Pathogenesis of Bone Erosions in Rheumatoid Arthritis: Not Only
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
CORRECTION of DEFORMITIES of the JAW by Patrick Clarkson M.B.E., M.B., B.S., F.R.C.S
CORRECTION OF DEFORMITIES OF THE JAW by Patrick Clarkson M.B.E., M.B., B.S., F.R.C.S. Casualty Surgeon, Guy's Hospital and Plastic Surgeon, Basingstoke Plastic;Ccntre. I. INTRODUCTION Degrees of Deformity and Pathology. Cooperation between Surgeon and Orthodontist. Surgical Treatment: Indication and Scope. Choice between radical surgery and " masking" operations. II. SURGICAL METHODS OF CORRECTION 1. Symmetrical Prognathism of the Mandible. 2. Asymmetrical Prognathism of the Mandible. 3. Symmetrical Recession of the Mandible. 4. Asymmetrical Recession of the Mandible. 5. The Jaw Deformities in Cleft Palate: Mandible and Maxilla. 6. Combined Jaw and Nasal Reductions. III. SUMMARY AND CONCLUSION I. INTRODUCTION A deformity of the jaw can be defined as any variation in these bones from the normal for the sex, age, and race of the patient; but only rela- tively gross variations come within the field of surgical repair. It is always possible by close examination to discover some degree of asymmetry in soft and bony tissues of the face, but the great majority of variations in facial skeleton, both symmetrical and unilateral, are scarcely noticeable to ordinary examination and require no treatment. Next in order of severity are a group of congenital origin which, given early and full ortho- dontic treatment, respond well without the need of surgery. This group includes a few of the early-cases of prognathism, of congenital open bite, and of recession of the jaw. Almost every case with these deformities can be improved by early orthodontic treatment. But all the more severe cases of prognathism, of recession, and the jaw deformities seen in patients with cleft palate, need surgical intervention if the correction is to be a complete one. -

Gender Reassignment Surgery Policy Number: PG0311 ADVANTAGE | ELITE | HMO Last Review: 07/01/2021
Gender Reassignment Surgery Policy Number: PG0311 ADVANTAGE | ELITE | HMO Last Review: 07/01/2021 INDIVIDUAL MARKETPLACE | PROMEDICA MEDICARE PLAN | PPO GUIDELINES This policy does not certify benefits or authorization of benefits, which is designated by each individual policyholder terms, conditions, exclusions and limitations contract. It does not constitute a contract or guarantee regarding coverage or reimbursement/payment. Self-Insured group specific policy will supersede this general policy when group supplementary plan document or individual plan decision directs otherwise. Paramount applies coding edits to all medical claims through coding logic software to evaluate the accuracy and adherence to accepted national standards. This medical policy is solely for guiding medical necessity and explaining correct procedure reporting used to assist in making coverage decisions and administering benefits. SCOPE X Professional X Facility DESCRIPTION Transgender is a broad term that can be used to describe people whose gender identity is different from the gender they were thought to be when they were born. Gender dysphoria (GD) or gender identity disorder is defined as evidence of a strong and persistent cross-gender identification, which is the desire to be, or the insistence that one is of the other gender. Persons with this disorder experience a sense of discomfort and inappropriateness regarding their anatomic or genetic sexual characteristics. Individuals with GD have persistent feelings of gender discomfort and inappropriateness of their anatomical sex, strong and ongoing cross-gender identification, and a desire to live and be accepted as a member of the opposite sex. Gender Dysphoria (GD) is defined by the Diagnostic and Statistical Manual of Mental Disorders - Fifth Edition, DSM-5™ as a condition characterized by the "distress that may accompany the incongruence between one’s experienced or expressed gender and one’s assigned gender" also known as “natal gender”, which is the individual’s sex determined at birth. -

Effects of Tofacitinib in Early Arthritis-Induced Bone Loss in an Adjuvant-Induced Arthritis Rat Model
Effects of tofacitinib in early arthritis-induced bone loss in an adjuvant-induced arthritis rat model Vidal B.1, Cascão R.1, Finnilä MA.2,3, IP. Lopes1, da Glória VG.1, Saarakkala S.2,4, Zioupos P.5, Canhão H.6, Fonseca JE.1,7 1 Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Lisbon, Portugal; 2 Research Unit of Medical Imaging, Physics and Technology, Faculty of Medicine, University of Oulu, Oulu, Finland; 3 Department of Applied Physics, University of Eastern Finland, Kuopio, Finland; 4 Medical Research Center, University of Oulu, Oulu, Finland; 5 Biomechanics Labs, Cranfield Forensic Institute, Cranfield University, DA of the UK; ; 6 EpiDoC Unit, CEDOC, NOVA Medical School, NOVA University, Lisbon, Portugal; 7 Rheumatology Department, Centro Hospitalar de Lisboa Norte, EPE, Hospital de Santa Maria, Lisbon Academic Medical Centre, Lisbon, Portugal ABSTRACT Rheumatoid arthritis (RA) causes immune mediated local and systemic bone damage. Objectives - The main goal of this work was to analyze, how treatment intervention with tofacitinib prevents the early disturbances on bone structure and mechanics in adjuvant induced arthritis rat model. This is the first study to access the impact of tofacitinib on the systemic bone effects of inflammation. Methods - Fifty Wistar adjuvant-induced arthritis (AIA) rats were randomly housed in experimental groups, as follows: non-arthritic healthy group (N=20), arthritic non-treated (N=20) and 10 animals under tofacitinib treatment. Rats were monitored during 22 days after disease induction for the inflammatory score, ankle perimeter and body weight. Healthy non-arthritic rats were used as controls for comparison. After 22 days of disease progression rats were sacrificed and bone samples were collected for histology, micro computed tomography (micro-CT), 3-point bending and nanoindentation analysis. -

Imaging in Psoriatic Arthritis
Review Standardizing the monitoring of outcome measures: imaging in psoriatic arthritis The wide spectrum of manifestations of musculoskeletal inflammation in psoriatic arthritis makes standardized assessment of joint damage in psoriatic arthritis a challenge. Assessment of erosions and joint space narrowing on plain radiographs of the hands and feet has remained the benchmark for assessing damage in psoriatic arthritis. The methods used to assess damage have been mostly borrowed from those used in rheumatoid arthritis. Axial joint involvement has not been systematically addressed. Methods to assess spinal disease have been borrowed from those used in ankylosing spondylitis. Both ultrasound and MRI have demonstrated promise in the assessment of psoriatic arthritis. The Outcome Measures in Rheumatology Clinical Trials (OMERACT) group is involved in the development of valid, reliable and feasible methods for assessment of joint involvement in psoriatic arthritis. † KEYWORDS: inflammation n joint damage n MRI n psoriasis n radiography Dafna D Gladman n spondylitis n ultrasonography n validation & Vinod Chandran1 1Psoriatic Arthritis Program, University Health Network, 1E 412, 399 Bathurst Psoriatic arthritis (PsA) is an inflammatory and validates outcome measures in rheumato- Street, Toronto, Ontario, M5T 2S8, musculo skeletal disease associated with psoria- logy, identified several measures that should be Canada †Author for correspondence: sis [1]. Psoriasis is an inflammatory, immune- assessed in patients with PsA [6]. These include University -
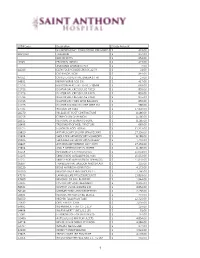
CPT4 Code Descrip1on Charge Amount NICARDIPINE HCL 20MG
CPT4 Code Descripon Charge Amount NICARDIPINE HCL 20MG/200ML PRE-MIXED IV $ 419.00 A9270GY TRAVATAN $ 354.00 BAYHEP B PFS $ 653.00 J1645 FRAGMIN 18000U $ 423.00 AMMONIA AROMATIC INH $ 4.00 A4340 CATH FOLEY COUDE LTX 5CC 22 FR $ 31.00 CLIP RESOLUTION $ 844.00 A4351 CATHETER URETHRAL BARDIA 14 FR $ 27.00 64832 REPAIR NERVE ADD ON $ 417.00 C1726 BALLOON HERCULES 15-16.5-18MM $ 663.00 C1726 DILATOR BAL CRE SGL USE FIXED $ 855.00 C1726 DILATOR BAL CRE SGL USE FIXED $ 855.00 C1726 DILATOR BAL CRE SGL USE FIXED $ 855.00 C1726 DILATOR CRE FIXED WIRE BALLOON $ 855.00 C1726 DILATOR COLONIC BAL CRE WIRE GU $ 986.00 27705 INCISION OF TIBIA $ 17,350.00 28270 RELEASE OF FOOT CONTRACTURE $ 8,186.00 28296 CORRECTION OF BUNION $ 8,186.00 28315 REMOVAL OF SESAMOID BONE $ 8,186.00 28405 TREATMENT OF HEEL FRACTURE $ 665.00 28725 FUSION OF FOOT BONES $ 31,327.00 29820 ARTHROSCOPY SHLDRR SYNOVEC PAR $ 17,350.00 29824 SHOULDER ARTHROSCOPY MUMFORD $ 8,186.00 29826 SHOULDER ARTHROSCOPY/SURGERY $ 1,440.00 29827 ARTHROSCOP ROTATOR CUFF REPR $ 17,350.00 29894 ANKLE ARTHROSCOPY/SURGERY $ 8,186.00 31254 REVISION OF ETHMOID SINUS $ 15,053.00 31295 SINUS ENDO W/BALLON DIL MAX $ 15,053.00 31297 SINUS ENDO W/BALLON DIL SPHENOID $ 15,053.00 36907 TRANSLUMINAL BALLOON ANGIOPLAST $ 235.00 38220 BONE MARROW ASPIRATION $ 4,172.00 46260 REMOVE IN/EX HEM GROUPS 2+ $ 7,166.00 47379 LAPAROSCOPE PROCEDURE LIVER $ 13,891.00 47600 REMOVAL OF GALLBLADDER $ 1,944.00 52235 CYSTOSCOPY AND TREATMENT $ 8,346.00 56501 DESTROY VULVA LESIONS SIM $ 4,854.00 58140 MYOMECTOMY ABDOM METHOD $ 2,156.00 -

IL-1Β-Driven Osteoclastogenic T Regulatory Cells Accelerate Bone Erosion in Arthritis
IL-1β-driven osteoclastogenic T regulatory cells accelerate bone erosion in arthritis Anaïs Levescot, … , Julia F. Charles, Peter A. Nigrovic J Clin Invest. 2021. https://doi.org/10.1172/JCI141008. Research In-Press Preview Autoimmunity Inflammation Graphical abstract Find the latest version: https://jci.me/141008/pdf Osteoclastogenic Tregs IL-1-driven osteoclastogenic T regulatory cells accelerate bone erosion in arthritis Anaïs Levescot1, Margaret H. Chang1,2, Julia Schnell1,3, Nathan Nelson-Maney1, Jing Yan1,4, Marta Martínez-Bonet1, Ricardo Grieshaber-Bouyer1, Pui Y. Lee1,2, Kevin Wei1, Rachel B. Blaustein1, Allyn Morris1, Alexandra Wactor1, Yoichiro Iwakura5, James A. Lederer6, Deepak A. Rao1, Julia F. Charles1,4, and Peter A. Nigrovic1,2 1Division of Rheumatology, Inflammation, and Immunity, Brigham and Women’s Hospital, Boston MA, USA 2Division of Immunology, Boston Children’s Hospital, Boston MA, USA 3Department of Medicine V, Hematology, Oncology and Rheumatology, Heidelberg University Hospital, Heidelberg, Germany 4Department of Orthopaedic Surgery, Brigham and Women’s Hospital, Boston MA, USA 5Center for Experimental Animal Models, Research Institute for Science & Technology, Tokyo University of Science, Tokyo, Japan 6Department of Surgery, Brigham and Women’s Hospital, Boston MA, USA Correspondence: Peter A. Nigrovic, MD Chief, Division of Immunology Boston Children’s Hospital Karp Family Research Building, Room 10211 One Blackfan Circle Boston, MA 02115 Ph: 617-905-1373 Email: [email protected] All authors declare no related conflicts of interest. 1 Osteoclastogenic Tregs Abstract IL-1 is a pro-inflammatory mediator with roles in innate and adaptive immunity. Here we show that IL-1 contributes to autoimmune arthritis by inducing osteoclastogenic capacity in T regulatory cells (Tregs). -

Assurant Health and Welfare Plan 2019 Summary Plan Description
Assurant Health and Welfare Plan 2019 Summary Plan Description October 8, 2018 New York, NY Main Table of Contents Getting to Know Your Assurant Benefits .....................................................3 Assurant Health and Welfare Plan ..............................................................4 Assurant Health Plan ...................................................................................14 Prescription Drug Coverage.........................................................................57 Employee Assistance Program .....................................................................64 Dental Plan ..................................................................................................67 Flexible Spending Accounts ........................................................................77 Life and Accident Insurance ........................................................................89 Disability Plan .............................................................................................106 Group Insurance ..........................................................................................120 Tuition Reimbursement Plan .......................................................................125 Commuter Benefits Program .......................................................................130 Severance Pay Plan .....................................................................................132 Plan Administration .....................................................................................137 -

Medi-Cal Surgical Services for Transgender
Medi-Cal Managed Care L.A. Care Clinical Guideline Subject: Medi-Cal Managed Care (Medi-Cal) Surgical Services for Transgender Beneficiaries Status: Annual review Current Effective Date: January 1, 2019 Last Review Date: February 3, 2020 Definition California Medi-Cal managed health care plans (MCPs) must provide medically necessary covered services to all Medi-Cal beneficiaries, including transgender beneficiaries. Medically necessary covered services are those services “which are reasonable and necessary to protect life, to prevent significant illness or significant disability, or to alleviate severe pain through the diagnosis and treatment of disease, illness or injury” (Title 22 California Code of Regulations § 51303). The California Department of Health Care Services (DHCS) recognizes the Affordable Care Act (ACA) and the implementing regulations as prohibiting discrimination against transgender beneficiaries. MCPs are required to treat beneficiaries consistent with their gender identity (Title 42 United States Code § 18116; 45 Code of Federal Regulations (CFR) §§ 92.206, 92.207; see also 45 CFR § 156.125 (b)). Federal regulations prohibit MCPs from denying or limiting coverage of any health care services that are ordinarily or exclusively available to beneficiaries of one gender, to a transgender beneficiary based on the fact that a beneficiary’s gender assigned at birth, gender identity, or gender otherwise recorded is different from the one to which such services are ordinarily or exclusively available (45 CFR §§ 92.206, 92.207(b)(3)). DHCS indicates that Federal regulations further prohibit MCPs from categorically excluding or limiting coverage for health care services related to gender transition (45 CFR § 92.207(b)(4)). The insurance Gender Nondiscrimination Act (IGNA) prohibits MCPs from discriminating against individuals based on gender, including gender identity or gender expression (Health and Safety Code Section (§)1365.5). -
A Systematic Approach to Differentiating Joint Disorders A
MedicalContinuing Education PODIATRIC RADIOGRAPHY Objectives After completing this mate- rial the reader shall be able to: 1) List the radiographic criteria for systematically evaluating joints and joint disease. 2) Define: joint effusion, AA SystematicSystematic arthritis mutilans, and en- thesopathy. 3) List common joint dis- ApproachApproach toto orders that are associated with arthritis. 4) Explain the importance DifferentiatingDifferentiating of a lesion (erosion, for exam- ple) having either a well- defined or ill-defined margin. JointJoint DisordersDisorders 5) List target areas in the foot and calcaneus for com- X-rays can be an important mon arthritic disorders. 6) Distinguish between tool in confirming your the joint disorders (based diagnosis. on radiographic findings). Welcome to Podiatry Management’s CME Instructional program. Our journal has been approved as a sponsor of Contin- uing Medical Education by the Council on Podiatric Medical Education. You may enroll: 1) on a per issue basis (at $17.50 per topic) or 2) per year, for the special introductory rate of $109 (you save $66). You may submit the answer sheet, along with the other information requested, via mail, fax, or phone. In the near future, you may be able to submit via the Internet. If you correctly answer seventy (70%) of the questions correctly, you will receive a certificate attesting to your earned cred- its. You will also receive a record of any incorrectly answered questions. If you score less than 70%, you can retake the test at no additional cost. A list of states currently honoring CPME approved credits is listed on pg. 246. Other than those entities cur- rently accepting CPME-approved credit, Podiatry Management cannot guarantee that these CME credits will be acceptable by any state licensing agency, hospital, managed care organization or other entity. -

Denosumab, Cortical Bone and Bone Erosion in Rheumatoid Arthritis
Correspondence response Ann Rheum Dis: first published as 10.1136/annrheumdis-2016-210027 on 23 August 2016. Downloaded from Response to: ‘Denosumab, cortical bone Correspondence to Professor Tsutomu Takeuchi, Division of Rheumatology, Department of Internal Medicine, Keio University School of Medicine, and bone erosion in rheumatoid arthritis’ 35 Shinanomachi, Shinjuku-ku, Tokyo 160-8582, Japan; by Rossini et al [email protected] Competing interests None declared. Dear Editor, Provenance and peer review Commissioned; internally peer reviewed. We thank Rossini et al for their comments1 on our recent study on inhibitory effect by denosumab on the progression of bone erosions in Japanese patients with rheumatoid arthritis (RA).2 They addressed their observation from point of view of bone in patient with RA. We think their view brings treatment of RA To cite Takeuchi T, Tanaka Y, Ishiguro N, et al. Ann Rheum Dis 2016;75:e71. closer to treatment of osteoporosis. Accepted 3 August 2016 Activated osteoclasts decrease bone mineral density (BMD) and stimulate bone erosion in patients with RA.3 Receptor activator of nuclear factor kappa-B ligand (RANKL) promotes osteoclast dif- – ferentiation, maturation, and activation.4 7 Denosumab is a fully human monoclonal antibody against RANKL that inhibits osteo- ▸ http://dx.doi.org/10.1136/annrheumdis-2016-210022 clast formation, function, and survival. Denosumab treatment increases BMD in cortical and trabecular bone. In addition, deno- Ann Rheum Dis 2016;75:e71. doi:10.1136/annrheumdis-2016-210027 sumab has been shown to improve cortical bone microstructure in subjects with osteoporosis or low bone mass.89 REFERENCES Increases in lumbar spine and total hip BMD and inhibition 1 Rossini M, Adami G, Viapiana O, et al. -

Association with Its Bone Mineral Density by HR-Pqct in Rheumatoid Arthritis Patients Camille P
Figueiredo et al. BMC Musculoskeletal Disorders (2021) 22:109 https://doi.org/10.1186/s12891-021-03992-5 RESEARCH ARTICLE Open Access Bone erosion in the 2nd metacarpophalangeal head: association with its bone mineral density by HR-pQCT in rheumatoid arthritis patients Camille P. Figueiredo1* , Mariana O. Perez1, Lucas Peixoto Sales1, Ana Cristina Medeiros2, Valeria F. Caparbo1 and Rosa M. R. Pereira1,2* Abstract Background: Rheumatoid arthritis (RA) is a chronic autoimmune disease depicted by synovial inflammation leading to local and systemic bone loss. The aim of this study was to evaluate by a HR-pQCT (High Resolution Peripheral Quantitative Computed Tomography) study which parameters are associated with volume of bone erosions including bone mineral density (BMD) around erosions (VOI 1 to 4 = volume of interest), BMD of metacarpophalangeal (MCP) head, BMD of radius, presence of osteophytes and joint space width (JSW). Methods: Fifty female RA patients (18–50 years) were enrolled in this study. Demographic and disease-specific data, laboratory inflammatory parameters and handgrip test were performed. All patients underwent HR-pQCT of 2nd and 3rd MCP joints and distal radius, according to established protocols. The volume of bone erosions was evaluated by MIAF (Medical Image Analysis Framework) software. Osteophytes were analyzed by manual method. Results: The mean of age and disease duration were 40.0 ± 6.0 yrs. and 10.8 ± 4.8 yrs., respectively. According to DAS- 28 (Disease Activity Score), 54% (27) of the sample were in remission. However, when SDAI (Simplified Disease Activity Index) was used, only 18% (9) were under remission. The mean of HAQ (Health Assessment Questionnaire), ESR (Erythrocyte sedimentation rate) and CRP (C reactive protein) were 0.9 ± 0.7, 13.9 ± 12.2 mm and 5.6 ± 7.5 mg/mL, respectively. -

Dartmouth Student Group Health Plan (DSGHP), 9/1/2018 Page 1 of 64
Dartmouth Student Group Health Plan (DSGHP) Plan Document 2019 - Effective Date: September 1, 2018 8 201 Mailing Address: 7 Rope Ferry Rd, HB# 6143 Hanover, NH 03755-1421 Physical Address: 37 Dewey Field Rd, 4th Floor Email: Dartmouth.Student.Health [email protected] Phone: (603) 646-9438 Fax: (603) 646-8893 For The Most Current Information Regarding The Photo: B. Murray Plan, Notices & General Information, Refer To The IMPORTANT INFORMATION DSGHP Website THIS DOCUMENT REFLECTS THE KNOWN REQUIREMENTS FOR COMPLIANCE dartgo.org/studentinsurance UNDER THE AFFORDABLE CARE ACT AS PASSED ON MARCH 23, 2010. AS ADDITIONAL GUIDANCE IS FORTHCOMING FROM THE US DEPARTMENT OF HEALTH AND HUMAN SERVICES, AND THE NEW HAMPSHIRE INSURANCE DEPARTMENT, THOSE CHANGES WILL BE INCORPORATED INTO THE HEALTH INSURANCE DOCUMENT. Dartmouth Student Group Health Plan (DSGHP), 9/1/2018 Page 1 of 64 TABLE OF CONTENTS Introduction .................................................................................................................................................................................................................................. 3 DSGHP Coverage & The Affordable Care Eligibility & Participation.......................................................................................................................................................................................................... 4-5 Enrollments ..............................................................................................................................................................................................................................