School of Medicine and Dentistry Student Handbook
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
COMLEX-USA for Residency Program Directors
COMLEX-USA FOR RESIDENCY PROGRAM DIRECTORS COMLEX-USA Evidence–based assessment designed specifically for osteopathic medical students and residents that measures competencies required for the provision of safe and effective osteopathic medical care to patients. It is recommended but not required that COMLEX-USA Level 3 be taken after a minimum of six months in residency. The attestation process for COMLEX-USA Level 3 helps to fulfill the NBOME mission to DO candidates are not required to pass the United States protect the public, and adds value and entrustability to state licensing Medical Licensing Examination (USMLE®) to be eligible to boards and patients. Additionally, attestation provides COMLEX-USA apply to ACGME-accredited residency programs. The score reports to residency program directors and faculty. ACGME does not specify which licensing board exam(s) (i.e., COMLEX-USA, USMLE) applicants must take to be eligible COMPETENCY AND EVIDENCE-BASED DESIGN for appointment in ACGME-accredited residency programs. In 2019, COMLEX-USA completed a transition to a contemporary, two Frequently Asked Questions: Single Accreditation System decision-point, competency-based exam blueprint and evidence- Accreditation Council for Graduate Medical Education, 20191 based design informed by extensive research on osteopathic physician practice, expert consensus and stakeholder surveys.3 The enhanced COMLEX-USA blueprint4 assesses measurable outcomes PATHWAY TO LICENSURE of seven Fundamental Osteopathic Medical Competency Domains5 COMLEX-USA, the Comprehensive Osteopathic Medical Licensing and focuses on high-frequency, high-impact health issues and clinical Examination of the United States, is the exam series used by all presentations that affect patients. medical licensing authorities to make licensing decisions for osteopathic physicians. -

Medical-Dental History Personal History All of the Information Which You Provided on This Form Will Be Held in the Strictest Confidence
Medical-Dental History Personal History All of the information which you provided on this form will be held in the strictest confidence. Although some questions may seem unimportant at the time, they may be vital in an emergency situation. Please answer each question and ask if you need assistance completing the form. Patients Name:________________________________________________ Sex: M F Parents / Guardian:___________________________________________________________________ Date of Birth: __________________________ BC Care Card: ____________________________ Mailing Address:_____________________________________________________________________ Home Phone: ______________________________ Cell Phone:________________________________ E-Mail:_____________________________________________________________________________ Purpose of Visit:______________________________________________________________________ Family Dentist:____________________________ Medical Doctor: ___________________________ Referred by:_________________________________________________________________________ I authorize the doctor to perform diagnostic procedures and treatment as may be necessary for proper dental care. I authorize the release of information concerning my child’s health care, advice, and treatment provided for the purpose of evaluating and administering claims for insurance benefits. I understand that my dental insurance carrier or payer of my dental benefits may pay less than the actual fee for services. I understand that I am financially responsible for payment -

Dental Medicine (DDS/DMD)
Pre-Health Information for Dental Medicine (DDS/DMD) Dentists who have a DMD or DDS have the similar education. Both degrees use the same curriculum requirements set by the American Dental Association and the type of degree awarded is determined by the university. Profession web site(s): www.ada.org , www.adea.org Application web site: www.adea.org/aadsas or for Texas schools: www.tmdsas.com Admission/Entrance exam:– DAT (Dental Admission Test) Transcripts: Official transcripts from ALL institutions attended, including Marquette University, must be sent directly from the institution to the central application service. If you completed study abroad courses at a U.S. sponsored program abroad, you must send transcripts. If you studied abroad and the courses and grades do not appear on a U.S. transcript, then you need to have transcripts sent to AADSAS from the foreign school or an evaluation service. Course prerequisites: Course prerequisites vary by program. Typical prerequisites include Biology 1001, 1002, a separate lab course such as Biology 2001, a biochemistry course, Chemistry 1001, 1002, 2111, 2112, Physics 1001 and 1002. Different course numbers for majors (e.g., Chemistry 1014 for Majors) will be accepted. Physics is required for dental school but not for the DAT. Many dental schools require courses such as Biochemistry, Anatomy, Physiology and/or Microbiology, Psychology, Sociology and other upper level biology or science courses. Students should research schools to which they will apply early enough to ensure they can complete all necessary pre-requisite courses. Observation hours/experience: Dental schools like to see well-rounded applications and look for quality and depth of experiences rather than requiring a specific number of hours. -

ADA.Org: Dental History Timeline
ARCHIVES OF THE AMERICAN DENTAL ASSOCIATION HISTORY OF DENTISTRY TIMELINE Compiled from various sources by ADA Library/Archives staff Ancient Origins • 5000 BC -A Sumerian text of this date describes “tooth worms” as the cause of dental decay. • 2600 BC -Death of Hesy-Re, an Egyptian scribe, often called the first “dentist.” An inscription on his tomb includes the title “the greatest of those who deal with teeth, and of physicians.” This is the earliest known reference to a person identified as a dental practitioner. • 1700-1550 BC -An Egyptian text, the Ebers Papyrus, refers to diseases of the teeth and various toothache remedies. • 500-300 BC -Hippocrates and Aristotle write about dentistry, including the eruption pattern of teeth, treating decayed teeth and gum disease, extracting teeth with forceps, and using wires to stabilize loose teeth and fractured jaws. • 100 BC -Celsus, a Roman medical writer, writes extensively in his important compendium of medicine on oral hygiene, stabilization of loose teeth, and treatments for toothache, teething pain, and jaw fractures. • 166-201 AD-The Etruscans practice dental prosthetics using gold crowns and fixed bridgework. The Beginnings of A Profession—Middle Ages • 500-1000 -During the Early Middle Ages in Europe medicine and surgery, including dentistry, is generally practiced by monks, the most educated people of the period. • 700 -A medical text in China mentions the use of “silver paste,” a type of amalgam. • 1130-1163 -A series of Papal edicts prohibit monks from performing any type of surgery, bloodletting or tooth extraction. Barbers often assisted monks in their surgical ministry because they visited monasteries to shave the heads of monks and the tools of the barber trade—sharp knives and razors—were useful for surgery. -
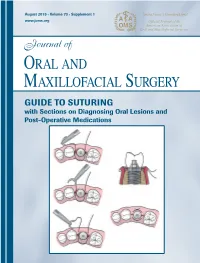
GUIDE to SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications
Journal of Oral and Maxillofacial Surgery Journal of Oral and Maxillofacial August 2015 • Volume 73 • Supplement 1 www.joms.org August 2015 • Volume 73 • Supplement 1 • pp 1-62 73 • Supplement 1 Volume August 2015 • GUIDE TO SUTURING with Sections on Diagnosing Oral Lesions and Post-Operative Medications INSERT ADVERT Elsevier YJOMS_v73_i8_sS_COVER.indd 1 23-07-2015 04:49:39 Journal of Oral and Maxillofacial Surgery Subscriptions: Yearly subscription rates: United States and possessions: individual, $330.00 student and resident, $221.00; single issue, $56.00. Outside USA: individual, $518.00; student and resident, $301.00; single issue, $56.00. To receive student/resident rate, orders must be accompanied by name of affiliated institution, date of term, and the signature of program/residency coordinator on institution letter- head. Orders will be billed at individual rate until proof of status is received. Prices are subject to change without notice. Current prices are in effect for back volumes and back issues. Single issues, both current and back, exist in limited quantities and are offered for sale subject to availability. Back issues sold in conjunction with a subscription are on a prorated basis. Correspondence regarding subscriptions or changes of address should be directed to JOURNAL OF ORAL AND MAXILLOFACIAL SURGERY, Elsevier Health Sciences Division, Subscription Customer Service, 3251 Riverport Lane, Maryland Heights, MO 63043. Telephone: 1-800-654-2452 (US and Canada); 314-447-8871 (outside US and Canada). Fax: 314-447-8029. E-mail: journalscustomerservice-usa@ elsevier.com (for print support); [email protected] (for online support). Changes of address should be sent preferably 60 days before the new address will become effective. -
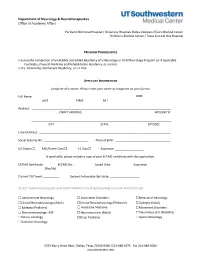
Neurology Fellowship Application
Department of Neurology & Neurotherapeutics Office of Academic Affairs Parkland Memorial Hospital / University Hospitals Dallas Veterans Affairs Medical Center Children's Medical Center / Texas Scottish Rite Hospital PROGRAM PREREQUISITES • Successful completion of an ACGME accredited Residency of a Neurology or Child Neurology Program (or if applicable Psychiatry, Physical Medicine and Rehabilitation Residency, or similar). • U.S. Citizenship, Permanent Residency, or J-1 Visa APPLICANT INFORMATION Complete all sections. Please enter your name as it appears on your license. Full Name: DOB: LAST FIRST M.I. Address: STREET ADDRESS APT/UNIT # ______________________________________________________________________________________ CITY STATE ZIP CODE Email Address: _________________________________________________________________________________ Social Security No.: ___________________________ Place of Birth: __________________________________ US Citizen ☐ EAD/Green Card ☐ J-1 Visa ☐ Expiration __________________ If applicable, please include a copy of your ECFMG certificate with this application. ECFMG Certificate: ________ ECFMG No.: ____________ Issued Date: _____________ Expiration ______________ (Yes/No) Current PGY level: __________ Desired Fellowship start date: __________________ SELECT WHICH NEUROLOGY & NEUROTHERAPEUTICS FELLOWSHIP(S) YOU ARE APPLYING FOR: ☐ Autoimmune Neurology ☐ Autonomic Disorders ☐Behavioral Neurology ☐Clinical Neurophysiology (Adult) ☐Clinical Neurophysiology (Pediatric) ☐ Epilepsy (Adult) ☐ Epilepsy (Pediatric) -

Boston Children's Hospital / Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health
Boston Children’s Hospital/Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health Speaker Alan Woolf, MD, MPH, FAACT, FAAP, FACMT Director, Pediatric Environmental Health Center, Boston Children’s Hospital Director, Region 1 New England PEHSU Director, Fellowship Training Program Professor, Harvard Medical School School Physician Acknowledgments & Disclosures This material was supported by the American Academy of Pediatrics (AAP) and funded (in part) by the cooperative agreement FAIN: 5 NU61TS000237-05 from the Agency for Toxic Substances and Disease Registry (ATSDR). Funding for this seminar was made possible (in part) by the cooperative agreement award number 1U61TS000237- 05 from the Agency for Toxic Substances and Disease Registry (ATSDR). The views expressed in written materials and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services. •The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government •Neither EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications. •In the past 12 months, we have had no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed -
Medical Scientist Training Program
The University of Michigan MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines A Handbook for Fellows https://www.medicine.umich.edu/medschool/education/md-phd- program/current students/ August 2018 CONTENTS 1. MSTP Office 2. Communication 3. Academic Advising 4. I.D. and Computer Access 5. Course of Study 6. Biological Chemistry Requirement 7. Medical School Registration 8. Medical and Graduate School Grading Systems 9. Graduate School Registration 10. Research Rotations 11. Selecting a Doctoral Field and the Thesis Research Mentor 12. Graduate School Residency Requirements 13. Research Responsibility and Ethics Requirements 14. Research Phase: External Funding Sources 15. Advancement to Candidacy 16. Precandidate Year to Candidacy Transition: Funding and Insurance Issues 17. Research Phase to M3 Transition 18. M4 Year 19. Transition to Post Graduate Training, Residency 20. Dean’s Letters 21. Simultaneous Awarding of Dual Degrees 22. United States Medical Licensure Examination Step 1 and Step 2 (Clinical Knowledge and Clinical Skills) 23. Rackham Graduate School Policies 24. Medical School Policies and Procedures 25. The Fellowship Award and the Stipend Level 26. Monthly Stipend Check 27. Taxability of NRSA Stipends 28. NIH Funding Trainee Appointment Forms and Trainee Termination Notice Forms 29. Tuition Payment, Billing Procedures, and Registration 30. Travel Funds and Expense Forms 31. Health Care Insurance 32. Health Service 33. CV and Publication File 34. Individual Development Pan (IDP) 35. Vacations and Other Absences 36. MSTP Scientific Retreat 37. MSTP Seminars 38. Citizenship 39. MSTP Committees: Operating Committee (OC) and Program Activities Committee (PAC) A Handbook for MSTP Fellows MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines for Fellows 1. -

Primer for Applying to Internal Medicine Residency Programs A
Primer for Applying to Internal Medicine Residency Programs A) Fourth-Year Schedule: • Ideally, schedule the internal medicine sub-internship during July or August in order to procure a letter of recommendation (if needed). • Alternative clinical experiences to consider in place of the sub-internship include: o Away rotations: ▪ Away rotations are NOT required for IM. The majority of students applying to IM across the country do not partake in visiting rotations. Visiting rotations are most helpful if students demonstrate a significant interest in a particular program or location. ▪ Away rotations may increase the chance of an invitation to interview at the hosting institution, but this is NOT guaranteed. ▪ Visiting subspecialty electives are preferred over visiting sub- internships, which require strong institutional systems knowledge to optimize clinical performance. o Critical Care Clerkship o Subspecialty Rotations at Cooper • IM residency interviews often start in mid-October and extend to the end of January with the majority of interviews occurring in November and December. Therefore, plan accordingly. • Schedule a more rigorous clinical experience in the spring to enhance clinical skills prior to graduation in preparation for residency. B) Timeline: C) Curriculum Vitae & ERAS Application: • Timeline: Should include all longitudinal, meaningful experiences from the first day of college until present day. • Experience Boxes: o Research Experience: ▪ Include all meaningful research at both the undergraduate and medical school level -
Manual of Applied Infection Prevention and Control
MANUAL OF APPLIED INFECTION PREVENTION AND CONTROL 2021-2022 1 Table of Contents OVERVIEW: APPLIED INFECTION PREVENTION AND CONTROL .............................. 5 Introduction ......................................................................................................................................... 5 Rationale ................................................................................................................................................ 5 How does infection occur ................................................................................................................. 5 Contact transmission .................................................................................................................................... 5 i. Direct ..................................................................................................................................................................... 5 ii. Indirect ................................................................................................................................................................. 5 Droplets .............................................................................................................................................................. 5 Aerosols .............................................................................................................................................................. 5 Infection Control Protocol: Standard Precautions ................................................................ -
SAP Crystal Reports
Results of the 2016 NRMP Program Director Survey Specialties Matching Service October 2016 www.nrmp.org Requests for permission to use these data as well as questions about the content of this publication or the National Resident Matching Program data and reports may be directed to Mei Liang, Director of Research, NRMP, at [email protected]. Questions about the NRMP should be directed to Mona M. Signer, President and CEO, NRMP, at [email protected]. Suggested Citation National Resident Matching Program, Data Release and Research Committee: Results of the 2016 NRMP Program Director Survey, Specialties Matching Service. National Resident Matching Program, Washington, DC. 2016. Copyright © 2016 National Resident Matching Program. All rights reserved. Permission to use, copy and/or distribute any documentation and/or related images from this publication shall be expressly obtained from the NRMP. Table of Contents Introduction .................................................................................................................................................... 1 Response rates ................................................................................................................................................. 2 All Specialties................................................................................................................................................. 3 Charts for Individual Specialties Abdominal Transplant Surgery .................................................................................................................... -

Georgia Boards of Dentistry and Pharmacy Presentation
Georgia Boards of Dentistry & Pharmacy Presentation to: The DCH Board Presented by: Tanja D. Battle Date: May 8, 2014 0 Mission The Georgia Department of Community Health We will provide Georgians with access to affordable, quality health care through effective planning, purchasing and oversight. We are dedicated to A Healthy Georgia. 1 STAFF OF THE BOARDS Tanja Battle Executive Director Asst Executive Director Eric Lacefield Rick Allen Dep. Executive Director Eva James Vacant Title or ChapterLicensure Analyst Slide Supervisor Annie Ruth Parks Janice Cook Taylor Hearn (use as needed;Licensure feel Analyst freeCustomer to Service delete)Specialist(Intake) Information/Referral Specialist Itovia Evans Licensure Analyst Ruth Reece Licensure Analyst Ryan McNeal Anil Foreman Anna Petway Brandi Howell Dianne Yawn Chief Investigator Legal Officer Compliance Analylst Business Operations Specialist Compliance Analyst 2 GEORGIA BOARD OF DENTISTRY 3 COMPOSITION OF THE BOARD OF DENTISTRY • 11 members: – Richard G. Bennett, D.M.D. (President) – Logan Nalley, Jr., D.M.D. (Vice-President) – Rebecca B. Bynum, R.D.H. – Randy Daniel, D.M.D. – Tracy Gay, D.M.D. – Thomas P. Godfrey, D.M.D. – Steve Holcomb, D.M.D. – Antwan L. Treadway, D.M.D. – H. Bert Yeargan, D.D.S. – Connie Engel (Consumer Member) • Appointed and commissioned by the Governor • Terms of 2 (hygienist), 4 (consumer), or 5 (dentist) years • Representation by Department of Law: Bryon A. Thernes, Esq., Assistant Attorney General 4 MEETINGS and COMMITTEES • At least one per month, typically the