Options of Bipolar Muscle Transfers to Restore Deltoid Function: an Anatomical Study
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

By the Authors. These Guidelines Will Be Usefulas an Aid in Diagnosing
Kroeber Anthropological Society Papers, Nos. 71-72, 1990 Humeral Morphology of Achondroplasia Rina Malonzo and Jeannine Ross Unique humeral morphologicalfeatures oftwo prehistoric achondroplastic adult individuals are des- cribed. Thesefeatures are compared to the humerus ofa prehistoric non-achondroplastic dwarfand to the humeri ofa normal humanpopulation sample. A set ofunique, derived achondroplastic characteris- tics ispresented. The non-achondroplastic individual is diagnosed as such based on guidelines created by the authors. These guidelines will be useful as an aid in diagnosing achondroplastic individualsfrom the archaeological record. INTRODUCTION and 1915-2-463) (Merbs 1980). The following paper describes a set of humeral morphological For several decades dwarfism has been a characteristics which can be used as a guide to prominent topic within the study of paleopathol- identifying achondroplastic individuals from the ogy. It has been represented directly by skeletal archaeological record. evidence and indirectly by artistic representation in the archaeological record (Hoffman and Brunker 1976). Several prehistoric Egyptian and MATERIALS AND METHODS Native American dwarfed skeletons have been recorded, indicating that this pathology is not A comparative population sample, housed by linked solely with modem society (Brothwell and the Lowie Museum of Anthropology (LMA) at Sandison 1967; Hoffman and Brunker 1976; the University of California at Berkeley, was Niswander et al. 1975; Snow 1943). Artifacts derived from a random sample forming a total of such as paintings, tomb illustrations and statues sixty adult individuals (thirty males and thirty of dwarfed individuals have been discovered in females) from six different prehistoric ar- various parts of the world. However, interpreta- chaeological sites within California. Two tions of such artifacts are speculative, for it is achondroplastic adult individuals from similar necessary to allow artistic license for individualis- contexts, specimen number 6670 (spc. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Trapezius Origin: Occipital Bone, Ligamentum Nuchae & Spinous Processes of Thoracic Vertebrae Insertion: Clavicle and Scapul
Origin: occipital bone, ligamentum nuchae & spinous processes of thoracic vertebrae Insertion: clavicle and scapula (acromion Trapezius and scapular spine) Action: elevate, retract, depress, or rotate scapula upward and/or elevate clavicle; extend neck Origin: spinous process of vertebrae C7-T1 Rhomboideus Insertion: vertebral border of scapula Minor Action: adducts & performs downward rotation of scapula Origin: spinous process of superior thoracic vertebrae Rhomboideus Insertion: vertebral border of scapula from Major spine to inferior angle Action: adducts and downward rotation of scapula Origin: transverse precesses of C1-C4 vertebrae Levator Scapulae Insertion: vertebral border of scapula near superior angle Action: elevates scapula Origin: anterior and superior margins of ribs 1-8 or 1-9 Insertion: anterior surface of vertebral Serratus Anterior border of scapula Action: protracts shoulder: rotates scapula so glenoid cavity moves upward rotation Origin: anterior surfaces and superior margins of ribs 3-5 Insertion: coracoid process of scapula Pectoralis Minor Action: depresses & protracts shoulder, rotates scapula (glenoid cavity rotates downward), elevates ribs Origin: supraspinous fossa of scapula Supraspinatus Insertion: greater tuberacle of humerus Action: abduction at the shoulder Origin: infraspinous fossa of scapula Infraspinatus Insertion: greater tubercle of humerus Action: lateral rotation at shoulder Origin: clavicle and scapula (acromion and adjacent scapular spine) Insertion: deltoid tuberosity of humerus Deltoid Action: -
Bones of the Upper and Lower Limb Musculoskeletal Block - Lecture 1
Bones of the Upper and Lower limb Musculoskeletal Block - Lecture 1 Objective: Classify the bones of the three regions of the lower limb (Thigh, leg and foot). Memorize the main features of the – Bones of the thigh (femur & patella) – Bones of the leg (tibia & Fibula) – Bones of the foot (tarsals, metatarsals and phalanges) Recognize the side of the bone. Color index: Important In male’s slides only In female’s slides only Extra information, explanation Editing file Click here for Contact us: useful videos [email protected] Please make sure that you’re familiar with these terms Terms Meaning Example Ridge The long and narrow upper edge, angle, or crest of something The supracondylar ridges (in the distal part of the humerus) Notch An indentation, (incision) on an edge or surface The trochlear notch (in the proximal part of the ulna) Tubercles A nodule or a small rounded projection on the bone (Dorsal tubercle in the distal part of the radius) Fossa A hollow place (The Notch is not complete but the fossa is Subscapular fossa (in the concave part of complete and both of them act as the lock of the joint the scapula) Tuberosity A large prominence on a bone usually serving for Deltoid tuberosity (in the humorous) and it the attachment of muscles or ligaments ( is a bigger projection connects the deltoid muscle than the Tubercle ) Processes A V-shaped indentation (act as the key of the joint) Coracoid process ( in the scapula ) Groove A channel, a long narrow depression sure Spiral (Radial) groove (in the posterior aspect of (the humerus -
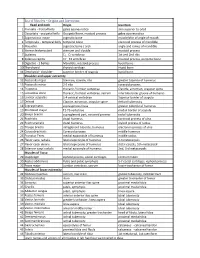
List of Muscles – Origins and Insertions
List of Muscles – Origins and Insertions: Head and neck Origin Insertion 1 Frontalis - frontal belly galea aponeurotica skin superior to orbit 2 Occipitalis - occipetal belly Occipetal bone, mastoid process galea aponeurotica 3 Zygomaticus major zygmatic bone muscle/skin of angle of mouth 4 Temporalis - temporal belly temporal bone coronoid process of mandible 5 Masseter zygmatic bone / arch angle and ramus of mandible 6 Sternocleidomastoid sternum and clavicle mastoid process 7 Scalenes C3 - C7 vertebrae 1st and 2nd ribs 8 Splenius capitis C7 - T4 vertebrae mastoid process, occipetal bone 9 Digastric - 2 bellies Mandible, mastoid process hyoid bone 10 Thyrohyoid thyroid cartilage Hyoid bone 11 Omohyoid - shoulder superior border of scapula hyoid bone Shoulder and upper extremity 12 Pectoralis major Sternum, clavicle, ribs greater tubercle of humerus 13 Pectoralis minor 2-5 ribs coracoid process 14 Trapezius thoracic / lumbar vertebrae Clavicle, acromion, scapular spine 15 Latissimus dorsi thoracic / lumbar vertebrae, sacrum intertubercular groove of humerus 16 Levator scapulae 1-4 cervical vertebrae Superior border of scapula 17 Deltoid Clavicle, acromion, scapular spine deltoid tuberosity 18 Supraspinatus supraspinous fossa greater tubercle of humerus 19 Rhomboid major T2-T5 vertebrae medial border of scapula 20 Biceps brachii supraglenoid part, coracoid process radial tuberosity 21 Brachialis distal humerus coronoid process of ulna 22 Brachioradialis distal humerus styloid process of radius 23 Triceps brachii infraglenoid tubercle, -

Muscles of the Upper Limb.Pdf
11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles of the Upper Limb Pectoralis minor ORIGIN: INNERVATION: anterior surface of pectoral nerves ribs 3 – 5 ACTION: INSERTION: protracts / depresses scapula coracoid process (scapula) (Anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Serratus anterior Subclavius ORIGIN: INNERVATION: ORIGIN: INNERVATION: ribs 1 - 8 long thoracic nerve rib 1 ---------------- INSERTION: ACTION: INSERTION: ACTION: medial border of scapula rotates scapula laterally inferior surface of scapula stabilizes / depresses pectoral girdle (Lateral view) (anterior view) Muscles Stabilizing Pectoral Girdle Muscles Stabilizing Pectoral Girdle Trapezius Levator scapulae ORIGIN: INNERVATION: ORIGIN: INNERVATION: occipital bone / spinous accessory nerve transverse processes of C1 – C4 dorsal scapular nerve processes of C7 – T12 ACTION: INSERTION: ACTION: INSERTION: stabilizes / elevates / retracts / upper medial border of scapula elevates / adducts scapula acromion / spine of scapula; rotates scapula lateral third of clavicle (Posterior view) (Posterior view) 1 11/8/2012 Muscles Stabilizing Pectoral Girdle Muscles Moving Arm Rhomboids Pectoralis major (major / minor) ORIGIN: INNERVATION: ORIGIN: INNERVATION: spinous processes of C7 – T5 dorsal scapular nerve sternum / clavicle / ribs 1 – 6 dorsal scapular nerve INSERTION: ACTION: INSERTION: ACTION: medial border of scapula adducts / rotates scapula intertubucular sulcus / greater tubercle flexes / medially rotates / (humerus) adducts -

Functional Anatomy of the Shoulder Glenn C
Journal ofAthletic Training 2000;35(3):248-255 C) by the National Athletic Trainers' Association, Inc www.journalofathletictraining.org Functional Anatomy of the Shoulder Glenn C. Terry, MD; Thomas M. Chopp, MD The Hughston Clinic, Columbus, GA Objective: Movements of the human shoulder represent the nents. Bony anatomy, including the humerus, scapula, and result of a complex dynamic interplay of structural bony anat- clavicle, is described, along with the associated articulations, omy and biomechanics, static ligamentous and tendinous providing the clinician with the structural foundation for under- restraints, and dynamic muscle forces. Injury to 1 or more of standing how the static ligamentous and dynamic muscle these components through overuse or acute trauma disrupts forces exert their effects. Commonly encountered athletic inju- this complex interrelationship and places the shoulder at in- ries are discussed from an anatomical standpoint. creased risk. A thorough understanding of the functional anat- Conclusions/Recommendations: Shoulder injuries repre- omy of the shoulder provides the clinician with a foundation for sent a significant proportion of athletic injuries seen by the caring for athletes with shoulder injuries. medical provider. A functional understanding of the dynamic Data Sources: We searched MEDLINE for the years 1980 to interplay of biomechanical forces around the shoulder girdle is 1999, using the key words "shoulder," "anatomy," "glenohu- necessary and allows for a more structured approach to the meral joint," "acromioclavicular joint," "sternoclavicular joint," treatment of an athlete with a shoulder injury. "scapulothoracic joint," and "rotator cuff." Key Words: anatomy, static, dynamic, stability, articulation Data Synthesis: We examine human shoulder movement by breaking it down into its structural static and dynamic compo- M ovements of the human shoulder represent a complex BONY ANATOMY dynamic relationship of many muscle forces, liga- ment constraints, and bony articulations. -

Shoulder Anatomy
ShoulderShoulder AnatomyAnatomy www.fisiokinesiterapia.biz ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy ClavicleClavicle – Sternal end – Acromion end ScapulaScapula Acromion – Surfaces end Sternal Costal end Dorsal – Borders – Angles ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy Scapula 1. spine 2. acromion 3. superior border 4. supraspinous fossa 5. infraspinous fossa 6. medial (vertebral) border 7. lateral (axillary) border 8. inferior angle 9. superior angle 10. glenoid fossa (lateral angle) 11. coracoid process 12. superior scapular notch 13 subscapular fossa 14. supraglenoid tubercle 15. infraglenoid tubercle ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – head – anatomical neck – greater tubercle – lesser tubercle – greater tubercle – lesser tubercle – intertubercular sulcus (AKA bicipital groove) – deltoid tuberosity ShoulderShoulder ComplexComplex BoneBone AnatomyAnatomy HumerousHumerous – Surgical Neck – Angle of Inclination 130-150 degrees – Angle of Torsion 30 degrees posteriorly ShoulderShoulder ComplexComplex ArticulationsArticulations SternoclavicularSternoclavicular JointJoint – Sternal end of clavicle with manubrium/ 1st costal cartilage – 3 degree of freedom – Articular Disk – Ligaments Capsule Anterior/Posterior Sternoclavicular Ligament Interclavicular Ligament Costoclavicular Ligament ShoulderShoulder ComplexComplex ArticulationsArticulations AcromioclavicularAcromioclavicular JointJoint – 3 degrees of freedom – Articular Disk – Ligaments Superior/Inferior -
Bones of Upper Limb
BONES OF THE UPPER LIMB Dr. Jamila El-Medany OBJECTIVES At the end of the lecture, students should be able to: List the different bones of the UL. List the characteristic features of each bone. Differentiate between the bones of the right and left sides. List the articulations between the different bones. The Bones of UL are: Pectoral Girdle. Arm : Humerus. Forearm : Radius & Ulna. Wrist : Carpal bones Hand: Metacarpals & Phalanges Pectoral Girdle Formed of Two Bones: Clavicle (anteriorly) and Scapula (posteriorly). It is very light and allows the upper limb to have exceptionally free movement. Clavicle It is a doubly curved long bone lying horizontally across the root of the neck It is subcutaneous throughout its length. Functions: 1. It serves as a rigid support from which the scapula and free upper limb are suspended & keep them away from the trunk so that the arm has maximum freedom of movement. 2. Transmits forces from the upper limb to the axial skeleton. 3. Provides attachment for muscles. 4. It forms a boundary of the Cervicoaxillary canal for protection of the neurovascular bundle of the UL. Clavicle It is a long bone with no medullary cavity. It has the appearance of an elongated letter Capital (S) lying on one side. It has Two Ends: Medial (Sternal) : enlarged & triangular. Lateral (Acromial) : flattened. Body (shaft): Its medial 2/3 is convex forward. Its lateral 1/3 is concave forward. Surfaces: Superior : smooth as it lies just deep to the skin. Inferior : rough because strong ligaments bind it to the 1st rib. Articulations of Clavicle Medially with the manubrium at the Sternoclavicular joint . -

The Deltoid, a Forgotten Muscle of the Shoulder
Skeletal Radiol DOI 10.1007/s00256-013-1667-7 REVIEW ARTICLE The deltoid, a forgotten muscle of the shoulder Thomas Moser & Junie Lecours & Johan Michaud & Nathalie J. Bureau & Raphaël Guillin & Étienne Cardinal Received: 17 February 2013 /Revised: 29 May 2013 /Accepted: 30 May 2013 # ISS 2013 Abstract The deltoid is a fascinating muscle with a signif- Keywords Deltoid muscle . Shoulder . Anatomy . Tears . icant role in shoulder function. It is comprised of three Nerve injuries distinct portions (anterior or clavicular, middle or acromial, and posterior or spinal) and acts mainly as an abductor of the shoulder and stabilizer of the humeral head. Deltoid tears are Introduction not infrequently associated with large or massive rotator cuff tears and may further jeopardize shoulder function. A variety The deltoid is an essential, although lesser considered, muscle of other pathologies may affect the deltoid muscle including of the shoulder and thus it is rarely mentioned in MRI reports, enthesitis, calcific tendinitis, myositis, infection, tumors, and which tend to focus on rotator cuff tendon and muscles. chronic avulsion injury. Contracture of the deltoid following In this paper, we aimed to review the normal anatomy and repeated intramuscular injections could present with pro- function of the deltoid muscle and to describe imaging gressive abduction deformity and winging of the scapula. features of various pathologies. The deltoid muscle and its innervating axillary nerve may be injured during shoulder surgery, which may have disastrous functional consequences. Axillary neuropathies leading to del- Anatomy and function toid muscle dysfunction include traumatic injuries, quadrilat- eral space and Parsonage–Turner syndromes, and cause dener- Overview and functional anatomy vation of the deltoid muscle. -
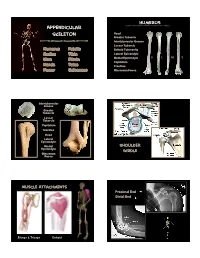
Appendicular Skeleton
Humerus Appendicular Skeleton Head Greater Tubercle Intertubercular Groove Lesser Tubercle Humerus Patella Deltoid Tuberosity Radius Tibia Lateral Epicondyle D L M V Ulna Fibula Medial Epicondyle Capitulum Hands Talus Trochlea Femur Calcaneus Olecrenon Fossa Intertubercular Groove Greater Tubercle Lesser Tubercle Capitulum Trochlea Head Lateral Epicondyle Medial Shoulder Epicondyle Girdle Olecrenon Fossa Muscle Attachments Proximal End Distal End Biceps & Triceps Deltoid 1 Radius Ulna Head Neck Radial Tuberosity Interosseous Crest Styloid Process Olecrenon Process Ulnar Notch Radial Notch Tuberosity L M D V Styloid Process D L M V Interosseous Crest Trochlea Radial Tuberosity Olecrenon Process Capitulum Head Medial Epicondyle Phalanges 1st 3rd Proximal Phalange 3rd Metacarpals 1st Proximal Phalange 2 Femur Head, medial Larger epicondyle, lateral Femur head Olecrenon fossa, distal Fovea capitus Olecrenon process, proximal Greater trochanter Radial notch, lateral Lesser trochanter Styloid process, towards ‘pinky’ Linea aspera Head, proximal Medial condyle Tuberosity, medial Lateral condyle Styloid towards thumb Intercondylar fossa V D L M Patellar articular surface Proximal Femur Fovea capitus Trochanteric Fossa Greater Trochanter Lesser femur humerus Trochanter Proximal Femur Medial condyle Lateral condyle Patella Patellar articular surface Intercondylar notch V D Apex Base Facet for lateral femoral condyle Distal Femur Facet for medial femoral condyle 3 Tibia Tibia Lateral condyle Lateral condyle Medial condyle Medial condyle Fibular -
Lab Manual Appendicular Skele
1 PRE-LAB EXERCISES When studying the skeletal system, the bones are often sorted into two broad categories: the axial skeleton and the appendicular skeleton. This lab focuses on the appendicular skeleton, which is formed from the pectoral and pelvic girdles and the upper and lower limbs. View Module 7.2 Axial and Appendicular Skeleton to highlight the bones of the appendicular skeleton and compare them to those of the axial skeleton. Examine Module 11.1 Appendicular Skeleton to view only the bones of the appendicular skeleton. In addition to learning about all the bones of the appendicular skeleton, it is also important to identify some significant bone markings. Bone markings can have many shapes, including holes, round or sharp projections, and shallow or deep valleys, among others. These markings on the bones serve many purposes, including forming attachments to other bones or muscles and allowing passage of a blood vessel or nerve. It is helpful to understand the meanings of some of the more common bone marking terms. Before we get started, look up the definitions of these common bone marking terms: Canal: Condyle: Facet: Fissure: Foramen: (see Module 10.18 Foramina of Skull) Fossa: Margin: Process: Proximal: Trochanter: Tubercle: Tuberosity: Throughout this exercise, you will notice bold terms. This is meant to focus your attention on these important words. Make sure you pay attention to any bold words and know how to explain their definitions and/or where they are located. Use the following modules to guide your exploration of the appendicular skeleton. As you explore these bones in Visible Body’s app, also locate the bones and bone markings on any available charts, models, or specimens.