintaining and modifying controls, are described in these requirements1. As used here, controls and hazard controls mean those engineered, administrative, or personal protective elements that are used to protect against a hazard. Normal process or operational controls are not included in these requirements except to the extent that their use is directly tied to safety. The concept of credited control is well established in the accelerator safety community. The concept of credited control is borrowed from DOE Order 420.2C, “Safety of Accelerator Facilities” (DOE O 420.2C), but this document neither extends the requirements of DOE O 420.2C to non-accelerator hazards nor modifies those requirements for accelerator hazards. The intent is to extend those robust principles to management of controls for non-accelerator hazards of similar risk. 2 Roles and Responsibilities 2.1 Associate Laboratory Director . Ensures that technical systems under his or her directorate’s management are properly analyzed to determine the type and level of controls necessary to control risk to an acceptable level . -
Code of Practice
HOW TO MANAGE WORK HEALTH AND SAFETY RISKS Code of Practice DECEMBER 2011 Safe Work Australia is an Australian Government statutory agency established in 2009. Safe Work Australia consists of representatives of the Commonwealth, state and territory governments, the Australian Council of Trade Unions, the Australian Chamber of Commerce and Industry and the Australian Industry Group. Safe Work Australia works with the Commonwealth, state and territory governments to improve work health and safety and workers’ compensation arrangements. Safe Work Australia is a national policy body, not a regulator of work health and safety. The Commonwealth, states and territories have responsibility for regulating and enforcing work health and safety laws in their jurisdiction. NSW note: This code of practice has been approved under section 274 of the Work Health and Safety Act 2011. Notice of that approval was published in the NSW Government Gazette referring to this code of practice as How to manage work health and safety risks (page 7194) on Friday 16 December 2011. This code of practice commenced on 1 January 2012. ISBN 978-0-642-33301-8 [PDF] ISBN 978-0-642-33302-5 [RTF] Creative Commons Except for the logos of Safe Work Australia, SafeWork SA, Workplace Standards Tasmania, WorkSafe WA, Workplace Health and Safety QLD, NT WorkSafe, WorkCover NSW, Comcare and WorkSafe ACT, this copyright work is licensed under a Creative Commons Attribution-Noncommercial 3.0 Australia licence. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/3.0/au/ In essence, you are free to copy, communicate and adapt the work for non commercial purposes, as long as you attribute the work to Safe Work Australia and abide by the other licence terms. -

Controlling Hazards (PDF)
Controlling Hazards Loss Control Bulletin Controlling Hazards Every workplace has the potential to expose an employee to occupational hazards which may result in injury or illness. Every employer has the responsibility of determining what hazards exist and how to properly control these hazards. One method that can be utilized to determine what hazards exist in an occupational setting is the job safety analysis. Once the hazards have been identified, a hierarchy of controls should be used to develop methods to protect employees from these occupa- tional hazards. Traditionally, a hierarchy of controls has been used as a means of determining how to implement feasible and effective controls for an occupational hazard. One representation of this hierarchy can be summarized as follows: Photo Credit: OSHA.gov The idea behind this hierarchy is that the control methods at the top of the list are potentially more effective and protective than those at the bottom. Applying this hierarchy is a systematic approach to identifying the most effective method of risk reduction. This normally leads to the implementation of inherently safer systems where the risk of illness or injury has been substantially reduced. Control Methods 1. Elimination and Substitution The first consideration for controlling hazards is to eliminate the hazard or substitute a less hazardous material or pro- cess. While eliminating or substituting is the most effective method to reduce hazards, it also tends to be the most diffi- cult to implement in an existing process as it may require major changes in equipment and procedures. One of the best times to utilize this method is during the design or development stage when making these changes can be inexpensive and simple to implement. -
Guidance for the Selection and Use of PPE in the Healthcare Setting
Guidance for the Selection and Use of Personal Protective Equipment (PPE) in Healthcare Settings 1 PPE Use in Healthcare Settings: Program Goal Improve personnel safety in the healthcare environment through appropriate use of PPE. PPE Use in Healthcare Settings The goal of this program is to improve personnel safety in the healthcare environment through appropriate use of PPE. 2 PPE Use in Healthcare Settings: Program Objectives • Provide information on the selection and use of PPE in healthcare settings • Practice how to safely don and remove PPE PPE Use in Healthcare Settings The objectives of this program are to provide information on the selection and use of PPE in healthcare settings and to allow time for participants to practice the correct way to don and remove PPE. 3 Personal Protective Equipment Definition “specialized clothing or equipment worn by an employee for protection against infectious materials” (OSHA) PPE Use in Healthcare Settings Personal protective equipment, or PPE, as defined by the Occupational Safety and Health Administration, or OSHA, is “specialized clothing or equipment, worn by an employee for protection against infectious materials.” 4 Regulations and Recommendations for PPE • OSHA issues workplace health and safety regulations. Regarding PPE, employers must: – Provide appropriate PPE for employees – Ensure that PPE is disposed or reusable PPE is cleaned, laundered, repaired and stored after use • OSHA also specifies circumstances for which PPE is indicated • CDC recommends when, what and how to use PPE PPE Use in Healthcare Settings OSHA issues regulations for workplace health and safety. These regulations require use of PPE in healthcare settings to protect healthcare personnel from exposure to bloodborne pathogens and Mycobacterium tuberculosis. -

Hierarchy of Controls” Specifies the Order in Which Controls Are Implemented in the Workplace
Hierarchy of FactSheet Controls he “Hierarchy of Controls” specifies the order in which controls are implemented in the workplace. They are the means for reducing employee exposures to occupational hazards. Control measures are established to T maintain employee exposures below permissible and recommended limits. It is usually more cost-effective to implement safety • Personal Protective Equipment – PPE (e.g., measures before facilities or processes are built. By using respirators, fall protection, ear plugs, lab coat) is used this proactive approach, controls are implemented in the when engineering controls are not available and/or to early stages of a project, resulting in the prevention of enhance existing engineering controls. injuries, environmental incidents, and property damage. What I need to do... • Elimination – Remove the hazard from the workplace. It is the most effective way to control a risk because • Employ engineering controls routinely such the hazard is no longer present. as a chemical fume hood, biosafety cabinet, • Substitution – Use a chemical that is less hazardous machine guarding, and guard rails to isolate or less toxic than a principal ingredient in a synthesis, the hazards. for instance. This may add more steps to the process, • Read and comprehend administrative but may be safer in the long run. Conduct a hazard controls such as protocols, standard operating assessment to verify. procedures, and warning signs. Complete • Engineering Controls – Enclose or isolate the hazard safety training to understand occupational with local exhaust ventilation, machine guarding, hazards and risks. guardrails, or other safety equipment. • Wear the appropriate personal protective • Administrative Controls – Require workers to do equipment for the hazard. -
Methods of Control
MODULE 4 METHODS OF CONTROL Recognize Evaluate Control At the end of this module, you will be able to… Identify the three types of control that should be used to achieve electrical safety. Identify the engineering, administrative and PPE electrical controls you use on your job as well as the controls you should be using. Identify facts and procedures relating to lockout/tagout. List the steps required to achieve an electrically safe condition. Recognize when a work permit is required to work on energized electrical circuits. Recognize the appropriate warning signs to alert employees to the danger of electricity. Recognize the appropriate PPE to use based on the calculated energy value of an energy source. Given a case study, determine the most appropriate method of control and necessary corrective action. Prevention Strategies for Electrical Hazards 1 © 2008 National Safety Council MODULE 4 PARTICIPANT GUIDE Controls for Electrical Hazards Question: What is a control? Answer: Three Types of Control Engineering—Engineering controls engineer the hazard out by initial design specifications or by applying substituion methods, isolation, enclosure, or ventilation. Of the three types of controls, engineering control methods should be considered first. Examples: Administrative—Administrative controls reduce employee exposures through methods such as education and training, work reduction, job rotation, maintenance/repairs, housekeeping, personal hygiene, and appropriate work practices. Administrative controls depend on constant human implementation or intervention. Examples: Personal Protective Equipment (PPE)—Personal Protective Equipment is worn by employees to protect them from the environment. PPE includes anything from gloves to full body suits with self-contained breathing apparatus and can be used with engineering and administrative controls. -

LASER Treatment of Laryngeal Papillomatosis in a Young Child: Anaesthetic and Surgical Management Faisal Shamim1, Durriya Raza1 and Mubasher Ikram2
CASE REPORT LASER Treatment of Laryngeal Papillomatosis in a Young Child: Anaesthetic and Surgical Management Faisal Shamim1, Durriya Raza1 and Mubasher Ikram2 ABSTRACT The authors report the case of a 4-year boy who required anaesthetic and surgical care during LASER excision of laryngeal papillomatosis. He presented with hoarseness and stridor and underwent emergency tracheostomy after confirmation of laryngeal papillomas on CT scan. He required LASER treatment under general anaesthesia with a requirement of paediatric LASER-safe endotracheal tube but unfortunately, this was not available in the country. Balanced anaesthesia technique using inhalational anaesthetic, muscle relaxant and narcotic is used with modifications. After three successful surgical sessions, the airway became patent and tracheostomy was de-cannulated. The perioperative issues surrounding this process are discussed including anaesthetic induction in the patient with a compromised airway, maintenance anaesthetic techniques, methods used for ventilation during LASER surgery of the upper airway, surgical implications and hazards of LASER to the operating room personnel. Key Words: Anaesthesia. LASER. LASER-Flex ETT. Laryngeal papillomatosis. INTRODUCTION room air with respiratory rate of 38/minute. On Human Papilloma Virus (HPV) type 6 or 11 is most examination, subcostal recessions were present. common causative organism for benign epithelial Decreased bilateral air entry and wheeze with tracheal tumours of upper respiratory tract termed as papilloma.1 tug was found on chest auscultation. CT scan head and Both adults and children can have this problem and neck showed laryngeal stenosis due to presence of may present with wheezing, hoarseness, or stridor. The papillomas on left vocal cord (Figure 1). goals of treatment are debulking, improvement of the He was rushed to the operating room for emergency voice and remission of papillomas.2 Paediatric patients tracheostomy and Direct Laryngoscopy (DL) ± biopsy. -
Controlling Ergonomic Hazards
F A C T S H E E T E 1 Controlling Ergonomic Hazards There are many ways to reduce ergonomic risk factors and help fit the workplace to the worker. Solutions can be grouped into three main categories: eliminate the hazard, improve work policies and procedures, and provide personal protective equipment. Often the best solution involves a combination of approaches. Eliminate the Hazard The most effective way to control ergonomic hazards is to eliminate the risk factors altogether. Sometimes you can change the tools, equipment, job design, or work area to remove the hazard completely. This is called using “engineering controls.” These are some examples of engineering controls: • Redesign workstations and work areas to eliminate reaching, bending, or other awkward postures. • Provide adjustable tables and chairs that can be used by workers with a range of sizes and shapes, and that allow neutral postures. • Provide carts for transporting material and mechanical hoists to eliminate lifting. • Use tools that fit the hand, have no sharp edges, and eliminate awkward hand and wrist positions. • Change where materials are stored to minimize reaching. • Design containers with handles or cutouts for easy gripping. Improving the workplace is the heart of ergonomics: changing the work to fit the worker. The design should accommodate the wide range of people assigned to the task. W O S H Specialist Training Supplemental Module Preventing Musculoskeletal Disorders 2 F A C T S H E E T E C O N T R O L L I N G E R G O N O M I C H A Z A R D S Improve Work Policies and Procedures The next most effective solution is to develop work policies, procedures, and practices that change how the job is done. -

Risk Management Guide
Risk Management Guide What is health and safety risk management? Risk Management is a proactive, logical and systematic approach of managing the uncertainty relating to potential risk, rather than responding to injury, incident or damage. Why do we perform the risk management process? The Work Health and Safety Act 2011 (the Act) (s17) details how an organisation can manage exposure to risks. Section 17 of the Act states: “A duty imposed on a person to ensure health and safety requires the person— (a) “to eliminate risks to health and safety, so far as is reasonably practicable; and (b) if it is not reasonably practicable to eliminate risks to health and safety, to minimise those risks so far as is reasonably practicable”. In minimising risks to health and safety, the University must: a) identify hazards; b) assess the risks that may result because of hazards; c) decide on appropriate control measures to prevent, or minimise the level of, the risks; d) implement control measures; and e) monitor and review the effectiveness of these measures What is the difference between hazard and risk? Hazard means a situation or thing that has the potential to harm a person. These may include; noisy machinery, a moving forklift, chemicals, electricity, working at heights, a repetitive job, bullying and violence at the workplace. Risk is the possibility that harm (death, injury or illness) might occur when exposed to a hazard. Hazard Risk Work at heights Breaking a limb as a result from a fall from height Electricity Electrical shock from faulty electrical lead Scalpel Cut/laceration from incorrect use of equipment Wet floor Sprained ankle from slipping on a wet floor Who must ensure work health and safety? At Griffith University, the Vice Chancellor maintains ultimate responsibility for ensuring workplace health and safety. -

Medical Surveillance for Healthcare Workers Exposed to Hazardous Drugs
Medical Surveillance for Healthcare Workers Exposed to Hazardous Drugs Summary Description of Exposure Healthcare workers who prepare, administer, or transport hazardous Drugs are considered hazardous if stud- drugs or dispose of hazardous drug ies in animals or humans show that they waste may face risks to their own have the potential to cause cancer, repro- health such as skin disorders, re- ductive toxicity, birth defects, or damage productive disorders, and possibly to organs at low doses [NIOSH 2004]. In cancer. NIOSH recommends that the United States, an estimated 8 million employers establish a medical sur- healthcare workers are potentially ex- veillance program as part of a com- posed to hazardous drugs or drug waste prehensive prevention program at their worksites [BLS 2011]. Healthcare that also minimizes worker expo- Figure 1. Multi-channel infusion pump workers who should be included in the for delivery of chemotherapy. sure through engineering controls, medical surveillance program are work- good work practices, and person- ers who may be exposed to hazardous al protective equipment (PPE) and drugs directly such as nurses, pharma- Table 1. Job titles that may provides education about working cists, and pharmacy technicians; or oth- involve exposure to hazardous with hazardous drugs. Medical sur- er workers (e.g., nurses’ aides, laundry drugs: veillance involves collecting and in- workers) who may come into contact 1. Pharmacists and pharmacy terpreting data to detect changes in with hazardous or patient waste [OSHA technicians the health status of working popu- 1999; NIOSH 2004; ASHP 2006; ONS 2. Nurses (RNs, ARNPs, LPNs) lations potentially exposed to haz- 2011].