Medication Reconciliation: Issues Identified when Collecting Baseline Data
Updated – November 9, 2005
Goal: complete a Best Possible Medication History (BPMH) within 24 hours after the patient has been admitted to the unit.1
The Safer Healthcare Now! Campaign has outlined three types of discrepancies:
Intentional Discrepancies Where the physician has made an intentional choice to add, change the dose or route or discontinue a medication and their choice is clearly documented. Documented intentional discrepancies are considered best practice in medication reconciliation.
Undocumented Intentional Discrepancies The physician has made an intentional choice to add, change the dose or route or discontinue a medication but this choice is not clearly documented. Undocumented intentional discrepancies are not medication errors and do not usually represent a serious threat to patient safety however, they lead to confusion, rework and may lead to errors. This category of discrepancies account for 25-75% of all discrepancies.2
Unintentional Discrepancy An unintentional discrepancy is one in which the physician unintentionally changed the dose or route, added or omitted a medication the patient was taking prior to admission. These are medication errors and can lead to adverse drug events (ADEs).
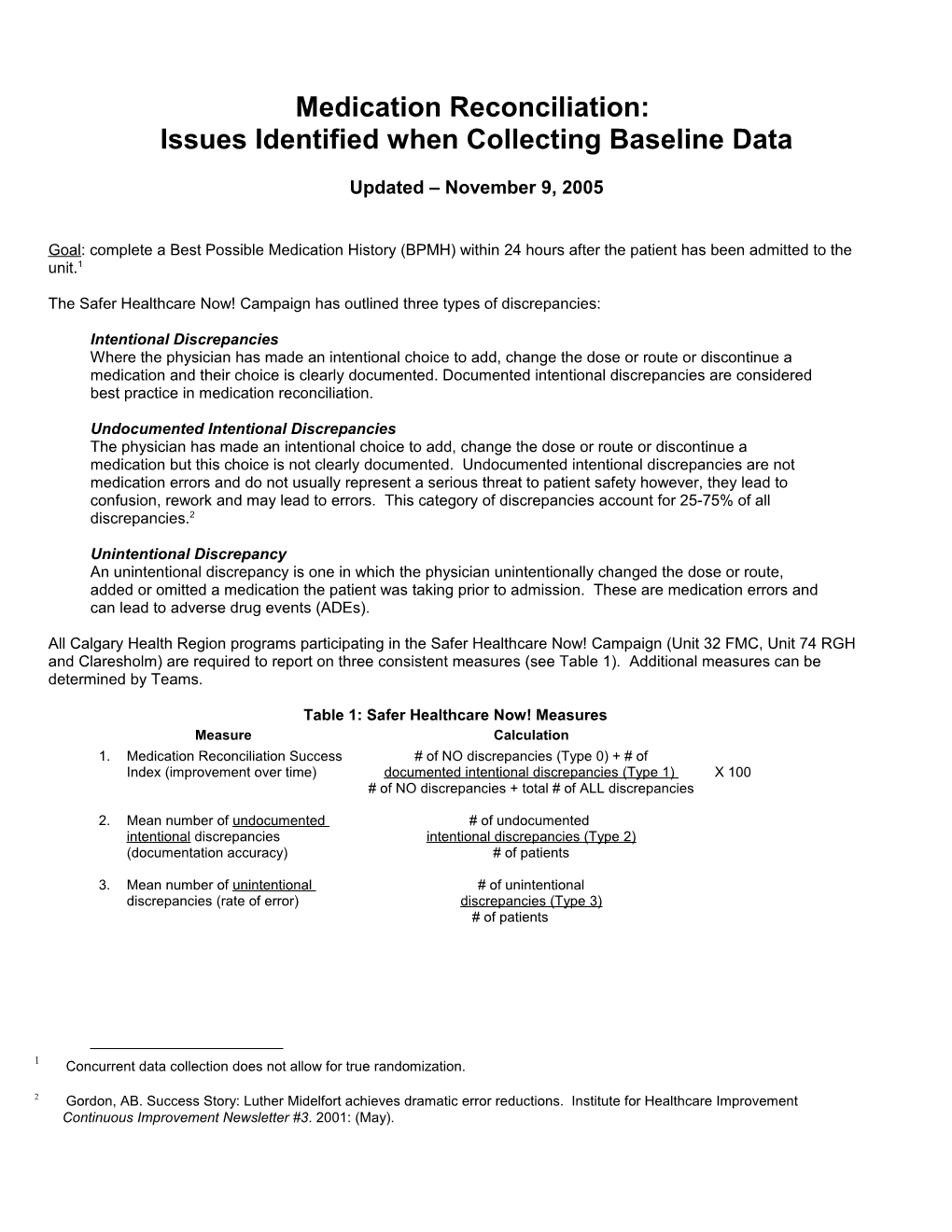
All Calgary Health Region programs participating in the Safer Healthcare Now! Campaign (Unit 32 FMC, Unit 74 RGH and Claresholm) are required to report on three consistent measures (see Table 1). Additional measures can be determined by Teams.
Table 1: Safer Healthcare Now! Measures Measure Calculation 1. Medication Reconciliation Success # of NO discrepancies (Type 0) + # of Index (improvement over time) documented intentional discrepancies (Type 1) X 100 # of NO discrepancies + total # of ALL discrepancies
2. Mean number of undocumented # of undocumented intentional discrepancies intentional discrepancies (Type 2) (documentation accuracy) # of patients
3. Mean number of unintentional # of unintentional discrepancies (rate of error) discrepancies (Type 3) # of patients
1 Concurrent data collection does not allow for true randomization.
2 Gordon, AB. Success Story: Luther Midelfort achieves dramatic error reductions. Institute for Healthcare Improvement Continuous Improvement Newsletter #3. 2001: (May). In the process of collecting baseline data a number of issues were identified. These issues were compiled and brought to the Regional Medication Reconciliation Working Group for discussion. Suggestions are provided for each of these issues to create a common approach/strategy for data gathering among all pilots.
Issues Identified During Data Collection Suggested Solution Dosing times are different (although the total dose is the Code as determined appropriate: same). This dose time change can impact patient care. - intentional discrepancy if the Physician documents the reason for the change Examples include: - undocumented intentional discrepancy if the physician is aware of the patient - medication given in a.m. vs. p.m. (e.g. nitrates, taking the medication at a specific time however, changes the administration time nitro-glycerine patches and cholesterol medication) without documentation - medication given at specific times (e.g. - unintentional discrepancy if the physician is unaware of when the patient takes Sinemet) the medication
Route of administration is different for clinical reasons Code as no discrepancy. related to admission (e.g. Lasix PO at home, has CHF exacerbation and Physician changes to IV).
Clinically obvious discrepancy, however not documented. Code as an undocumented intentional discrepancy. Examples include: - warfarin changed based on INR Rationale: reasons for the discrepancy should be documented and easily accessed - insulin changed based on blood sugar to avoid rework and increase efficiency (e.g. staff searching for information in - nothing orally (NPO) for GI bleeds where medications charts). Also, clinically obvious to one clinician may not be obvious to other or new are held with the typical exception of BP medications clinicians. - dose inhaler to nebs due to acute illness This strategy can be communicated by saying “For the purposes of this study we are tracking all discrepancies. Undocumented intentional discrepancies include those that seem clinically obvious. Our aim is to reduce these by 75%. In order to do that we are requesting that all discrepancies, including those that may be viewed as clinically obvious, be documented upfront. We recognize that this process may involve additional work and some duplication in order to gain efficiencies.” Over the Counter (OTC) medications (e.g. Vit D, calcium, Code as determined appropriate: aspirin, folic acid, motrin, etc.) are not accounted for while - intentional discrepancy if the physician documents the reason for the in an acute facility. discrepancy - undocumented intentional discrepancy if these medications are taken regularly OTC medications are expected to be documented in the and are on the agreed upon Regional list of OTCs medication list if the patient takes them on a regular basis - unintentional discrepancy if the physician is not aware of the patient using the or are specifically prescribed by a physician OTC Rationale: Patients may leave hospital with the assumption/impression that they are no longer meant to take these medications. As well, there is a need for consistent messaging with public health, family medicine and other health care professionals. Some OTC medications may have drug interaction potential. Discrepancy is caught by the Pharmacist in the If written in an order by the Physician on admission orders to the Unit then yes, code Dispensary. (e.g. Ritalin ordered vs. Rispiradone. as determined appropriate (e.g. undocumented intentional or unintentional) Pharmacist recognized ordered dose (20 mg) as much If written in an order in the Emergency Department then do not include. higher than typical (6 mg) and discovered wrong medication was ordered) Combination Medications. Examples include: If the order is correct for both of the combination medications then code as no - Blood pressure medication and diuretic discrepancy. Count as one ‘no discrepancy’ only. - Calcium and Vitamin D If the order is incorrect for either or both of the combination medications then there is a discrepancy. Code as determined appropriate (e.g. intentional, undocumented intentional or unintentional) and count as one ‘discrepancy’ only. Vitamin B12 (typically 1x/mo) – normally not ordered or Code as determined appropriate by speaking to the physician as to awareness of documented because of length of stay B12: - undocumented intentional if physician is aware of B12 usage and not ordered - unintentional if physician is not aware of B12 usage Rationale: The admitting physician should document all medication and indicate when the medication is due Unit 32: Hospitalists also have a Family Practice and As this is a typical scenario the patients data should be included in the data. sometimes see their patients in hospital. In these situations there are few, if any, discrepancies. Should we include these in the sample?