Primer for Applying to Internal Medicine Residency Programs A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
COMLEX-USA for Residency Program Directors
COMLEX-USA FOR RESIDENCY PROGRAM DIRECTORS COMLEX-USA Evidence–based assessment designed specifically for osteopathic medical students and residents that measures competencies required for the provision of safe and effective osteopathic medical care to patients. It is recommended but not required that COMLEX-USA Level 3 be taken after a minimum of six months in residency. The attestation process for COMLEX-USA Level 3 helps to fulfill the NBOME mission to DO candidates are not required to pass the United States protect the public, and adds value and entrustability to state licensing Medical Licensing Examination (USMLE®) to be eligible to boards and patients. Additionally, attestation provides COMLEX-USA apply to ACGME-accredited residency programs. The score reports to residency program directors and faculty. ACGME does not specify which licensing board exam(s) (i.e., COMLEX-USA, USMLE) applicants must take to be eligible COMPETENCY AND EVIDENCE-BASED DESIGN for appointment in ACGME-accredited residency programs. In 2019, COMLEX-USA completed a transition to a contemporary, two Frequently Asked Questions: Single Accreditation System decision-point, competency-based exam blueprint and evidence- Accreditation Council for Graduate Medical Education, 20191 based design informed by extensive research on osteopathic physician practice, expert consensus and stakeholder surveys.3 The enhanced COMLEX-USA blueprint4 assesses measurable outcomes PATHWAY TO LICENSURE of seven Fundamental Osteopathic Medical Competency Domains5 COMLEX-USA, the Comprehensive Osteopathic Medical Licensing and focuses on high-frequency, high-impact health issues and clinical Examination of the United States, is the exam series used by all presentations that affect patients. medical licensing authorities to make licensing decisions for osteopathic physicians. -
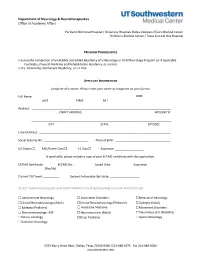
Neurology Fellowship Application
Department of Neurology & Neurotherapeutics Office of Academic Affairs Parkland Memorial Hospital / University Hospitals Dallas Veterans Affairs Medical Center Children's Medical Center / Texas Scottish Rite Hospital PROGRAM PREREQUISITES • Successful completion of an ACGME accredited Residency of a Neurology or Child Neurology Program (or if applicable Psychiatry, Physical Medicine and Rehabilitation Residency, or similar). • U.S. Citizenship, Permanent Residency, or J-1 Visa APPLICANT INFORMATION Complete all sections. Please enter your name as it appears on your license. Full Name: DOB: LAST FIRST M.I. Address: STREET ADDRESS APT/UNIT # ______________________________________________________________________________________ CITY STATE ZIP CODE Email Address: _________________________________________________________________________________ Social Security No.: ___________________________ Place of Birth: __________________________________ US Citizen ☐ EAD/Green Card ☐ J-1 Visa ☐ Expiration __________________ If applicable, please include a copy of your ECFMG certificate with this application. ECFMG Certificate: ________ ECFMG No.: ____________ Issued Date: _____________ Expiration ______________ (Yes/No) Current PGY level: __________ Desired Fellowship start date: __________________ SELECT WHICH NEUROLOGY & NEUROTHERAPEUTICS FELLOWSHIP(S) YOU ARE APPLYING FOR: ☐ Autoimmune Neurology ☐ Autonomic Disorders ☐Behavioral Neurology ☐Clinical Neurophysiology (Adult) ☐Clinical Neurophysiology (Pediatric) ☐ Epilepsy (Adult) ☐ Epilepsy (Pediatric) -

Boston Children's Hospital / Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health
Boston Children’s Hospital/Harvard Medical School Fellowship Training in Pediatric & Reproductive Environmental Health Speaker Alan Woolf, MD, MPH, FAACT, FAAP, FACMT Director, Pediatric Environmental Health Center, Boston Children’s Hospital Director, Region 1 New England PEHSU Director, Fellowship Training Program Professor, Harvard Medical School School Physician Acknowledgments & Disclosures This material was supported by the American Academy of Pediatrics (AAP) and funded (in part) by the cooperative agreement FAIN: 5 NU61TS000237-05 from the Agency for Toxic Substances and Disease Registry (ATSDR). Funding for this seminar was made possible (in part) by the cooperative agreement award number 1U61TS000237- 05 from the Agency for Toxic Substances and Disease Registry (ATSDR). The views expressed in written materials and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services. •The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government •Neither EPA nor ATSDR endorse the purchase of any commercial products or services mentioned in PEHSU publications. •In the past 12 months, we have had no relevant financial relationships with the manufacturer(s) of any commercial product(s) and/or provider(s) of commercial services discussed -
Medical Scientist Training Program
The University of Michigan MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines A Handbook for Fellows https://www.medicine.umich.edu/medschool/education/md-phd- program/current students/ August 2018 CONTENTS 1. MSTP Office 2. Communication 3. Academic Advising 4. I.D. and Computer Access 5. Course of Study 6. Biological Chemistry Requirement 7. Medical School Registration 8. Medical and Graduate School Grading Systems 9. Graduate School Registration 10. Research Rotations 11. Selecting a Doctoral Field and the Thesis Research Mentor 12. Graduate School Residency Requirements 13. Research Responsibility and Ethics Requirements 14. Research Phase: External Funding Sources 15. Advancement to Candidacy 16. Precandidate Year to Candidacy Transition: Funding and Insurance Issues 17. Research Phase to M3 Transition 18. M4 Year 19. Transition to Post Graduate Training, Residency 20. Dean’s Letters 21. Simultaneous Awarding of Dual Degrees 22. United States Medical Licensure Examination Step 1 and Step 2 (Clinical Knowledge and Clinical Skills) 23. Rackham Graduate School Policies 24. Medical School Policies and Procedures 25. The Fellowship Award and the Stipend Level 26. Monthly Stipend Check 27. Taxability of NRSA Stipends 28. NIH Funding Trainee Appointment Forms and Trainee Termination Notice Forms 29. Tuition Payment, Billing Procedures, and Registration 30. Travel Funds and Expense Forms 31. Health Care Insurance 32. Health Service 33. CV and Publication File 34. Individual Development Pan (IDP) 35. Vacations and Other Absences 36. MSTP Scientific Retreat 37. MSTP Seminars 38. Citizenship 39. MSTP Committees: Operating Committee (OC) and Program Activities Committee (PAC) A Handbook for MSTP Fellows MEDICAL SCIENTIST TRAINING PROGRAM General Information and Guidelines for Fellows 1. -
SAP Crystal Reports
Results of the 2016 NRMP Program Director Survey Specialties Matching Service October 2016 www.nrmp.org Requests for permission to use these data as well as questions about the content of this publication or the National Resident Matching Program data and reports may be directed to Mei Liang, Director of Research, NRMP, at [email protected]. Questions about the NRMP should be directed to Mona M. Signer, President and CEO, NRMP, at [email protected]. Suggested Citation National Resident Matching Program, Data Release and Research Committee: Results of the 2016 NRMP Program Director Survey, Specialties Matching Service. National Resident Matching Program, Washington, DC. 2016. Copyright © 2016 National Resident Matching Program. All rights reserved. Permission to use, copy and/or distribute any documentation and/or related images from this publication shall be expressly obtained from the NRMP. Table of Contents Introduction .................................................................................................................................................... 1 Response rates ................................................................................................................................................. 2 All Specialties................................................................................................................................................. 3 Charts for Individual Specialties Abdominal Transplant Surgery .................................................................................................................... -

School of Medicine and Dentistry Student Handbook
University of Rochester School of Medicine and Dentistry Student Handbook Updated: September 21, 2021 1 | Page INTRODUCTION This official student handbook has been compiled to inform students about institutional policies as well as to identify many services and resources that may be of value during their training at Rochester. The policies and guidelines of the School are dynamic – constantly being improved through the efforts of students, faculty, and administration. We publish the official handbook in a web-based format and send students periodic updates. All policies are subject to improvement and revision at any time. We hope students find these materials to be useful. Should students have any comments, concerns, or questions, they should contact their Advisory Dean or any staff member in the Student Services Center. Sincerely, David R. Lambert, M.D. Senior Associate Dean for Medical Student Education 2 | Page Table of Contents INTRODUCTION ................................................................................................................................................................................... 2 I. ADMISSIONS ................................................................................................................................................................................. 8 FALSIFICATION OF ADMISSIONS INFORMATION .................................................................................................................... 8 Academic, Behavioral and Professionalism Expectations of Accepted -
Postgraduate Training for Md-Phds Optimizing the Path to Independence Part I: Research Residencies
POSTGRADUATE TRAINING FOR MD-PHDS OPTIMIZING THE PATH TO INDEPENDENCE PART I: RESEARCH RESIDENCIES 2015 NATIONAL ASSOCIATION OF MD-PHD PROGRAMS ANNUAL PROFESSIONAL DEVELOPMENT MEETING Robin G. Lorenz, M.D., Ph.D. Assistant Dean for Physician Scientist Education Department of Pathology University of Alabama at Birmingham [email protected] Presenters • Larry S. Schlesinger, M.D. • Samuel Saslaw Professor of Medicine • Chair, Department of Microbial Infection & Immunity • Director, Center for Microbial Interface Biology and the Medical Scientist Training Program • The Ohio State University • • Arthur Gutierrez-Hartmann, MD • Professor, Medicine-Endocrinology, Metab & Diabetes, Biochemistry and Molecular Genetics • Director, MSTP and PSTP • University of Colorado School of Medicine • • Alexander Adami • MD/PhD student • University of Connecticut School of Medicine • APSA Technology Committee Objectives MD or Residency/Fellowship Career in MD/PhD Research Program and Medicine What residency programs support physician scien3st training? What residency programs do MD/PhD graduates enter? Report on Residents AAMC data 2011-2013 • In 2013 3.4% of all active residents who are graduates from US MD-granting medical schools were MD-PhD graduates • Of those individuals (MD and MD-PhD) who completed residency training from 2004-2013, 15.9% currently hold a full-time faculty appointment at a US MD- granting medical school Report on Residents (AAMC data 2011-2013) 30.0% 25.0% * 20.0% * 15.0% * 2011 10.0% 2012 * * 2013 5.0% 0.0% Report on Residents (AAMC data 2011-2013) 4.0% * 3.5% 3.0% 2.5% 2.0% 1.5% 1.0% 2011 2012 0.5% 2013 0.0% National Data, Ranked by Specialty Paik, JAMA 302: 1271, 2009 Why do MD/PhD or MDs not pursue a career in research? Graduates did not have a good Private prac3ce becomes more experience in research and do arac3ve than academics not want to con3nue. -
M4 ELECTIVE/SUB-INTERNSHIP POLICIES Phases C – Year 4
M4 ELECTIVE/SUB-INTERNSHIP POLICIES Phases C – Year 4 Revised: 11/27/19 Page 1 of 14 Table of Contents M4 CNUCOM CONTACT INFORMATION....................................................................................... 3 OFFICE OF MEDICAL EDUCATION (OME)................................................................................ 3 Leadership ...................................................................................................................................... 3 Administrative Staff for Clinical Rotations ................................................................................... 3 Summary of M4 Elective/Sub-Internship Policies ................................................................................ 4 General Policies ..................................................................................................................................... 5 General Sub-Internships (Acting Internship) Policy.............................................................................. 6 Required Components:................................................................................................................... 6 Optional Components: ................................................................................................................... 6 Emergency Medicine Sub-Internships (Acting Internship) Policy ........................................................ 7 Definition of Home and Away Elective ................................................................................................ -

Definitions: Fellow/Resident: a Physician Who Is Engaged in A
Roles, Responsibilities and Patient Care Activities of Fellows ADOLESCENT MEDICINE FELLOWSHIP PROGRAM Definitions: Fellow/Resident: A physician who is engaged in a graduate training program in medicine (which includes all specialties) and who participates in patient care under the direction of attending physicians (or licensed independent practitioners) as approved by each review committee. Note: The term “resident” may also be used interchangeably with fellow for training and includes all residents and fellows including individuals in their first year of training (PGY1), often referred to as “interns,” and individuals in approved subspecialty graduate medical education programs who historically have also been referred to as “fellows.” As part of their training program, fellows are given graded and progressive responsibility according to the individual fellow’s clinical experience, judgment, knowledge, and technical skill. Each fellow must know the limits of his/her scope of authority and the circumstances under which he/she is permitted to act with conditional independence. Fellows are responsible for asking for help from the supervising physician (or other appropriate licensed practitioner) for the service they are rotating on when they are uncertain of diagnosis, how to perform a diagnostic or therapeutic procedure, or how to implement an appropriate plan of care. Attending of Record (Attending) An identifiable, appropriately-credentialed and privileged attending physician or licensed practitioner (as approved by each Review Committee) who is ultimately responsible for the management of the individual patient and for the supervision of the fellows involved in the care of the patient, The attending delegates portion of care to fellow based on the needs of the patient and the skills of the fellow. -
Senior Sub-Internship Pediatrics
Curriculum and Educational Policy Committee 539 Pediatric Subinternship This course satisfies the Sub Internship requirement for UC Irvine Students This rotation does not accept international students All students must get prior approval for all CHOC based rotations Course Name Pediatric Subinternship Course Director Behnoosh Afghani, MD Academic Year 2020-2021 1. Course Director, Coordinator and General Administrative Information FACULTY AND STAFF Name Office Location Phone Email Director: Behnoosh Afghani, Bldgg. 26 Ste. 714-456-5650 [email protected] MD 1001 Coordinator: Frank Cruz 505 S. Main St., 714-456-5650 [email protected] Ste. 525 DESCRIPTION Students spend four weeks as sub-interns during which time they carry the full ward responsibility of an intern on one-half the number of patients usually carried by an intern. The sub-internship is designed to improve clinical competence and to prepare the students for the challenges and demands of the internship. Students may choose between sub-internships in medicine, surgery or pediatrics. PREREQUISITES This course is intended for 3rd and 4th-year students enrolled in the undergraduate medical education program at University of California, Irvine School of Medicine (UCISOM). RESTRICTIONS This course is intended for 4th-year students enrolled in the undergraduate medical education program at University of California, Irvine School of Medicine (UCISOM). If this is going to be on the website for outside medical students, we will need to revise the section. COURSE DIRECTOR Dr. Afghani has worked in higher education since 1995. Behnoosh Afghani, MD, is Clinical Professor of Pediatrics at the UC Irvine School of Medicine. She received her Rev. -

Max Kade Clinical Clerkship Program in the USA
Max Kade Clinical Clerkship Program In the USA Experience Guide 2018/2019 MAX KADE FELLOWSHIP PROGRAM The American Austrian Foundation MKCC Experience Guide 2018/2019 1 1. Short information about this guide: .................................................................................................. 3 2. Students attended a rotation at UPENN: .......................................................................................... 3 A. A Day at PENN ............................................................................................................................................................. 3 B. Housing .......................................................................................................................................................................... 5 C. Recommendations - Which suggestions or recommendations do you have for future Max Kade students (hospital, leisure time, etc.) ......................................................................................................................... 6 D. Other – Is there any other vital information you would like to share with future Max Kade students? ................................................................................................................................................................................ 7 3. Students attended a rotation at GWU: .............................................................................................. 8 A. A Day at GWU .............................................................................................................................................................. -

Introduction to the Fellowship Guide
INTRODUCTION TO THE FELLOWSHIP GUIDE We are very excited that you are beginning to take the steps towards a sub-specialty career! As a program, we are dedicated to your success. As successful graduates of this program, you are our greatest ambassadors and recruiters that will bring the next generation of outstanding house staff to the University of Colorado. This guide was created to combine the expertise of the program directorate and the experiences of your colleagues into a concise document that will help to make you as competitive of a candidate as you can be. The fellowship application and interviewing experience can be confusing and stressful. This guide is just one piece of greater programmatic changes that we hope will provide clarity and minimize the stress associated with applying and interviewing for fellowship. The fellowship guide provides a longitudinal step-by-step description of the application process, obtaining and preparing for interviews, and the post-interview period leading up to your match day. Please know that Dr. Connors and your associate program directors (specifically your sub-specialty APDs- Lisa Davis, Brian Graham, and Mark Kearns) are here to support you and advocate for you throughout this process. Please do not hesitate to contact us with questions, concern, and needs. Many thanks are owed to prior authors of this guide, including: Suzanne Brandenburg; Brian Graham and the associate program directors; Nicole Canterbury and Jennifer Weber in the House staff office; and your colleagues whose insights and quotes are contained in the document. As you progress through the fellowship experience, I would welcome your feedback so that we can continue to update and improve this document for future University of Colorado residents applying for fellowship.